The tl;dr Pharmacy Journal Club: Fish Oil for Cardiovascular Risk Reduction in Hemodialysis Patients
FDR may not be giving this particular fireside chat, but we hope you’ll find it just as interesting.
Steph’s Note: It’s back! We haven’t don’t a journal club in (*cough*) quite a while, so we figured it was a good time to revisit our old friend. Who doesn’t love a good fireside chat about studies and statistics? We know we do!
This journal club is brought to you by our own Jenny Hoang, who previously taught us about Aucatzyl and CAR-T as well as herbals. Thanks, Jenny!
Happy New Year to all! While it may be Aquarius season, today we will be diving into the depths of hemodialysis and cardiovascular disease with the PISCES trial, which was published in NEJM in November 2025. In this journal club, we will learn whether fish oil supplementation has the potential to improve the heart health of hemodialysis patients.
But first, let’s look at how cardiovascular disease affects hemodialysis patients, specifically.
Hemodialysis (HD) is used in patients with end stage renal disease (ESRD). These patients’ kidneys no longer work properly to filter waste in the body, so a machine is used for this job instead. Blood is pumped out of a patient into a dialysis machine, where it encounters dialysate fluid. This fluid draws out the waste through a combination of diffusion and convection, and the “scrubbed” blood is then reinfused back into the patient.
For a more thorough discussion of hemodialysis mechanics, check out this post.
Pretty neat, right? However, there are MANY risks associated with performing hemodialysis, including infection, high or low blood pressure, fluid overload, anemia, and electrolyte imbalances - just to name a few. To make things worse, these issues can also lead to secondary cardiovascular changes that can cause unwanted cardiovascular disease (CVD). In fact, more than half of ESRD patients die from CVD. Yet despite their mortality being nearly 20 times higher than the average population, there are few proven medication interventions to prevent CVD events.
With such high risks and few interventions, the purpose of the PISCES trial was to see if fish oil supplementation could lower the rates of CVD in HD patients. Fish oils and the fatty acids they contain have been studied in research for many years, with significant findings in their ability to help reduce risk of CVD in the general population. In the PISCES trial, the authors highlight that many HD patients tend to have a lower amount of fatty acids in their blood. So they decided to see if giving some extra would produce protective heart benefits.
Methods of the PISCES Trial
Now let’s move on to how this trial was set up. It was a double-blind, randomized, placebo-controlled trial conducted at 26 sites in Canada and Australia. Patients on maintenance HD were to take either daily fish oil or a corn oil placebo.
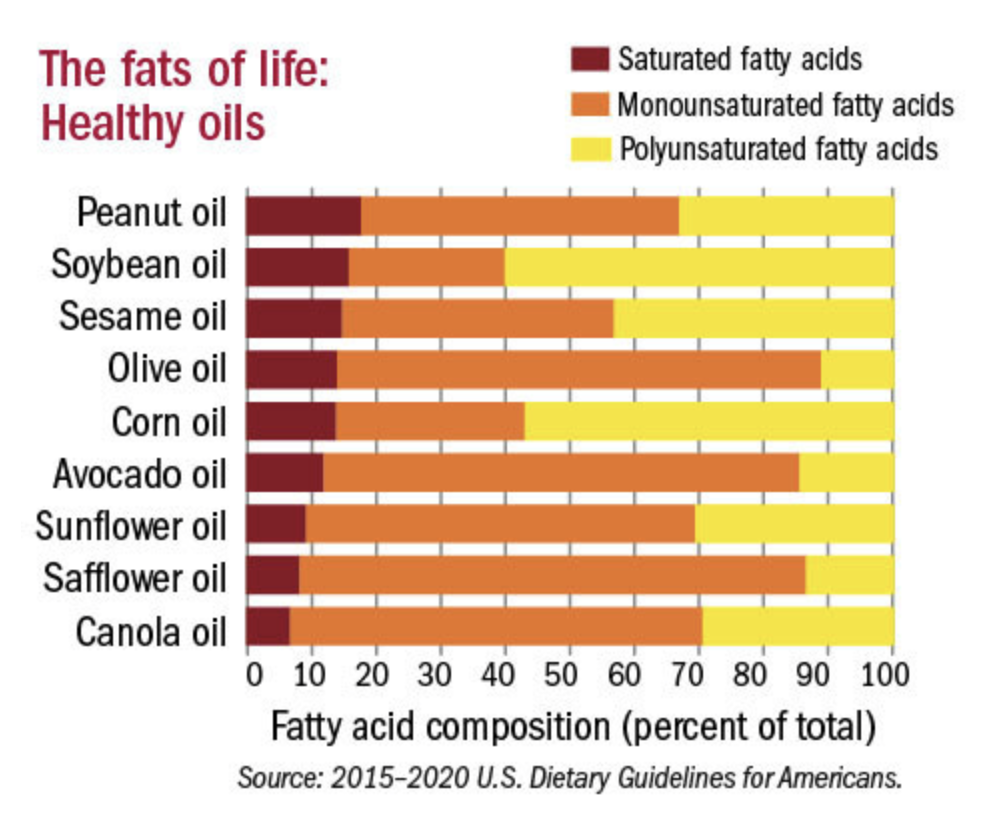
Corn oil, you say? Is that really an inert placebo, or would that be bad for the heart (making any other intervention look good by default)??
Just another glimpse into why corn oil probably isn’t as bad as some people think it is. Not all oils are created equally!
Glad you asked. Because so did the American Heart Association. In this 2023 study that compared potential atherogenic effects of various oils, including corn and mineral oils, corn oil did not appear to contribute to LDL oxidation (and subsequent atherogenesis). This means it doesn’t appear to be a harmful oil and should be an appropriate placebo. (Image)
In PISCES, the fish oil dose was 4 g of n−3 polyunsaturated fatty acids, which is equivalent to 1.6 g of EPA and 0.8 g of DHA. Simply put, the body needs omega fatty acids to help the cells function properly in the body. EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are fatty acids commonly found in fish. According to studies from the American Heart Association, consuming about 3 g of omega 3s in a day can help lower blood pressure, thereby helping to prevent CVD. So it makes sense that the researchers in the PISCES trial picked 4 g of fish oil as their intervention since it is just around the previously studied dose found to have CVD benefit. It’s just a tad more to account for what we mentioned earlier - that HD patients tend to be a little deficient at baseline.
Breaking down the double blinded and randomized part, it means that both the patients and the researchers were unaware of who was given fish oil or placebo. The randomization was done by an independent, web-based system, meaning a computer generator helped assign the groups to eliminate human error or accidental bias. The benefit of this is that both parties are less prone to any bias that may occur if they believe the patient is or is not receiving the fish oil. Randomization helps to give the study the best chance at capturing a realistic distribution of variables.
The placebo control allows the researchers to ensure that any treatment effect observed is due to the intervention rather than other factors. The researchers tried their best to control how similar the patients were in the experimental and control groups at baseline, and patients in both groups were measured and studied in the same ways over the follow up period to prevent any biases or errors that could skew their results. All of these things are very reassuring for the accuracy of the study.
At least the participants didn’t have to feel like this guy… not everyone is lucky enough to have deodorized, flavored fish oil capsules.
The patients were assigned 1:1 for fish oil or corn oil placebo. Both were deodorized and citrus flavored to taste and perform similarly when taken by the participants. (Image) The participants signed written consent to be followed and have data collected for a year, and then they checked in after an additional 2.5 years.
Inclusion/Exclusion Criteria of the PISCES Trial
Eligible participants were at least 18 years old and had ESRD managed with HD 3 to 4 times a week. They also had to be considered clinically stable before enrollment, so no active bleeds, blood pressures over 180/120, or life expectancy less than 6 months (palliative dialysis patients).
Any patients who were already taking any fatty acid or omega supplements prior to randomization or had any allergies to fish, soy, corn, or any other materials in the study were excluded. This tells us that the researchers were trying to isolate any effect from the study intervention rather than muddying the waters with confounding previous treatments.
PISCES Study End Points
For their primary end points, they looked at a composite of all serious cardiovascular events, including cardiovascular related deaths (e.g., sudden/non sudden cardiac death, fatal myocardial infarctions/heart attacks, and fatal strokes) as well as non fatal cardiovascular events (including non fatal myocardial infarctions/heart attacks, non fatal strokes, or peripheral vascular diseases that led to amputations).
They chose not to include heart failure as an endpoint. This makes sense because HD patients have many other non cardiac related factors that contribute to and cause fluid overload.
Overall, this seems like a very reasonable primary end point because they were hoping to see if there is a connection between the patients taking the fish oils and any and all cardiovascular disease.
For the secondary endpoints, they chose to elaborate on the primary ones:
Non cardiac causes of death,
Individual components of the primary end point (meaning that while the primary end point tallied up all the events, in the secondary endpoints, they decided to separately tally them up so we could see how many of each event happened), and
First cardiovascular event or death from any cause (meaning they measured the time it took for any patient to have a cardiovascular event, regardless of what caused it).
So overall, these secondary end points make a lot of sense because they wanted to dive a little deeper into whether the fish oils affected mortality. These endpoints also are a window into whether there were any patterns of what type of cardiac events happened in connection with fish oil. And they help to illuminate time to benefit (IF it was effective at all).
Analytic Strategies in the PISCES Trial
A little bit on how these end points were analyzed. The intention to treat principle was used. As a reminder, this means that the results of the trial were computed based on the patients’ original treatment assignments and study protocol, not what actually happened. So even if a patient didn’t go through with the entire protocol as designed (e.g., drop out), they would still be included in the data analysis.
The Cox proportional hazard model was used. This statistical model is used to assess how different variables affect the risk of an event happening over a period of time. This makes sense for this study’s endpoints because they were looking to see what factors influenced the occurrence of cardiovascular events during the trial. The standard Cox model does not reset time to zero after each event, meaning the risk is assumed to be constant over time.
On top of that, the Prentice-Williams-Peterson (PWP) gap time model was used. This is an extension of the Cox model. It looks at the same subjects but also assesses whether they experience events more than once and in what order. The gap time part means that they reset the time to event clock to the very beginning after each event (unlike the standard Cox model), allowing for a new assessment of risk after each new event.
The calculations were done from a sample of 1100 participants followed over at least 3.5 years. They provided the trial with a 82% power at an alpha level of 0.05. These values are pretty standard in the research world - for a more detailed look at power and alpha levels, check out our biostatistics series here.
The study designers targeted a hazard ratio of 0.825, meaning that they expected a 17.5% risk reduction in patients who took the fish oils. (1-0.825=0.175) They also assumed baseline event rates as follows:
recurrent cardiovascular event 0.74 times per 1000 patient days,
0.12 cardiovascular deaths per 1000 patient days, and
0.27 non cardiovascular deaths per 1000 patient days.
They also assumed 10% of the participants would be lost to follow up and 3% would drop out.
These numbers are important to assess because these baseline assumptions shape the remaining study design, including how many participants they think they’ll need to reveal a difference between groups. If these calculations are off because the baseline assumptions aren’t real world, then it’s possible a treatment’s impact can be missed. Which would be a shame after all the time, effort, and money that go into running a study!
Results of the PISCES Trial
And on to our favorite part of a journal club…the results!
Here’s a little bit on the baseline characteristics of the bunch. The mean age was 64.3 +/- 13.7 years old. They were on HD for a mean duration of 3.7 +/- 4.1 years, and 35.3% of the participants had a history of cardiovascular disease.
Moving on to the primary endpoint, the rate of all serious cardiovascular events was lower in the fish oil group (0.31 per 1000 patient days) than the placebo group (0.61 per 1000 patient days) with a hazard ratio of 0.57 (95% confidence interval 0.47 to 0.70, p<0.001). So that means there was an estimated 43% reduction in risk of cardiovascular events in the fish oil group compared to the placebo. That’s pretty good! (And much better than their target 17.5% reduction!)
Additionally, the percent of patients with at least one cardiovascular event was lower in the fish oil group (20.8%) vs the placebo group (33.7%).
The PISCES researchers, when they did their results calculations and compared to their original estimates.
The researchers also noted that these lower rates of cardiovascular events with the fish oil group were similar between those with or without a history of cardiovascular events. That really highlights how the fish oil intervention was helpful to anyone on hemodialysis.
16.6% of patients in the fish oil group vs 23.1% of patients in the placebo group had only one serious cardiovascular event, while 4.3% of fish oil patients and 10.5% of placebo patients had recurrent events. As you can see, the fish oil won in preventing the first and only serious event, but it pretty much halved the number of patients experiencing recurring ones. Pretty impressive if you ask me. (Image)
Now it’s time for the secondary endpoints. When they accounted for the primary endpoint and non cardiac causes of death, the hazard ratio was 0.77 (95% confidence interval 0.65 to 0.90). This means there was a 23% reduction in risk of death (cardiac or otherwise) if taking fish oil! The occurrence of at least one component of the primary end point was found to be lower in the fish oil group (35.2%) than the placebo group (43.7%). The percent of patients with heart failure was 1.6% for the fish oil group and 2.3% for the placebo group with 8.5% and 9.9% needing cardiovascular intervention, respectively.
All of these numbers sure do paint fish oil in a pretty positive light.
And when we flip the coin and look at safety, serious bleeding occurred in 4.8% of fish oil patients vs 7.6% in the placebo group. So it’s not like there was even a trade off there. Usually you can’t have your cake and eat it too, but…maybe we can in the case of fish oil.
A Few Additional Thoughts on the PISCES Trial
In this study, it looked like fish oils really did help in lowering the rate of serious cardiovascular events in HD patients, both with or without a history of cardiovascular disease. The researchers measured the patients’ phospholipid concentrations before and after the trial and found increased concentrations afterwards.
These may have contributed to antithrombotic, antiinflammatory, antilipid, antiarrhythmic, and remodeling effects in the cardiovascular system…all good things that the patients could benefit from. While this trial was only able to enroll patients on maintenance HD, it shows promise for future research and development into cardiovascular interventions in this patient population.
The tl;dr of the PISCES Trial
Patients on HD have lower levels of fatty acids. There are few interventions for CVD prevention in patients on HD even though these patients are at high risk of CVD. Fish oil supplementation may lower HD patients’ risk of cardiovascular events and death. The increase in phospholipid concentration may be the key to the reduction in cardiovascular risks. More research can and will be done to develop cardiovascular interventions for HD patients.