Vancomycin Dosing in Hemodialysis
Yes, I know it’s been a hot minute. Or a couple hot years. But it’s time. We are FINALLY going to talk about vancomycin dosing in hemodialysis!
When I was a PY4 on rotation, the thought of having to dose vancomycin in hemodialysis (HD) literally used to terrify me, and I used to pray that my patients wouldn’t be on HD. But that’s because I didn’t understand dialysis. Now that I have a better understanding, it’s actually not so bad. I promise. Hopefully by the end of this post, you’ll feel better about it too!
For a review of pharmacokinetics and vancomycin dosing in the general population, please revisit Pharmacokinetics: Dosing Wars and The Complete (but Practical) Guide to Vancomycin Dosing. We’re going to build on a lot of these concepts, so you may want to make sure you’ve read and understand the “normal” population before veering into the realm of kidney dysfunction.
If you’ve got that part down pat though, buckle up - because here we go on HD!
So you’re feeling pretty good. You’ve dosed a few vancomycins in your patients, gotten a couple of levels back, and adjusted the dose based on those levels. You’re riding pretty high on your successful use of population kinetics to get these people going. And you should feel proud - that’s a heck of an achievement!
But of course there’s a curveball. (There always is. Why else would we have tl;dr!?!)
The next septic patient on your service happens to also have End Stage Renal Disease (ESRD) and typically receives hemodialysis three days a week. Harking back to your previous vanc knowledge, you KNOW that renal dysfunction will affect the patient’s clearance of vancomycin…
But what do you do about it? How do you, the pharmacist, manage it? Because you can bet that YOU are who the team is relying on to manage this.
Before we go too far down the road of kidney disease, let’s have a minute to review some big points about vancomycin kinetics:
Vancomycin distributes pretty darn well throughout the body. Population kinetics estimates a volume of distribution (Vd) of ~0.7 L/kg.
Because of this distribution, we dose vancomycin based on total (actual) body weight in non-obese patients. In obese patients, consider use of adjusted body weight instead and/or lowering the Vd estimate (0.5-0.6 L/kg).
Vancomycin is cleared via the kidneys. Cockcroft-Gault’s estimation of CrCl can be used to estimate the elimination rate constant (Ke) by the equation Ke = 0.00083*(CrCl) + 0.0044. Ke can then be used to estimate the half-life of the medication: t1/2 = 0.693/Ke.
In a patient with consistent renal function, repeated dosing of vancomycin eventually leads to steady state, where the peak and trough concentrations are similar from dose to dose. Remember:
But then what about our ESRD patient on HD three times a week?
In this scenario, you basically have to think about HD as replacing the patient’s kidneys. At least partially.
What is Hemodialysis?
Without properly functioning kidneys, patients with chronic kidney disease accumulate waste and toxins, not to mention they can experience dangerous electrolyte imbalances. To clear out that waste and to rebalance electrolytes, HD removes a patient’s blood from the body, runs it through a machine, and then infuses the “scrubbed” blood back into the patient.
The HD machine (which is basically a fancy filter) is where the magic happens.
Within the HD machine, there are tubes containing semi-permeable membranes. Bags of fluid called dialysate are introduced to one side of these semi-permeable membranes.
Dialysate fluid typically consists of water, electrolytes, and glucose in varying concentrations. Choice of dialysate depends on a patient’s specific needs for waste/toxin removal and electrolyte rebalancing. (Luckily nephrologists make the determination of which dialysate to use!)
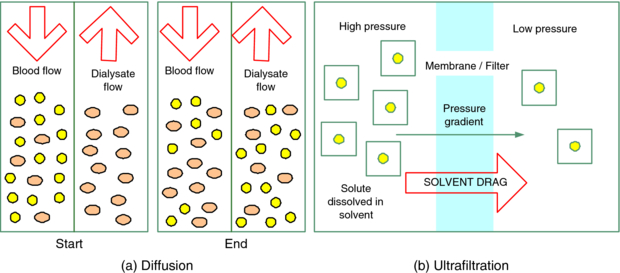
When the patient’s blood is removed from the body, it is introduced to the opposite side of the semi-permeable membrane in the tubes. And buh-BAM! Diffusion occurs across the semi-permeable membrane due to the gradient created between the patient’s blood and the dialysate.
Recall from basic biology: in diffusion, solutes move from areas of higher concentration to lower concentration in a passive process! So the blood that is rich in waste and toxins will lose those junk to the clean dialysate that is just waiting to accept those molecules. And any electrolytes that are out of balance in the blood can be rebalanced by using the right mix of dialysate to create a diffusion gradient.
Pretty nifty, right?
Modern HD also often incorporates a component of convection as well as diffusion. Convection, which uses a pressure gradient to move larger molecules, can also help to clear the patient’s blood of unwanted solutes. Furthermore, it can be used to remove excess fluid (or water) as ESRD patients often have a component of fluid overload since they make little to no urine. The use of convection to remove larger solutes and fluid is called ultrafiltration.
To compare the processes of diffusion and convection/ultrafiltration:
Important: note how diffusion is a two-directional/passive process whereas ultrafiltration is a one-directional/active process. (Image)
HD can also be classified as low-flux or high-flux. This categorization is based on the permeability of the membrane used. These days, most HD is considered to be high-flux, meaning a higher permeability membrane is used that allows passage of larger solutes and molecules.
How well HD works to cleanse a patient’s blood depends on a number of factors:
Duration of treatment affects solute clearance. The longer a patient is dialyzed, the more time there is for waste and toxins to be removed.
Blood flow rate is another factor to consider. The more blood entering the cleansing system, the more there is available to scrub.
Along the same lines as #2, the dialysate flow rate can affect clearance of solutes. If you don’t introduce sufficient “clean” gradient, you may not pull off as much solute as desired.
The membrane surface utilized - as above low versus high-flux membranes and the varying degrees of permeability to solutes.
In general, HD is a pretty exhausting procedure, especially when each session is usually 3-4 hours on three days each week. You can imagine that, depending on how quickly blood is removed from the body, patients can experience dramatic drops/swings in blood pressure. They often feel tired and nauseated, and sometimes they are unable to complete the entire session as planned. (Important: log this away!)
Think about it. You’re taking someone’s entire blood supply out of their body, and then putting it back in. It’s exhausting. Not exactly something people look forward to.
For those visual people, here’s HD in a nutshell:
A schematic of the HD process (only diffusion is illustrated here). (Image)
What HD looks like in real life. Pretty intense! (Image)
Effects of Hemodialysis on Vancomycin Kinetics
So now that we know a little more about the process of dialysis, we need to talk about how it fits with vancomycin.
With modern high-flux HD, a good general rule of thumb is that approximately 30-50% of a patient’s vancomycin will be removed with each HD session. What happens in between HD sessions is dependent upon a patient’s residual kidney function.
What? But the patient is on HD! What do you mean residual kidney function??
Some dialysis patients still have some modicum of urine production, which means they may clear some small amount of vancomycin in between dialysis sessions. Other dialysis patients are completely anuric, meaning they do not make any urine at all.
For anuric patients, assume that any vancomycin left in their system after HD will still be there until their next dialysis session.
Why is all of this important?
The time vs concentration curve, my friends! In HD patients, you can figure their curve looks a little more like this:
Hey, no judgment zone, ok? For drawing in Paint on a laptop without a mouse, I’m calling it a win!
To break down this (obviously beautifully crafted) graph, you give an HD patient his first dose in hopes that where you land concentration-wise after filling the tank is at a therapeutic level of (hopefully/usually) 15-20 mcg/mL.
This first dose can be treated just like an initial dose in a patient with normal renal function. Generally, we’re looking at 15-20 mg/kg of your chosen dosing weight.
You and I when we ASSume just a smidge too much. (Image)
Now most of the time, are you going to hit that nail exactly on the head and give just the right amount on the first try?
Proooobably not. Maybe…but not likely.
Think of all those assumptions we make about Vd and which weight to use. It’s a veritable minefield of assumptions! And we all know what happens when we assume…
One can have #lifegoals though.
Regardless, then the patient has their first HD session (left red arrow), and somewhere between 30-50% of that first dose is removed (Gosh, not cool!).
We need to get that patient’s serum level back into the therapeutic range. So you recognize you need to give the patient some sort of supplemental vancomycin dose after HD. That second dose will then largely stay at a consistent concentration until the patient has HD again (middle red arrow). And so on.
So what are the different colored curves?
Starting with purple, this is representative of a patient who is completely anuric. You can see how after each dose, the patient’s serum vancomycin concentration stays pretty much constant. This patient is not clearing any vancomycin on his own. Then HD comes along and draws off 30 - 50% of drug, forcing you (the pharmacist) to figure out how much you need to give back to get his serum concentrations back in therapeutic range.
Then if we look at the blue curve, this is representative of a patient who still has some residual urine output. In between HD sessions, his vancomycin level drifts downward…but only slightly. Certainly not as much as the normal vancomycin time vs concentration curve, but it does mean that you (the pharmacist) may have to give a wee bit more vanc supplementation after HD to get him back in therapeutic concentration range.
So what exactly qualifies as significant residual urine output in someone on HD? What number may actually make you think you need to give a little extra supplementation?
Unfortunately, that’s not a black and white number… But in general, if patients are producing more than 400-500 mL in 24 hours even while on HD, that’s probably sufficient enough to consider needing a little extra vancomycin supplementation after HD.
Long story short, your mission (should you choose to accept it) is to figure out how much vancomycin to give a patient after each HD session to keep their levels in therapeutic range.
Well how on earth are you supposed to do that?
Checking Serum Vancomycin Levels before Hemodialysis
Luckily, we can check serum levels to help us!
But when should we check? Before HD? After HD? Both?
Usually the easiest and most straightforward method is to check a vancomycin random level before HD (aka a “pre-HD random”). If you think conceptually about this concentration, it’s akin to checking a “trough” level in a normal patient.
NOTE: It is NOT a “trough” in the sense that it is the lowest serum concentration the patient will experience in the course of their therapy (because of course their levels are lower right after HD).
But rather, it’s a trough in the sense that the blood level right before dialysis is the therapeutically active drug concentration. It’s the concentration that the patient is exposed to for the majority of the time in between HD sessions. So if that’s not in therapeutic range, then we’re either not treating the infection, or we’re over-treating the infection.
And while some might argue that over treatment isn’t as big of a deal in ESRD patients (because “their kidneys don’t work anyway”…grrr), there are adverse effects to vancomycin outside of just nephrotoxicity! So even though levels slightly above 20 (say, 20-23) aren’t the absolute end of the world, it’s still not good practice to leave a patient with preHD levels much greater than that.
Therefore, ideally, a pre-HD vancomycin random shouuuuld be between 15-20 mcg/mL for treatment of most infections. But in a practical world, the target pre-HD levels really end up being 15-25 mcg/mL.
Adding on to our previous time vs concentration HD curve, the green time points are representative of checking pre-HD random vancomycin concentrations. So you give a dose, generally let it hang out, and then check a random level right before a patient goes to dialysis. Now does it particularly matter whether that pre-HD level is 1, 2, or 3 hours before HD? Not really… because remember, these patients aren’t really clearing much on their own, if at all. So a 6 am check shouldn’t really be much different than an 8 am check, as long as the check is before HD starts.
When and how often should these pre-HD levels be checked?
Well that’s a loaded question.
Unquestionably, however, a pre-HD level should definitely be checked after you’ve given your first dose and before the next session of HD. This will tell you where you stand on filling the tank.
But…sometimes the interval between dose and pre-HD random can be quite long, opening up that gray area we like to call “clinical judgement.”
For example, a patient who normally receives HD on Monday, Wednesday, and Friday, comes into the emergency department on Saturday. He is admitted and receives his first dose of vancomycin on Saturday, but having just had HD on Friday, he is deemed stable enough to wait until his regularly scheduled next HD on Monday.
As the dosing expert, should you wait all the way until Monday morning to check a pre-HD level?
That really depends on how stable your patient is. Are you willing to gamble and run the risk of potentially under-treating with sub therapeutic levels for potentially 36-48 hours? If not, maybe you check a random level with Sunday morning labs just to see where you are after your chosen estimated first dose.
Perhaps you need to give a supplemental dose even without the patient having HD on Sunday if you’ve completely undershot and get a morning random of 9 mg/dL. (That might explain his continued fevers even after getting a dose… let’s give him a little extra vanc, please.)
More than likely, you will also need to check another pre-HD random after giving your second dose, before the next HD session. This will tell you how well you did with your chosen supplemental vancomycin dose.
I know, I know. "Depends” isn’t exactly what you want to hear. But unfortunately, it’s hard to get much more black and white than this when it comes to dosing vancomycin in HD.
After the first couple of levels and HD sessions, the continued frequency of level checks depends.
Is the patient on a stable HD regimen?
Is he tolerating full and regular sessions of HD, or did the last one get cut short due to low blood pressures?
Did the nephrologist order an extra session with ultrafiltration because the patient’s declining respiratory status was thought to be due to some fluid overload?
These are the types of situations that make dosing in HD more complicated. And they’re also the scenarios that force us to check more frequent pre-HD random vancomycin levels.
In the ideal situation of a patient tolerating full, regularly scheduled, 3 times a week HD sessions, perhaps you only need to check those initial two pre-HD randoms to help establish an adequate supplemental dose and then you can get by with checking weekly pre-HD randoms.
But let’s be honest. That kind of stability in an inpatient setting is a rare unicorn.
More than likely, you will need to monitor the HD schedule, whether or not sessions are tolerated and fully completed, any extra ordered sessions, any changes in type of dialysis ordered (HD vs plain ultrafiltration), etc. Which will then force you to need to check more frequent levels.
But again, one can hope for stability!
So that’s the happy pre-HD vancomycin random story. But there’s another side. (I won’t say the dark side… even though y’all know I like Star Wars.)
Checking Serum Vancomycin Levels after Hemodialysis
We need to talk about post-HD vancomycin levels. Aka, levels drawn after HD sessions.
These levels are a little trickier. And the reason for that has to do with how dialysis affects drug distribution. When you give a dose of vancomycin, we’ve already established that it distributes pretty well. So with some time after a dose, the drug reaches a happy equilibrium between blood and tissues. Then, with a session of dialysis, we go and mess up that equilibrium!
We’re forcefully removing and scrubbing a patient’s blood of toxins, including vancomycin, during each session. When the resulting “clean” blood is re-infused into a patient, there’s a new vancomycin gradient created between blood and tissue. The blood (relatively) suddenly has a much lower concentration of vancomycin after being dialyzed, but the tissues are still harboring vancomycin.
So if we check a random vancomycin level immediately after the end of dialysis, it’s going to look low. Very low. FALSELY LOW. But given some time to re-equilibrate between blood and tissue, that serum vancomycin level is going to rebound, at least to some degree.
The key point here is this: if you’re going to check a post-HD vancomycin level, you have to allow for re-equilibration (aka redistribution) after the dialysis session. How long should you wait? Generally, most people wait 4-6 hours after the end of dialysis before checking post-HD vancomycin levels to avoid falsely low results.
What should a post-HD vancomycin level be? Let’s go back to this thought: whatever that level is after HD, it’s likely to stay at that general level until either more drug is added or the patient is dialyzed again. So as long as that post-HD level is at least 15 (for most indications), there’s really no need to redose after HD.
But always consider your indication - maybe it’s cellulitis and you can scrape by with a 13.5…
The exception to this is if your HD patient still has significant residual urine output, where a post-HD level of 15 may not last them until their next level check in 2 days because they may clear enough on their own to drop to <15. In that case, depending on indication, maybe you need to give a smidge of a supplemental dose.
Now let’s have a practical moment about the utility of post-HD levels.
You know a patient is on a MWF HD schedule, and you see the patient’s order for HD today. But what time are they actually transferring to the Renal Unit for HD? How are you going to know whether or not they tolerated their full HD session as planned when the HD nurse’s note may not be entered until much later today?
So actually entering and timing an order for a post-HD level can require more legwork on your part to find out these pieces. Definitely not impossible…just not ideal when you have 30 other patients needing your attention! The easiest way to get this information is to develop a good working relationship with the nurses (and everyone else) on the team you’re working with.
That being said, there ARE times when it may be necessary to check a post-HD level. For example, it’s 8 am on Tuesday. Your patient is normally on a MWF HD schedule, and he received his HD and post-HD vancomycin dose yesterday afternoon as planned. It was beautiful, and all went according to plan. Win!
But SURPRISE! His labs from this morning just returned with a potassium of 6.5, and he’s short of breath and edematous. Guess what - he’s having an extra session of HD today. By the time you find this out, they’re literally rolling him down the hall. There’s no time to get phlebotomy up here to draw a pre-HD level.
So you’re stuck. You’re going to need that post-HD level, which means you have some legwork ahead of you to track the patient’s HD progress throughout the day to ensure the level is timed and drawn in a meaningful way.
To sum up vancomycin levels in HD, most of the time pre-HD levels are best and you prioritize checking these. Occasionally, you may find use for post-HD levels, but if you do, be sure to allow adequate time for re-equilibration.
How often you check levels after establishing a good supplemental post-HD dosing regimen depends on the stability of the patient’s HD regimen.
Changing renal function can affect vancomycin steady state in a patient with normal kidneys. Accordingly, changing HD regimens will affect how much vanc a patient requires to maintain therapeutic levels.
Determining Vancomycin Supplemental Doses after Hemodialysis
Now that we’ve discussed what levels to check, how often to check them, and what we want them to be, we need to talk about what to do with them!
Disclaimer: there are many ways to skin this cat (ew, sorry for the phraseology, kitties), but I’m going to give you my approach first. Then I’ll briefly review another strategy that some people employ.
In general, if a patient doesn’t have significant residual urine output, here’s a VERY general scheme for re-dosing after HD based on pre-HD levels:
| Pre-HD Vancomycin Level | Supplemental Vancomycin Dose |
|---|---|
| < 10 mcg/mL | 1000 mg |
| 10-25 mcg/mL | 500-750 mg |
| > 25 mcg/mL | No dose needed |
Honestly, at the risk of sounding a little “one size fits all,” this is the dosing scheme that I prefer.
Of course, as always, this is with the HUGE CAVEAT that these doses may need to be tweaked based on each individual patient’s specific characteristics (residual urine output, weight, HD schedule and tolerance, etc.). But this is certainly a pretty good starting base for that supplemental, post-HD dose following the first load and first pre-HD level.
So let’s look at an example:
What? Of course a person who likes Star Wars can like LOTR too! (Image)
GtG is a 75 YOM with ESRD on HD MWF who is admitted from home on Sunday for osteomyelitis.
(This guy, he just can’t keep himself out of trouble…Recently, he was bitten by a warg. The wound got infected, the stubborn fool refused medical attention, and it has now progressed to his bone. He’s refusing an amputation, so we’re trying IV antibiotics instead.)
GtG is 6’ and 85 kg. How should we initiate GtG’s vancomycin?
This patient doesn’t appear to be anywhere near obese, but for practice, let’s run through it. His IBW is 78 kg. 85/78 = 1.09, so he is only 9% over his IBW. Definitely not obese. GtG’s vancomycin dosing weight will be his TBW.
FYI, he’s not particularly septic (vitals stable, afebrile). As such, we won’t be using aggressive loading doses of 25 mg/kg; instead, we’ll stick somewhere in the range of ~15-20 mg/kg. So his first dose comes to 1275 - 1700 mg. Let’s meet in the middle and use 1500mg (17.6 mg/kg).
GtG receives his first dose of vancomycin 1500mg x1 on Sunday afternoon. Per the nephrologist note, he completed his full session of outpatient HD on Friday, doesn’t have any indicators for urgent HD (AEIOU), and won’t be due for HD again until Monday AM.
You order a vancomycin random level with morning labs on Monday to see where he stands after his first dose. This will be his first pre-HD level.
On Monday morning, his pre-HD vancomycin level returns at 17 mcg/mL. Woot! We did pretty darn well with our first dose (he’s in the target 15-25 mcg/mL range)!
We follow up with the RN to ensure he makes it to HD on Monday as planned and that he tolerates his full 3.5h session this time. She reports positively on both counts. So what should we order for his supplemental post-HD vancomycin dose?
His pre-HD level was between 10 and 25 mcg/mL, so by our general scheme as above, we’re looking at 500-750 mg. Deciding between the 2… He doesn’t make any residual urine, and he’s smack dab in the middle of that 10-25 mcg/mL range. So, let’s give him the 500mg x1 supplemental dose after HD.
Suppose his pre-HD level was more like 11 instead of 17… Then I might consider giving him 750mg instead of 500 mg.
Let’s now suppose his pre-HD level was 17 but he also still makes 500-600mL of urine a day… That’s pretty significant! So whatever we give him, he’s going to work on clearing at least some on his own between Monday evening and his next HD on Wednesday. So I might err on the higher side and give him 750mg instead of 500mg.
So back to reality and not all these suppositions. We went with option #1 and gave him 500mg x1 after his Monday HD session. The nephrologist note states that they are planning to keep him on his normal MWF schedule with another session on Wednesday. He’s still stable and not showing any signs of sepsis. So we’ll plan to check another pre-HD level on Wednesday AM.
Keep searching for that unicorn named…Stability. (Image)
Wednesday morning’s labs return, and his pre-HD vancomycin level is 19 mcg/mL.
Still within our target range.
So as long as GtG’s HD schedule and tolerance remains the same, our 500mg supplemental vancomycin doses are appropriate.
As long as he stays stable and his HD regimen doesn’t change, we can get away with giving 500mg doses after HD and only checking pre-HD levels once per week instead of before each HD session.
That’s an example of best case scenario. Unfortunately, it almost never works out quite so smoothly. (Remember that unicorn?)
More than likely what happens is more like this:
The same patient is admitted on Saturday afternoon, and he is floridly septic (febrile to 103F, WBC 17, HR 106, BP 85/55). You quickly give him a first dose of vancomycin (although perhaps this time you err closer to 20mg/kg than the 17 mg/kg previously). The nephrologist note says that he is ok from a renal perspective to wait until his regularly scheduled Monday HD session.
So now you’ve given this loading dose of vancomycin to your septic patient, and per the pre-HD level scheme, you’ll be waiting…ohhhh…around 36 hours before checking a level before HD on Monday.
How does that sound? Do you feel like gambling with a long stretch of time in a septic patient?
Hopefully this idea doesn’t sit well with you. 36 hours is a long time to inadequately treat a septic patient!
Instead of waiting until Monday AM labs, you decide to check a level with Sunday AM labs. Good choice.
Your Sunday AM vancomycin random is woefully subtherapeutic at 10 mcg/mL.
Remember, your patient is going to sit at whatever level you’ve produced until he goes to HD (where it’s only going to get lower). So you produced a 10. We know we need levels of at least 15 in our septic patient (who, btw, was fevering all night).
We need to bump his serum levels! Sure, it’s not a supplemental post-HD dose we’re giving to replace what HD removed…but we’re doing a catch up dose all the same because we missed the mark with our first loading dose.
You order an additional 500mg vancomycin x1 for Sunday AM in order to bump his levels >15 mcg/mL.
He is still scheduled to go to HD on Monday AM. You will still need to know where he stands before his Monday HD session in order to know how much vancomycin to replace after HD. So you order a pre-HD vancomycin level for Monday AM.
Monday AM’s vancomycin level returns at 22 mcg/mL. Phew! It’s a good thing you gave him that supplemental dose on Sunday even without him having any HD because at least now you’re adequately covering him.
His vitals have stabilized enough in the last 24 hours that the team thinks he will tolerate his Monday HD session. And now it’s up to you to decide how much drug to order for after HD. He’s at the high end of the range, and he hasn’t made any urine since admission.
You order 500mg vanc after Monday’s HD, which the patient receives. Then you order a Wednesday AM pre-HD level in preparation for seeing how well you did with your 500mg supplemental dose choice.
You come into work on Tuesday, and you overhear the RNs giving report about GtG. He apparently has a potassium of 6.5 this morning, a new O2 requirement of 2L/min, and has some fluid overload. The nephrologist would like to take him back to HD again today rather than waiting until his regularly scheduled session on Wednesday.
Your patient, rolling down the hallway. (Image)
Oh whoops, there he is now, on his way to HD. There’s no way you can get a pre-HD level on him this morning!
You’re going to have to order a post-HD vancomycin level, which you do for 1600 this afternoon (at least 4-5 hours after the expected end of this catch up HD).
Unfortunately, at around noon, you ask the RN and find out that the patient wasn’t able to tolerate the full 3.5h HD session, and they had to stop after only 2 hours of HD. You retime your vancomycin level for a little earlier in the day, and follow up with it that afternoon.
Your post-HD vancomycin level returns at 18 mcg/mL. In this patient who doesn’t make any residual urine, what should you do?
Here’s where it’s VITAL to remember what kind of vancomycin level you’ve ordered!! This is a post-HD level, so because he doesn’t make any urine, GtG is going to remain largely at that same level until his next HD. How do you feel about him sitting at 18 mcg/mL?
Hopefully you feel fantastic! It’s at least 15 (and still between 15-20 mcg/mL)! We absolutely like this! He does not need a supplemental dose of vancomycin after this extra, partially tolerated Tuesday HD session.
(Contrast this with the scenario of getting a PRE-HD level of 18. In this case, 30-50% of that 18 is then subsequently going to be removed by HD, so you WOULD need to replace with some additional vancomycin.
CRUCIAL DIFFERENTIATION OF TYPE/TIMING OF LEVEL.)
From then on, it’s up to you to continue to follow GtG’s tolerance of and schedule for HD. Hopefully, he will return to a regular, more predictable schedule that allows you to use standard maintenance doses. But until that “steady state” HD occurs, you’re kinda stuck ordering and following levels.
So that’s my preferred approach.
Another Way to Dose Vancomycin after Hemodialysis (but Don’t Do It)
I promised a quick review of another approach that some people use, and just so that you recognize it when and if you see it, we’ll at least touch on it here. But for the record, no me gusta…(Spanish for “I don’t like it”…or something close).
Some people take the approach of giving the patient a big dose (like 15-20 mg/kg) every time their level indicates it’s time to re-dose, whether that’s a pre-HD <25 or a post-HD <15. Meaning the patient doesn’t get a smaller dose after each HD session as the strategy was in the previous section.
Instead, the patient gets a big ol’ dose on an infrequent basis and then HD hacks at it a little at a time. Then, once the serum level is indicative of redosing, the patient gets another big ol’ dose instead of just a nice widdle supplemental dose.
For you visual people:
More high quality artwork. Notice in this (non-preferred) HD dosing method, the patient experiences higher levels for longer until either their pre- or post-HD serum level is indicative of the need to redose.
Pros of this method: less frequent dosing, I guess? So maybe less labor-intensive when it comes to having to address levels around multiple subsequent HD sessions? I suppose?
Cons of this method: um, why expose a patient to such high, sometimes sustained, levels for days if you don’t have to? Vancomycin isn’t completely benign, even if a patient’s kidneys aren’t functioning… Cytopenias are possible, as well as ototoxicity, although the latter is usually in patients with other ototoxic meds.
I dunno, call me crazy, I just tend to be a fan of exposing patients to the lowest effective dose when possible. #pharmacistlife
Vancomycin, Hemodialysis, and Transitions of Care
My last thoughts about vancomycin dosing in HD patients have to do with transitions of care. It’s important to note that, just because you dose your patients one way while they’re in the hospital, it doesn’t mean they will be dosed the same once they leave.
One of my colleagues once described an HD appointment as a hair salon appointment: chair time is extremely valuable. So HD centers don’t like to run late or take more time than necessary to complete a patient’s session because their next patient is coming in for the next time slot.
What that means is this - in the hospital, we wait until the HD session is 100% complete before we administer that supplemental vancomycin dose afterwards. In the outpatient world, sometimes the vancomycin dose is started during the last hour of the HD session in order to get a head start on the infusion and save that valuable chair time.
What this means is that outpatient post-HD supplement vancomycin doses are usually larger than those given inpatient because the patient is dialyzing when the dose is started! So some of that dose is going to be removed.
What THIS means is (bottom line, I promise) that, if you ever call an HD center to find out what dose of vancomycin a patient has been receiving, you MUST also ask how they administer it in relation to the HD session.
The HD center may say, oh yeah, that patient gets vancomycin 1250mg after each HD session. And if you go and try to order the same thing in the hospital, where you don’t hang that bag until HD is finished, you will (likely) quickly realize the difference with your next pre-HD level!
You Made It!
Alright. PHEW. I think that about wraps it up. Hopefully this at least gives you a starting point and some conceptual understanding of why dosing vancomycin in HD isn’t as terrifying as it seems. The best thing you can do is follow as many HD vancomycin patients as possible to consider when to order levels, how to interpret the results, and then determine any supplemental doses.
Practice, PRACTICE, PRACTICE! And always bounce your ideas off of another pharmacist if you’re in question. We’re all playing in the same sandbox :)
Happy vancomycin dosing!