A Pharmacist's Introduction to CAR-T: Aucatzyl (obecabtagene autoleucel)
Steph’s Note: After a couple of weeks largely heavy in infectious diseases, we’re changing gears and heading back to oncology land. Whoa, before all you “I’ll never touch oncology” pharm phriends click off this page, hang tight for a hot second. Because the topic this week is just plain SO COOL. We all became interested in pharmacy for a reason, and for many of you, it may have started with an initial interest in your science classes. So for anyone who thought the lecture on gene editing, vectors, plasmids, and gene insertion sounded like a sci-fi movie, you should definitely read on. Reality does not disappoint!
Guiding us through this fiction turned reality is Dr. Jenny Hoang. You may remember her from her previous post on the CTCAE grading system. Take it away, Jenny!
How your brain feels when you start learning about hematologic malignancies. (Image)
Blood cancers. It would take us quite a bit of time to get into the intricacies of what they are (there are many), so I’ll leave that to this wonderful article. If you haven’t read that post yet, it may help you to check it out before diving into this one!
Instead we’re going to start with a story about a cancer survivor named Doug Olson.
Doug was diagnosed with chronic lymphocytic leukemia (CLL) in 1996. Over the next decade or so, he tried multiple treatments without much success for achieving control. Faced with limited options, he decided to join a clinical trial in 2010, in which they took a patient’s own blood cells and modified them to specifically target the cancer cells.
Sounds crazy, right? Like a sci-fi show? Training a person’s own cells to fight off the other cells that have gone rogue. Talk about an insurgence within our own bodies.
Believe it or not… it worked! Doug has been in remission for more than 10 years now.
Even though it seems crazy or far out, this idea of having our own cells target invaders is actually not a foreign concept to our body. It’s exactly what our immune system does all the time! At all times, we have immune cells in our body that scan for foreign invaders (pathogens) and have them destroyed. So the logic for this new treatment was sound - if our immune cells can detect and get rid of foreign pathogens, maybe we can train them to detect and get rid of our own cancer cells.
And this is exactly what CAR-T therapy does.
What is CAR-T Therapy?
CAR-T Therapy stands for Chimeric Antigen Receptor T-Cell Therapy. But before we get into the details of CAR-T therapy, we need to review what T-cells do in our bodies.
T cells are immune cells that serve many different functions, such as helping rally other immune cells to fight, destroying foreign pathogens, and regulating our immune system - short term and long term. Think of them like an army ready to attack anyone who invades your territory.
Sure, we call him “incredible” when he loses control and rages out. But it’s not quite the same when T cells go unchecked… (Image)
But one thing that will help us understand the design of CAR-T cells is that T-cells have to be very well safe-guarded because, if left to their own account, they can get out of control and start attacking our own normal cells, i.e., the case of autoimmune disease. Talk about friendly fire.
To help ensure that this doesn’t happen, 2 signals are needed before T-cells get called into action. It’s like needing 2 keys kept in separate locations to push The Red Button (in every action movie ever). The first signal is detection of a foreign pathogen. Usually T cells recognize a portion of the pathogen known as an antigen - but only if this antigen is connected to what is called an MHC receptor on a dendritic cell. (Think of this MHC receptor as the bouncer at a club holding up the squirming guy who tried to sneak in.)
The second T cell activation signal is a co-stimulatory signal. This second signal is the one to double check if we really are attacking something foreign, and if so, it gives the green light for the T cell to proceed. Once these two signals confirm that the body is truly detecting a foreign invader, then the T-cells activate and multiply, sending their army of cells ready to seek and destroy any invaders that match the original one.
T-cells come in many forms, including helper T, cytotoxic T, and regulatory T cells. But the ones we are most interested in for today’s discussion are the killer T cells. This type circulates, looking for MHC receptors presenting with an antigen and programming those specific cells to self destruct, thereby eliminating foreign invaders in the body.
You can see how this process would be a great way to get rid of cancer cells. Tracking down the specific cells and getting them to self destruct. Talk about targeted therapy!
How CAR-T Therapy Works
Aaaaand voila! This is exactly what CAR-T therapy is based on - using a person’s own immune cells to detect cancer cells and have them destroyed. But since cancer cells are not pathogens, we cannot rely on the MHC complexes to hold them down until T cells can detect them.
Instead, CAR-T therapy T cells express a special receptor with 3 domains:
The CAR (or chimeric antigen receptor) portion of a CAR-T therapy cell. (Image)
The first is a binding domain (or targeting element, teal in the picture to the right) that recognizes an antigen on the cancer cells of interest. At this point in time, that antigen is often a surface biomarker (such as the CD19 glycoprotein) on the surface of B cells.
The next domain is the signaling domain (orange in the pic) at the end of the CAR. Remember, for a T cell to activate, it needs a second co-signal for verification.
Lastly there is the transmembrane domain connecting these two (yellow in the pic).
Now is a good time to remind everyone that the C in CAR-T stands for chimeric. Aka CARs are not naturally made by the T cells. Some REALLY smart people figured out how to make a person’s T cells produce and express this non-natural receptor protein.
How, you ask? By transducing the genes for the CAR into a person’s T cell genome.
Um, what?
Genetic material encoding for the CAR (i.e., the transgene) is delivered to the patient’s T cells by viral vectors like lentiviruses or adenoviruses. These particular viruses are equipped for - and really good at - inserting genetic material into a host cell without a high risk of pathogenicity. Then, the host T cell reads the new genome, manufactures the CAR, and expresses it just like it would its normal proteins.
Interestingly, research is also exploring non-viral vectors for genome delivery, including nanovectors and mRNA. (As much like sci-fi as this all sounds, it should also ring some bells… Consider the mRNA COVID vaccines that provide our cells with instructions for producing the foreign SARS-CoV-2 protein so that we can then recognize it! So while it’s absolutely amazingly cool and crazy, it’s all coming full circle, whoa.)
How is CAR-T Therapy Administered?
Onto the fun part!
We’ve discussed the origins, structure, and mechanism of this therapy, so now it’s time to talk about how we use it for treatment.
First, we have to remove all the blood from the patient through a process called leukapheresis. This is a bit like dialysis, but instead of removing metabolic toxins and balancing electrolytes, the white blood cells (WBCs) are collected and sequestered. From this sample of WBCs, we can isolate the T cells to be modified with the CAR genomic sequence that we have ready in the disarmed virus.
My little pony knows the deal on waiting for those CAR-T cells. (Image)
This genetic material - the trans gene - is inserted into the T cells and then stimulated to multiply and grow. This engineering process generally takes 3- 6 weeks. Yep, WEEKS. Magic doesn’t happen overnight, folks. Then these modified T cells are transfused back into the patient’s body to seek and destroy their targets.
As a result, this process ends up being an extremely specific and effective therapy. So you might be asking then…will this become the first-line answer to all our blood cancer problems?
Unfortunately not yet, because of many potentially detrimental side effects.
Potential Adverse Effects of CAR-T Therapy
Cytokine Release Syndrome (CRS)
Ahh isn’t it a fine line when virtues become vices, and the exact reason a drug is effective is what also makes it dangerous? (We’ve touched on this idea before in our toxicology post.) Well, that is most certainly the case for CAR-T therapy. As we harness the power of immune cell activation to hunt down cancer cells, we can also cause quite a (cytokine) storm if left unchecked. Simply put, if the immune system response that we get from this therapy is too robust, we could be looking at anything from flu-like symptoms to organ failure. As a result, it is absolutely vital that patients be carefully monitored on this therapy.
It should also be noted that the higher the cancerous load in the body, the more likely to have a severe cytokine attack.
Neurologic Toxicity
Neurologic toxicity can develop due to inflammatory damage to the blood brain barrier, which can lead to fatal inflammation in the brain. Symptoms can range from headaches to insomnia to delirium.
Specifically, there is a need to monitor for Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS). While it is fairly common after CAR-T therapy (up to 60% of patients) and may be reversible with appropriate management, it can also progress to multiple life-threatening neurological symptoms, including status epilepticus, cerebral edema, and/or intracerebral hemorrhage.
Other adverse effects include infections, cytopenias, hypersensitivity reactions like anaphylaxis, and secondary malignancies. In other words, while this type of therapy is extremely revolutionary and has certainly proven beneficial in hematologic malignancies, it is not without substantial risks and necessary monitoring.
Aucatzyl (obecabtagene autoleucel)
Now that we’ve covered the basics of CAR-T therapy, we can explore Aucatzyl (obecabtagene autoleucel). Let’s do so by walking through a journal club for the 2024 FELIX study (NCT04404660).
FYI, even though the generic name is super cool (and the cool kids are apparently calling it obe-cel), it’s pretty obnoxious to type every 5 seconds. So we’re going to break with pharmacy etiquette and just call it Aucatzyl for the rest of the post.
The purpose of the FELIX study was to evaluate the safety and efficacy of autologous T cells engineered with a chimeric antigen receptor (CAR) targeting CD19 in adult patients with relapsed or refractory B cell acute lymphoblastic leukemia (ALL). That is, the FELIX study was conducted to see how well Aucatzyl works for these refractory patients.
To break that down, Aucatzyl is the latest and greatest of the CAR-T therapy family. You can think of Aucatzyl as the Mr. Miyagi for an ALL patient’s T cells. It is the product that is used to transduce the therapeutic CAR gene to a patient’s own T cells so that they will seek and destroy CD19-expressing cancerous B cells after being reinfused. CD19 is the selected target of this CAR-T therapy as this protein is largely expressed on B cells, which are the ones out of control in B cell ALL. As a reminder, let’s check out how the B cells fit with the other blood cells:
As you can see from this diagram, the B cells are just one of many types of blood cells, so Aucatzyl must make a patient’s T cells very specific in order to minimize friendly fire to other essential cells. (Image)
The FELIX trial was a Phase Ib/II open-label, multi-center, single arm study. Breaking that down…
Open label meant that everyone (from the investigators to the patients) knew what treatment was being given to the subjects. Single arm meant that every subject was getting the same treatment. There was no comparator or control group. This makes sense as it is indicated for relapsed and refractory ALL, where oftentimes we have exhausted other options.
Multicenter is great in that they were able to capture a larger, more diverse group of subjects. It was a Phase IB/II trial. This means that it’s still in a relatively early phase. Phase IB refers to testing for the dosing, administration, and safety of the product. Phase II refers to determining its efficacy in a relatively small sample size.
Patients were included if they met the following criteria:
Age 18 years or older
ECOG performance status of 0 or 1
Relapsed or refractory B cell ALL
Patients with Ph+ ALL were eligible if intolerant to TKI, failed two lines of any TKI, or failed one line of second-generation TKI, or if TKI is contraindicated
Documented CD19 positivity within 1 month of screening
Phase Ib: Primary Cohort IA: Presence of ≥5% blasts in bone marrow (BM) at screening
Phase Ib: Exploratory Cohort IB: MRD-positive defined as ≥ 1e-4 and <5% blasts in the BM at screening
Phase II: Primary Cohort IIA: Presence of ≥5% blasts in BM at screening
Phase II: Cohort IIB: ≥2nd CR or CRi with MRD-positive defined as ≥1e-3 by central ClonoSEQ® NGS testing and <5% blasts in the BM at screening
Adequate renal, hepatic, pulmonary, and cardiac function
The key takeaways here are that participants were of relative healthy functioning, having adequate organs and ECOG scores, but also relapsed or refractory ALL. Having both these criteria met may not be truly reflective of real life scenarios because if a patient is classified as a relapsed/refractory case, then they likely are not going to be in the best overall condition. Also of note, ALL is primarily diagnosed in children. So to only include patients 18 years and older may not be entirely representative of the true population that stands to benefit from this therapy.
On the other hand, patients were excluded from the FELIX study if…
Phase Ib (Cohort IA and Cohort IB) and Phase II (Cohort IIA and Cohort IIB) B-ALL with isolated extramedullary (EM) disease
Diagnosis of Burkitt's leukaemia/lymphoma or CML lymphoid in blast crisis
History or presence of clinically relevant CNS pathology
Presence of CNS-3 disease or CNS-2 disease with neurological changes
Presence of active or uncontrolled fungal, bacterial, viral, or other infection requiring systemic antimicrobials for management
Active or latent Hepatitis B virus or active Hepatitis C virus
Human Immunodeficiency Virus (HIV), HTLV-1, HTLV-2, syphilis positive test
Prior CD19 targeted therapy other than blinatumomab. Patients who have experienced Grade 3 or higher neurotoxicity following blinatumomab.
Of note, there were a lot of restrictions regarding a history of neurological pathology, which makes sense with CAR-T therapy’s neurological risks, including ICANS.
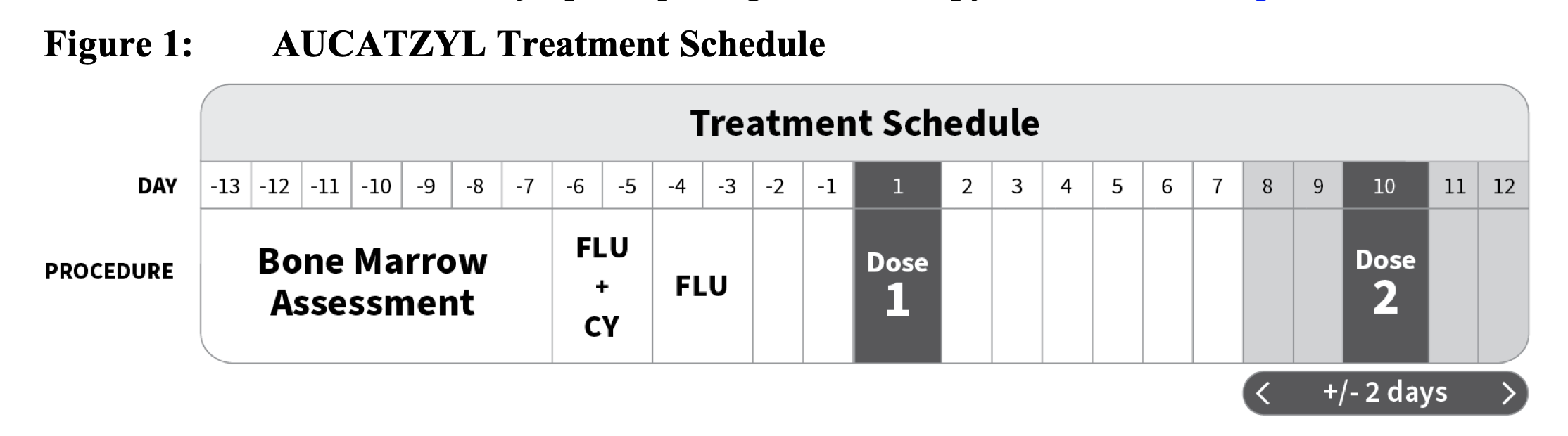
For included patients, a bone marrow assessment was obtained 7 days before starting pre CAR-T chemotherapy. This assessment was imperative because Aucatzyl dosing depends on the patient’s bone marrow blast percentage.
Why do we dose Aucatzyl based on blast percentage? CAR-T cells are highly activated when they meet their target. Think of them as overeager soldiers. So if there is a high number of blasts in the body, this means a high disease burden. In this case, the CAR-T cells we infuse rapidly expand and release large amounts of inflammatory cytokines, leading to dangerous side effects like CRS and ICANS.
On the other hand, if we dose according to disease burden, then the CAR-T cells will be able to more strategically attack the target cells, while (hopefully) releasing cytokines at a rate that the body can keep up with.
Once the bone marrow assessment was completed, patients proceeded with lymphodepleting chemotherapy. For Aucatzyl, this meant cyclophosphamide and fludarabine. The dosing was fludarabine (FLU) 30 mg/m2/day intravenously (IV) for four days and cyclophosphamide (CY) 500 mg/m2/day IV for two days starting with the first dose of fludarabine. (Total doses: FLU 120 mg/m2 ;CY 1000 mg/m2)
Three (+/- 1) days after chemotherapy was completed, Aucatzyl was infused. The total target dose was 410 x 10^6 of CD19-positive CAR T cells divided into split doses on Day 1 and on Day 10 (±2 days).
(Image)
Now onto how the doses of Aucatzyl are split based on that bone marrow assessment we took earlier.
(Image)
As you can see, if the blast percentage was high (>20%), patients received a lower Aucatzyl dose on day 1 to mitigate risks of ICANS or CRS from high disease burden. On the other hand, if the blast percentage is lower (</=20%), patients were started with a higher dose.
Note that patients also received premedication with acetaminophen 30 minutes prior to Aucatzyl infusion. Tocilizumab, an anti-inflammatory monoclonal antibody (anti-interleukin 6 or anti-IL-6), was also on hand in case of a CRS reaction.
From there, the patient was monitored for at least 14 days at the administering facility. They were also monitored at least 4 weeks after each infusion.
So what did they find? Did Aucatzyl do its duty in the FELIX study??
First, let’s take a quick look at the study population so we know who we’re evaluating…
A total of 112 patients were enrolled and underwent leukapheresis.
18 patients (16%) stopped the study prior to Aucatzyl infusion for various reasons, including death (n=11), adverse event (n=1), physician decision (n=1), and manufacturing failure (n=5).
94 patients received at least one dose of Aucatzyl, but only 65 patients met criteria for the efficacy-evaluable population based on blast percentage. Population characteristics of efficacy-evaluable patients were as follows:
Median age was 51 years (range: 20 to 77 years)
35 patients (54%) were female
47 patients (72%) were White, 8 patients (12%) were Asian, and 1 patient (2%) was Black or African American. Twenty-one patients (32%) were of Hispanic or Latino ethnicity.
At enrollment, 35 patients (54%) were refractory to the last prior line of therapy, and 32 patients (49%) relapsed to first-line therapy within 12 months.
The median number of prior lines of therapy was 2 (range: 1 to 6).
Five patients (8%) only received the first Aucatzyl dose, primarily due to adverse events (5%).
The major efficacy outcome measures were rate and duration of complete remission within 3 months after infusion. Additional outcome measures were rate and duration of overall complete remission which includes complete remission at any time.
This means that of those who were able to be evaluated as efficacious, 27 (42%) achieved complete remission within 3 months and had a duration of remission for a median of 14.1 months. Then if they extended the time to remission to any time, 41 (63%) were able to achieve overall complete remission with a median duration of 14.1 months as well. Not bad considering these were people who were running out of options!
Additional Information about Aucatzyl
Drug Interactions
Just as with other CAR-T or chemotherapy, since we are getting rid of many healthy cells in the process of killing off the cancer cells, this leaves patients largely at risk of immunosuppression. So it is best for these patients to avoid any further immunocompromising treatments or live vaccines.
Special Populations
Aucatzyl is not recommended for pregnant women, and no data has been established for the effects in lactation. It has not been studied yet in children, despite ALL being mainly found in children. For geriatrics though, about 20% of participants were 65 and older, and no significant differences were found in safety and efficacy compared to younger patients.
Black Box Warnings
Cytokine Release Syndrome (CRS)
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS)
T cell malignancies
As discussed in our introduction, some of CART-T therapies’ most dangerous side effects are those shown in the Black Box Warnings, so it makes sense that they are the top priorities to monitor for.
The tl;dr of CAR-T Therapy and Aucatzyl
How exciting that the future is now and we can train our cells to attack the enemy within: cancer.
But just as with any new product, with great gains come great risks as seen in the adverse effects of CAR-T therapy. However, when options are limited (as in the case of relapsed or refractory B cell ALL), having another therapy available can have a huge impact for patients. Although there are no head to head trials directly comparing Aucatzyl to other CAR-T therapies and although the population studied in FELIX does not truly reflect the (younger) folks that may benefit most frequently from this therapy, it is certainly exciting and promising to see how this therapy develops! Just be aware to pay close attention to dosing, monitoring, and premedication to mitigate the risks of serious adverse effects like CRS and ICANS.