What Every Pharmacist Should Know about Contraception
Steph’s Note: This week, we’re back with another crucial clinical topic - contraception. Regardless of practice setting, it’s essential for all of us pharmacists to be able to recognize the different types of contraceptives available and at least have a basic understanding of how they work. If there’s any evidence out there of just how important this topic is, know that there’s a tl;dr cheat sheet on Women’s Health that beautifully outlines a LOT of information. (And if cheat sheet status doesn’t demonstrate importance, we don’t know what does!)
If, however, you’re like I was (am?) with this topic, and you need more explanation before you jump straight to the cheat sheet, Devki Gajera is here to fill in the gaps. If you don’t recognize her name yet, you should definitely pop over to Devki’s previous, thought-provoking post about race coefficients in clinical equations. She’s got some serious knowledge to share with us, and her teaching skills are on point. (I almost said, “on fleek,” just for kicks and giggles, but I couldn’t face the subsequent self-loathing I would feel afterwards.)
Take it away, Devki!
At first, learning about contraceptives can be summarized in one word: overwhelming. There are so many types, each with many brand names. Choosing the best option for patients and identifying unique counseling points are essential for helping patients stay adherent. Today, I’m here to give you some comfort and tell you that contraceptives can be boiled down to three major buckets: hormonal, non-hormonal, and emergency:
See… it’s not soooo complicated, right??
But before we make too many determinations about how complicated it all is, let’s take a step back to define and drop some history facts.
What is contraception?
Contraception is the prevention of pregnancy by either…
preventing a fertilized ovum from implanting in the endometrium, or
preventing a sperm from meeting a mature ovum.
We have methods that target both of these!
The history of contraception essentially spans all of time and is heavily (and uniquely) intertwined with political and economic movements. The first commercially-manufactured contraceptive was a suppository made from cacao butter and quinine in 1886 and commonly used through World War II. (And you thought the only historical use of quinine was for restless legs!)
It wasn’t until 1914 that the term “birth control” was coined by Margaret Sanger, a leader during the early feminist movement who worked to expand access to contraception. In 1957, Enviod became the first FDA-approved oral contraceptive - quickly being dubbed, “The Pill”. After 5 years, 1.2 million American women were taking “The Pill.” In a nutshell, access to contraception revolutionized society. It’s estimated that almost 2 in 3 women (65%) aged 15-49 are using contraception today.
Keeping that stat in mind and knowing now just how far reaching these therapies are, how many of you can honestly say you feel comfortable discussing how contraceptives work or the most important counseling points?
Yeah, don’t worry, you’re not alone if you’re not comfortable. That’s why we’re having this chat!
Even though contraception is more accessible today and female use is quite prevalent, about 45% of pregnancies in 2011 were unintended. Individuals falling into lower socioeconomic brackets and of younger age are more likely to have unintended pregnancies. Pharmacists can play a major role in educating patients taking contraceptives about possible adverse effects and optimal adherence strategies. In the case of emergency contraception, creating safe spaces for education and questions is just as crucial.
Now, let’s dive into the three contraceptive buckets.
BUCKET 1: Hormonal Contraceptives
To understand hormonal contraception more intuitively when you come across a new brand on the shelf or in the news, it’s necessary to be familiar with the normal menstrual cycle and the role of major hormones (the figure below and this Osmosis video are both great overviews). To sum it up:
The normal menstrual cycle. (Image)
Gonadotropin release hormone (GnRH) is released by the hypothalamus.
This stimulates follicle-stimulating hormone (FSH) and luteinizing hormone (LH) to be released by the pituitary gland. This green-lights the ovarian follicles to grow and triggers ovulation (i.e,. when a wee follicle grows into a mature egg that can be fertilized by sperm).
Then, estrogen and progestin are released from the ovary. These work to prepare the uterine lining for implantation.
If the egg is not fertilized, the increased levels of estrogen and progestin trigger a negative feedback that is menses.
This repeats every 28 days!
So how does hormonal contraception fit in?
Hormonal contraception provides a steady level of synthetic estrogen and progestin to trick the body into believing it’s already pregnant, preventing the need to stimulate ovulation. Estrogen suppresses FSH, preventing follicle development; however, it mostly works to keep the cycle in a hormonal rhythm. Progestin provides most of the contraceptive effect by inhibiting ovulation. Essentially, the body stays at Step 3 from above.
Hormonal contraceptives come in many shapes and forms, as you may know if you’ve ever worked in a community pharmacy or had to find formulary alternatives!
Within Bucket #1 of hormonal contraceptives, there are two smaller buckets:
Combined hormonal contraceptives (CHCs)
Progestin-only contraceptives
Combined Hormonal Contraceptives (CHCs)
CHCs can be oral, transdermal patches, or vaginal ring formulations. We’ll take each of these types one by one and break them down a bit further…
Combined oral contraceptives (COCs) have different ratios of estradiol (estrogen) and progestin (norethindrone, levonorgestrel, drospirenone) with varying hormonal phases. Women who are overweight or obese may require higher doses of estrogen since the failure rate is considered to be higher at lower doses. There are a few name hacks though!
Brand names with “Lo” generally have lower estrogen doses (<35 mcg).
Monophasic options (Loestrin 24 Fe, Yaz, Cryselle, Ortho-Cyclen) have the same hormone dose for active hormone pills (whether that’s 21 hormone/7 placebo or 24 hormone/4 placebo pills).
BIphasic, triphasic, and quadriphasic medications have 2, 3, or 4 different doses, respectively, over the 21 or 24 hormone days. Brand names with “Tri” or “7/7/7” are triphasic (Ortho Tri-Cyclen). Quadriphasic mimic the menstrual cycle most closely.
Extended-cycle options (Seasonique, Lo Loestrin Fe) cause menstruation every 3 months. (Hence, Seasonique is like 4 periods/seasons a year with 12 weeks of active hormone pills.)
Continuous-cycle medications have no placebo pills and prevent any menstrual periods.
(Image)
There are several key counseling points associated with COCs. First, assuming perfect adherence, COCs are 99% effective at preventing pregnancy. However, if more than one dose is missed, a backup contraceptive method should be used. If missed doses are in Weeks 2 or 3, then the placebo week should be discarded, and a new pack should be started altogether. Next, oral options do not prevent transmission of sexually-transmitted infections (STIs).
So who’s the ideal patient for a COC? Someone with a high chance of solid adherence who prefers an oral option.
Now on to the next type of combined hormonal contraceptive: transdermal patches.
Transdermal CHC patches (e.g., Xulane) are applied weekly (3 weeks on, 1 week off). The systemic estrogen exposure is higher with patches compared to oral options, which may increase the risk for venous thromboembolisms (VTEs) (~10-15 per 10,000 women per year), although the data has been slightly inconsistent. Nonetheless, clots are no joke, so the FDA has included this risk in the labeling.
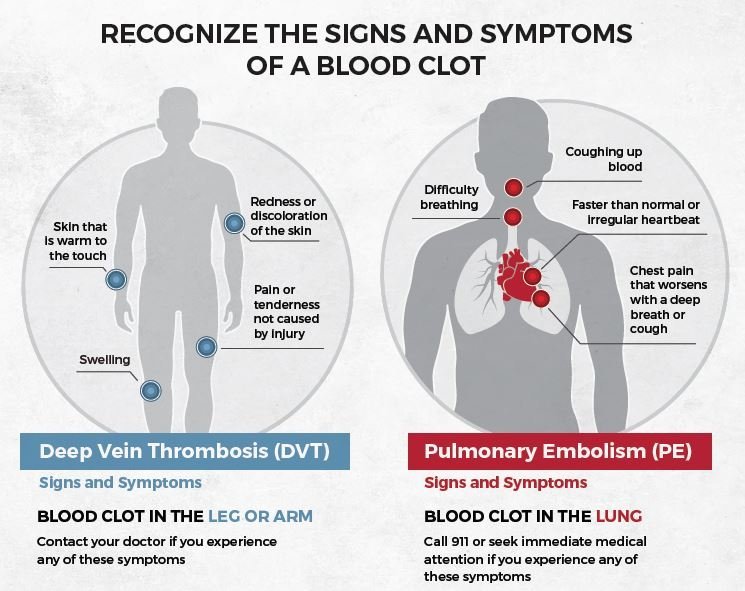
Key counseling points for transdermal patches? Patients need to remember to go patch-less on the 4th week. If the patch falls off for more than 24 hours, then they have to start all over from Week 1. Patients should also be counseled on signs and symptoms of a blood clot. (Check out the image below for some easy-to-remember common symptoms of VTEs. Then you can use this when you’re counseling patients on all kinds of meds, including warfarin and the other anticoagulants!)
So who’s the Ideal patient for a transdermal combined hormonal contraceptive? Someone who prefers a weekly dosing option, is less likely to be adherent to oral medications, and females who weigh less than 198 pounds. (There’s some evidence that the patches are not as effective at their contraceptive job in patients over this weight limit.)
Now on to the last type of CHC: vaginal rings.
Vaginal ring CHCs (e.g., NuvaRing, Annovera) are inserted into the vagina monthly by patients themselves (3 weeks on, 1 week off).
Key counseling points for vaginal ring CHCs include information about what to do if that ring doesn’t stay where it’s supposed to… If the ring is displaced for more than 3 hours, then a backup contraceptive should be used. Otherwise, it can be reinserted. Also (and only because things happen and we can’t make this stuff up), vaginal rings are not meant to worn as bracelets. And they’re not meant to be cut into 28 little bits to take orally. Truly. Be sure to emphasize the vaginal route and insertion.
So who is the ideal patient for a vaginal ring? Likely someone who has less than optimal adherence to oral medications and perhaps has experienced skin reactions to the patch.
(Image)
This wraps up the CHC section! The next time you come across a CHC, test yourself: how many phases are there based on the name? What counseling will you provide to the patient?
So on to the other type of hormonal contraceptives: those that contain just progestin.
Progestin-only contraceptives
Progestin-only contraceptives can be oral, intrauterine devices (IUDs), injections, and implants. As a reminder, the progestins include norethindrone, levonorgestrel, and drospirenone.
Of these 3 progestin options, drospirenone in particular is less androgenic and is actually a potassium-sparing diuretic (yep, like spironolactone and eplerenone!). So metabolic effects like weight gain, mood swings, and acne, as well as bloating, are minimized. Unfortunately, drospirenone also has a higher risk of VTE than other progestins (~10-15 per 10,000 women who used drospirenone-containing oral contraceptives).
Of note, progestin-only contraceptives are the best options for certain females due to the increased risk of stroke associated with estrogen. These folks who may benefit from progestin-only contraceptives include those who have a history of…
breast cancer,
DVT/PE,
diabetes with microvascular complications,
migraines with aura,
uncontrolled hypertension (>160/90 mmHg),
smokers who are older than 35 years,
hypercoagulable states,
systemic lupus erythematosus,
pulmonary hypertension,
high risk of atrial fibrillation, and (finally)
those who are pregnant or breast-feeding <6 weeks postpartum (FYI, estrogen also decreases milk production).
I know, I know, that is A LOT to remember!! But just remember to be vigilant of patients with cardiovascular risk or history when making contraceptive recommendations. So now let’s take each of the types of progestin-only contraceptives and break those down one by one.
Oral, progestin-only contraceptives
Progestin-only pills, or Mini-Pills, contain 28 active hormone pills. So adherence is absolutely essential! Some key counseling points for this type includes the shorter half-life than CHCs, which means doses really must be taken at the same every day. If 3 or more hours from the scheduled dose have passed, then a back-up contraceptive should be used for 48 hours.
Talk about pressure to adhere, right? Gosh, being 3 hours late on a dose is usually considered not a huge deal for many medications. But with this, you oversleep because you had a late night with your friends, and guess what - backup method required!
The ideal patient for these oral progestin-only contraceptives is really a breast-feeding female.
Now on to the non-oral, progestin-only formulations.
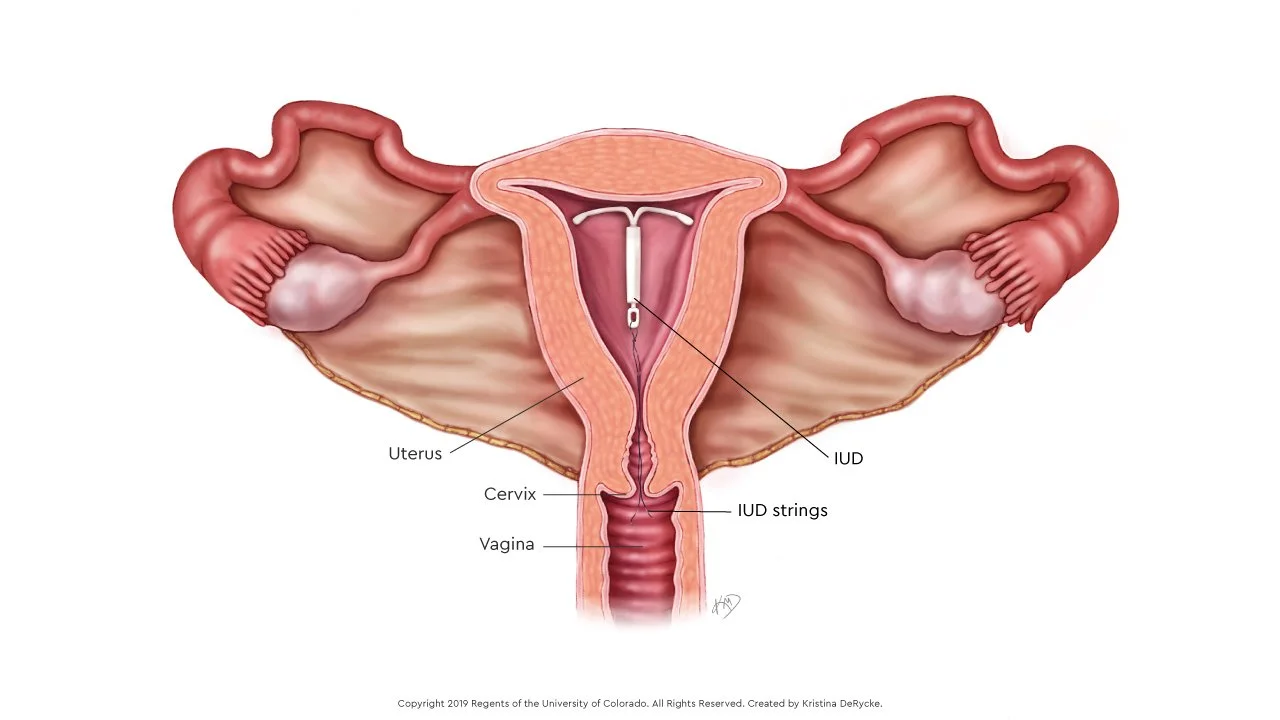
IUDs live a bit higher up in the female reproductive tract than vaginal rings, which is why they must be placed by a provider and often require some measure of anesthesia to do so. (Image)
Progestin-containing intrauterine devices (IUDs) are some of the most effective contraceptive methods. These devices can be left in place for 3, 5, or even up to 7 years depending on the type. They do require vaginal insertion by a provider, so these are not DIY at home like the vaginal rings.
There are four levonorgestrel-containing IUDs (Skyla, Liletta, Mirena, and Kyleena). These vary in amount of progestin released from beginning to end, although all of them decrease in progestin dose released over time. The longest-lasting product of the four is Mirena, which may remain in place for up to 7 years (recently extended by the FDA from 5 years). The shortest product is Skyla, which is only approved for up to 3 years’ use. Choice of product will depend on a patient’s contraceptive and family planning desires (if any).
Patients should be extensively counseled before having a progestin-containing IUD inserted. Some of the most important counseling points are that there are plastic strings attached to the IUD that can help patients confirm that the IUD is still in place, although displacement is very uncommon. One way to avoid displacing an IUD is to avoid using menstrual cups. Some patients experience cramping after IUD placement (similar to severe menstrual cramps). NSAIDs can help with pain, although patients should certainly be encouraged to contact their provider for refractory pain as ovarian cysts can develop with IUDs.
So who could be the ideal patient for a progestin IUD? Often these are good choices for someone with poor medication adherence since they’re kind of a “set and forget” option. On the other hand, it’s important for patients with IUDs to be those who are cautious about their sexual habits and partners as sexually transmitted infections (STIs) can develop into raging cases of pelvic inflammatory disease (PID) in the presence of an IUD. (Nothing like a nice, internal foreign object for a pathogen to latch onto and make its new home base!) So ideally, IUDs are for patients without a history of STIs or pelvic inflammatory disease.
Depot progestin injections are given either intramuscularly (Depo-Provera) or subcutaneously (Depo-SubQ) every 3 months by providers. The risk for bone loss requires a risk-benefit analysis for prolonged use after at least 2 years of use.
Key counseling points for these contraceptives are that they can cause menstrual irregularities and weight gain. They also have an FDA black box warning for bone loss, which was added to the labeling in 2004.
The Ideal patient for these long-acting injections is someone who is not planning to become pregnant in the near future. This is because it can take longer to conceive after discontinuing this contraception. These forms can be useful in a breast-feeding patient with poor adherence to pills or underweight patients (due to the ability to cause weight gain). Interestingly, patients with sickle-cell disease may be good candidates for progestin injections as they may reduce frequency of pain crises given the lower risk of thromboembolism compared with estrogen-containing contraceptives.
Subdermal implants (etonogestrel, Nexplanon) are effective for up to 3 years. Unlike an irreversible depot injection, fertility can kick back in a week after implant removal. So sort of a “set and forget” option but also with a quick off action for people who want that flexibility for family planning. This makes the ideal patient for these formulations someone who maybe isn’t great about medication adherence but also might be considering pregnancy soon-ish. Patients who choose the implant should be counseled about the possibility of menstrual spotting.
Whew, that’s a lot of information about ALL of the hormonal choices! Sometimes, patients prefer to read the package insert (which is legally required to be dispensed with each and every fill, FYI) for those details and then address specific concerns about starting or continuing medications.
Counseling Pearls for Patients New to Hormonal Contraception
When should I start a new oral contraceptive pack?
As pharmacists, you may get this question when a patient is starting medication for the first time. First and foremost, it’s essential to inform all patients that they should continue to use a backup contraceptive method for at least 7 days after starting. After that, luckily, there are several methods that patients may use when starting a contraceptive:
Start on the first day of bleeding during the menstrual cycle.
Start on the first Sunday after the menstrual cycle starts. (This is sometimes the most convenient long-term because it allows weekends free of menstrual periods.)
Start on the 5th day after the menstrual cycle starts.
“Quick start” occurs when women take the first dose in the clinic. Their menstrual cycle will be “rescheduled” to occur when the active pills in the pack are complete.
Should I be worried about other medications with this contraception?
Rifampin at the top of a drug interaction list? You don’t say. (Image)
Speaking of starting new medications, pharmacists intuitively scan medication lists for potential interactions, but patients don’t always know to consider the effects of other medications on their contraception. So first, patients should always be encouraged to reach out if they start or stop any new medications to check for important drug interactions. Additionally, patients on lower doses of oral contraceptives are more susceptible to lowered efficacy and should consider using backup methods of contraceptives whenever possible. Here are a couple MAJOR interactions to log away:
Rifampin (surprise, surprise) is THE drug that can reduce estrogen exposure via induction of CYP3A metabolism. This reduces contraceptive efficacy.
Other antibiotics, like tetracyclines and penicillins, MAY affect efficacy based on case reports. You can still recommend backup contraception during antibiotic use, especially if patients report breakthrough bleeding.
Anticonvulsants (e.g., phenobarbital, carbamazepine, and phenytoin) induce CYP3A metabolism and can reduce contraceptive efficacy. Since these are maintenance medications, perhaps a depot injection or IUDs are better options.
What are the side effects of my new contraceptive medication?
If patients come to you reporting side effects, knowing the hormone content is really important as shown in Table 1. Many side effects do improve by the third cycle, but for some patients, these may severely affect quality of life. Generally, medications should be tried for at least 2 cycles prior to making changes. Likewise, if patients have certain side effects they want to avoid prior to starting therapy, such as weight gain, then understanding physiological effects can determine alternatives!
Before I dive into non-hormonal contraceptives, let’s put what we’ve discussed into practice with some examples of patients taking hormonal contraceptives:
Issue: Reports of breakthrough bleeding during the beginning of their cycle.
Recommendation: Increase the patient’s estrogen content.
Issue: Complaints of mood swings affecting personal relationships.
Recommendation: Decrease progestin content.
Issue: Concerns with acne or oily skin.
Issue: Consider drospirenone-containing products (remember, it’s less androgenic than other progestins!).
BUCKET 2: Non-Hormonal Contraceptives
Snip snap, snip snap, snip snap! (If you know, you know.) (Image)
Contraceptives without hormones include condoms, diaphragms, spermicides, surgeries (vasectomy for males and tubectomy/tubal ligation for females), and abstinence (which is the only 100% effective method to prevent pregnancy). Surgeries are the most effective PERMANENT method of contraception (although some are technically reversible).
Condoms are physical barriers available for men and women, although those for women are generally more expensive and have a higher failure rate. Male and female condoms should never be used simultaneously due to the risk of displacement.
Female condoms can be inserted 8 hours before intercourse.
Latex or synthetic (polyurethane) condoms, unlike oral contraception, help to prevent STIs, and they have about a 2% failure rate.
Diaphragms provide a cap and prevent sperm movement. These reusable contraceptives require prescriptions to ensure proper fitting. They should be used with spermicides.
Ideal patient: no history of recurrent urinary tract infections (UTIs), toxic shock syndrome, or allergy to latex/rubber.
Cervical caps (FemCap) are made of silicone. These have to be filled with spermicide before use. Unlike condoms and diaphragms, they should be inserted 6 hours before intercouse and kept in place for 6 hours after.
Ideal patient: no history of recurrent UTIs, toxic shock syndrome, or allergy to latex/rubber; someone who is able and willing to plan intercourse.
Spermicides (like foam, sponges, jellies) contain nonoxynol-9 which breaks down sperm cell walls. They do not protect against STIs. They are considered one of the least effective methods of contraception. They should be inserted into the vagina 10-15 minutes before use and are effective for one hour.
Phexxi gel is a prescription vaginal gel that has to be applied within an hour before intercourse. It has up to a 14% failure rate.
Ideal patient: one with no history of UTIs.
As you can see, there are many choices available with or without prescription, for males or females, and with varying effectiveness levels. Ultimately, the bottom line for non-hormonal contraceptives is this:
Cons: many brands, many types, many doses
Pros: many brands, many types, many doses
Wait, HUH? Pros = cons? Having so many options, in fact, means that patients have the freedom (insurance-limited) to switch contraceptives based on cost, side effects, adherence, and personal comfort. Which can be really useful! However, it also means that education on proper use becomes all the more essential as patients may switch products without fully understanding how to use them or the caveats associated with each type. Understanding a patient’s goals and baseline knowledge should help narrow down choices on the front end and steer the education conversation!
BUCKET 3: Emergency Contraception
Emergency contraception (EC) is used to prevent unwanted pregnancy after intercourse. (I’ve always heard about women having a prescription on file just in case it’s needed, but I’ve rarely seen this occur in practice.)
With all of these ECs, patients should be educated on what to expect: nausea, vomiting, and irregular bleeding.
Progestin-only (Plan B One-Step, Next Choice) are specifically FDA-approved for EC and are generally used first-line. They work to inhibit or delay ovulation. Next Choice is two doses, taken 72 hours within intercourse and then again 12 hours later. Plan B One-Step is just one tablet that’s taken within 72 hours of intercourse. These are available without prescriptions.
Ulipristal (Ella) is a selective progesterone receptor modulator which works to delay ovulation. Unlike progestin-only ECs, this requires a prescription, and can be taken up to 120 hours after intercourse. It may not be the ideal choice for those who are unable to visit a prescriber within the efficacy time period, but on the other hand, this is the MOST effective ORAL EC. Of note, scheduled contraception can be resumed 5 days after taking ulipristal.
A copper IUD is almost 100% effective if inserted by a provider within 5 days of unprotected intercourse. It isn’t as commonly used, but it might make sense for women who want to remain on contraception long-term since it’s good for 10 years. It may also be useful for women who are overweight or obese. It is the MOST effective emergency contraception overall.
High-dose oral contraceptives may be recommended by some providers. The timing is like Next Choice (first dose within 72 hours, then second dose 12 hours later). This may be a good choice for patients who don’t have time to go to the pharmacy, already have oral contraceptives on hand, or can’t afford progestin-only ECs. Top tip: taking nausea medications an hour before starting this type of regimen can help with the estrogen-induced nausea.
The tl;dr of Contraceptives
Contraceptives available on the market will keep adapting to what patients are using and avoiding - new year, new contraceptive. A few major points to keep in mind:
Be sure to consider a patient’s expected or self-reported adherence: are there daily routines in place where an oral option could be tagged in? Combined oral contraceptives are almost 99% effective when used perfectly, meaning 100% adherence. Progestin-only pills give you a 3 hour window to maintain strict adherence. But someone who travels for work may not want to carry pill packs or patches around, so maybe an IUD, patch, or ring makes more sense.
Always check in about side effects and comfort with new medications. Perhaps the estrogen or progesterone content needs to be adjusted to accommodate side effects.
Scan the medical history for cardiovascular disease or risk, especially in folks being prescribed CHCs.
Check for drug interactions and counsel patients to ask when they start or stop new medications!