Migraine Management: Beyond the Triptans
Steph’s Note: Since I recently started a new job in a neurology clinic, I’ve been encountering a lot of chat about treatment of migraines. Who knew migraine would be the next big thing in neuro??
Ok, maybe some of you have been waiting for these meds for years. Or maybe you suffer from migraines yourselves. I was probably just out of the loop because we would never actually use these medications in the inpatient world.
Regardless, it’s time to chat injectable migraine meds so that wherever you practice, you’ll recognize and understand these medications on your patients’ lists. Migraine meds don’t have to be such a headache.
C’mon, you knew it was coming…
What is a migraine?
This is actually a really difficult question. Many of us would likely automatically say it’s a fierce headache.
Which isn’t untrue, per se. It’s just not always true.
Migraines come in multiple forms, and none is them is particularly well understood. Check out the following summary table to learn more about several migraine classifications according to the American Migraine Foundation.
This brings us to this aura. (Oooo…sounds spooky! But this is not the misty cloud surrounding a person in a movie that only someone with a 6th sense can detect, although that is another meaning of the word aura. No evil auras.)
One example of a visual aura. Little trippy, right? (Image)
When talking about migraine, an aura refers to sensory changes that can either start shortly before or during a migraine. These symptoms generally last up to a half an hour, although there’s variability between patients.
Usually an aura consists of visual changes, like seeing dots, squiggly lines, or lightning flashes. But other senses can also be affected. Sensory auras can manifest as tingling or numbness. Patients may have a dysphagia aura, in which they have difficulty forming speech. Motor auras are also possible.
How common are migraines?
Pretty darn!
According to the American Headache Society in 2018, almost 20% of women and a little over 5% of men will experience a migraine in the period of a year. Attacks are most common between the ages of 25 and 55 years old.
Probably most astounding is that, even with all of the other neurologic conditions we see in our daily inpatient practice - strokes, seizures, Parkinson’s, etc. - migraine is the SECOND most debilitating neurologic condition in the world when measured according to years lost to disability.
Geez! No wonder this is a hot spot of medication development! That’s a lotta people losing quality of life and productivity.
Not to mention there’s a $27 billion financial burden price tag associated in the United States. Yep, that’ll spur pharma to do some research.
(So basically, I should have known more about them prior to starting this new job, especially now after seeing the numbers. But hey, better late than never.)
For the rest of this post, we’re going to focus on chronic migraines.
What causes chronic migraine?
I promise this is meant to be an informative post, but I’m sorry to say again that we just don’t fully know!
Contributory hypotheses that we do have some evidence for include cortical hyperexcitability, overly sensitive trigeminal and thalamic neurons, and increased release of pain mediators (nociceptive molecules). Basically, the pain pathways are ramped up, and the neurons are hypersensitive.
One of the nociceptive molecules that has been more highly studied is CGRP, or calcitonin gene-related peptide. Previous studies have demonstrated increased release of CGRP from trigeminal nerves, which then leads to increased neuroinflammation, which in turn leads to more CGRP release. It’s a vicious cycle…
In chronic migraine versus other types, CGRP levels seem to remain more consistently elevated. So whereas in other types, CGRP levels may abate between attacks, they don’t subside to the same degree in patients with chronic migraine.
How do we treat chronic migraines?
There are two buckets to this question. The first is how do we acutely treat the migraine, and the second is how do we prevent symptoms from occurring so frequently.
Acute Management of Migraines
There are essentially 3 categories of options here:
Analgesics, e.g., acetaminophen
NSAIDs, e.g., ibuprofen
Triptans (or 5HT agonists)
Although you may have dispensed the classic Fiorinal and Fioricet scripts for headaches, or perhaps even opioids like tramadol or hydrocodone, these types of medications are falling out of favor for multiple reasons. First, The Opioid Crisis and these meds’ addictive properties. Second, they may actually perpetuate or worsen headaches, a phenomenon known as medication overuse headache (MOH) or a rebound headache.
Unfortunately, it’s not entirely clear whether overuse or chronic use of just about any medication used for acute migraine relief may lead to MOH. Even down to triptans, which with continued use may actually increase CGRP! Or even ibuprofen.
Sooo that’s unfortunate for these patients.
Plus, there’s that pesky (but valid) warning on triptans to not exceed max dosages in a certain time period, which also doesn’t help if your patients are having headaches the equivalent of every other day (based on >15 headache days/month).
So if we don’t have viable or effective acute treatment options that can be used at the frequency that patients with chronic migraines need, we simply need to PREVENT the migraines from happening in the first place, right?
Ha. Easier said than done.
But guess what - maybe we’re not so crazy for thinking that….
Prevention of Migraines
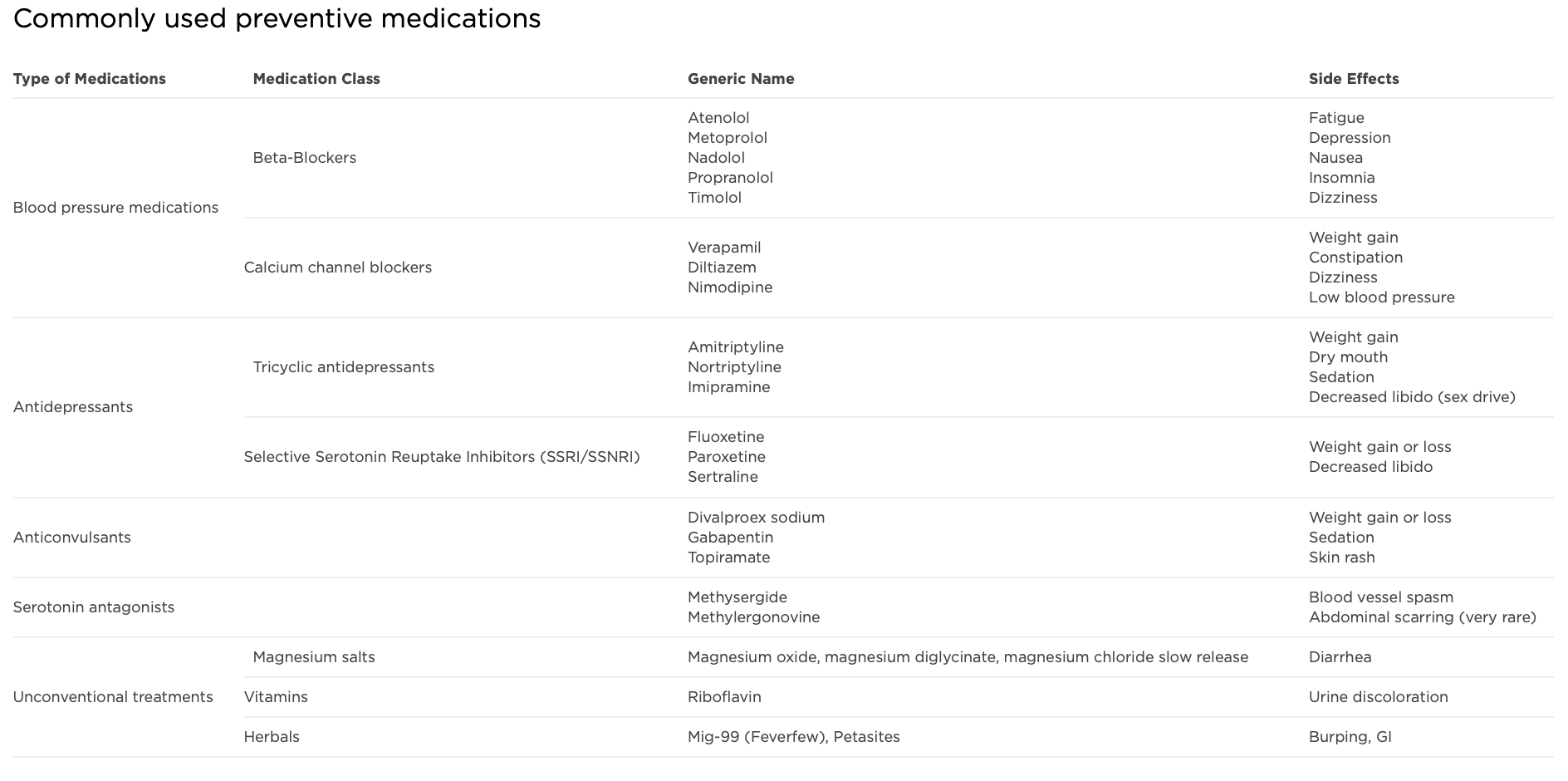
Historically, we had a mish mash of non-targeted therapies to try and prevent migraines. Take a look at the below chart from the American Migraine Foundation:
(Image)
Now we’re all pharmacy people here. What do you notice about this list?
A lot of these medications are used for other indications. We have beta blockers, used in cardiac diseases like hypertension, myocardial infarction, atrial fibrillation, and heart failure. There are calcium channel blockers, also used in hypertension or atrial fibrillation. Tricyclic antidepressants and SSRIs, used for depression, anxiety, and insomnia, just to mention a few. There are anticonvulsants, used for epilepsy, neuropathic pain, and even bipolar disorder in some cases!
Not exactly a list that jumps out and says, “I target migraines!”
So then move on over to the far right hand column of this chart and check out the adverse effects commonly associated with these medications. Whew, that’s a long list!
And we’re not necessarily talking insignificant adverse effects, either.
These include potentially impactful effects like low blood pressure - is your patient going to experience syncope? Dizziness and sedation - will your patient be able to function taking these meds on a daily basis?
So essentially we have a list of medications that’s not reeeeeeally targeted for migraines AND we have a plethora of potentially harmful side effects.
Fantastic.
You’re welcome, all you 80s babies. (Image)
But until recently, these were kinda what we had to work with, which brings us to the new kids on the block (NKOTB). The CGRP antagonists.
As of writing this post, there are 3 CGRP antagonists on the market:
Ok, I lied. There’s actually a 4th CGRP inhibitor, ubrogepant (Ubrelvy), but it’s only indicated for acute treatment of migraines rather than prevention. Since this post is more about chronic migraine prevention, this medication is only gonna get this quick shout out.
Also, if you’re wondering whether I had a finger spasm and typo’d all those weird letters after the generic names, check out our quick guide to biosimilars.
As for the first 3 medications on that list, let’s take a closer look:
What’s the evidence for CGRP inhibitors in chronic migraine prevention?
Erenumab
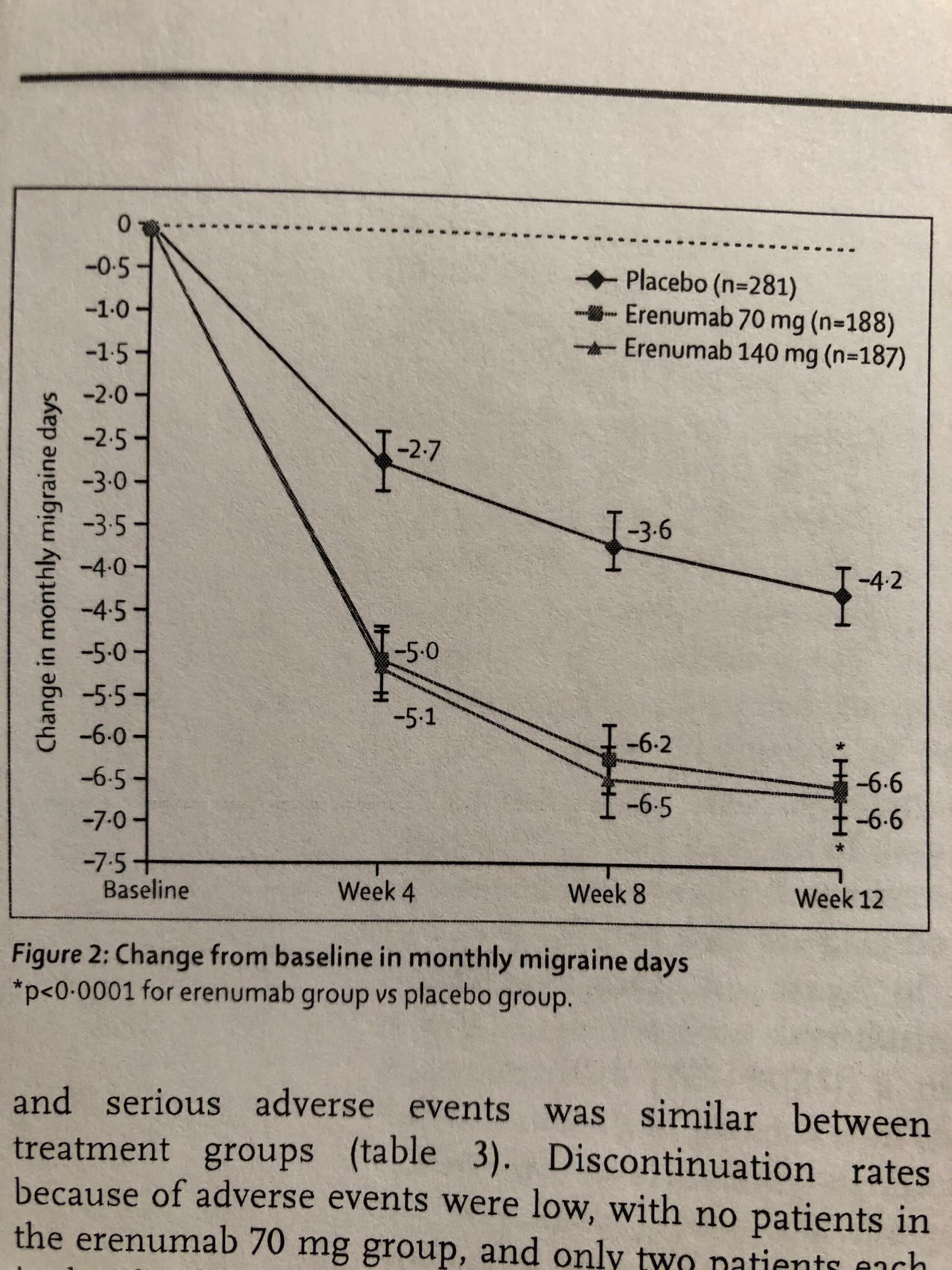
In this 2017 Lancet phase 2 trial, erenumab was compared with placebo in 667 mostly female, middle-aged, Caucasian patients with chronic migraine, which was defined for this study as >15 headache days per month including at least 8 migraine days. This was a randomized, double-blind, multicenter study conducted in North America and Europe. There were 3 arms with decently balanced baseline characteristics: placebo, erenumab 70mg, and erenumab 140mg, each given every 4 weeks for 12 weeks. The investigators were trying to assess the change in monthly migraine days experienced by patient, as well as assess the safety of this medication.
How did investigators get the information about change in migraine days? Not exactly something one can objectively measure with lab tests or imaging.
It was actually based on a headache diary. Now I don’t know about you, but I’m terrible at journaling or keeping a diary. I can barely remember to take my multivitamin every day (and my poor vitamin D is severely neglected). And I’m a pharmacist! So what kind of results would this study have gotten in the general population…
Trick question. They didn’t necessarily include the general population. They included patients who showed at least 80% compliance with keeping a daily electronic headache diary during a screening phase. So these were pretty on the ball, self-aware patients.
It also didn’t necessarily represent the general population since they excluded people who started having migraines after the age of 50 and those who had failed more than 3 other classes of migraine prophylaxis. They also excluded patients with fibromyalgia and poorly controlled hypertension. So these were also the more refractory cases without some potentially confounding disease states, although patients with continuous headache pain were also excluded.
Overall, it seems like they wanted to capture the group of patients who were bad enough to have tried a 1-2 different prevention strategies but not so bad off as to never have relief from migraines. And these were patients who were pretty aware of their headaches and cognizant of keeping a diary about symptoms.
So what did they find?
(Image)
Both doses of erenumab significantly decreased monthly migraine days by about 2-3 days compared with placebo, although it should be noted that the most pronounced/statistically significant differences were in the last 4 weeks of the 12 week study period.
Both doses of erenumab also had a significantly greater chance of producing a 50% or greater reduction in monthly migraine days compared with placebo. Erenumab use reduced the number of days patients had to use acute migraine relief treatments.
Yay! We pharmacists like to use less drug when possible!
Interestingly, even though monthly migraine days were significantly improved with erenumab, the secondary measure of cumulative monthly headache hours was not.
Makes you wonder about that diary and how accurately these patients recalled their symptoms and recorded them. (Let’s be real - if you are having photophobia from a migraine, do you really want to log onto a bright computer and log your symptoms?)
Safety-wise, numbers of adverse events were very low with the most commonly reported event being injection site pain (still only 4% of patients). Other reported side effects included constipation and muscle spasms (both more with the erenumab 140mg dose). No patients withdrew due to a serious adverse event.
In summary, this study provided the basis for considering erenumab in a treatment-refractory migraine population, albeit one without some confounding comorbidities. It’s also encouraging to see the reduction in use of other acute migraine relief products, which may help with alleviating medication overuse headache. It is, however, a little thought-provoking to consider how the use of the diary and the reduction in days but not hours may be interpreted. It will also be important to counsel patients that the greatest benefit may not be seen until they are 2-3 doses into treatment.
And then there’s always cost. Remember, this is a -mab, so it’s gonna be pricey… to the tune of ~$7000 per year without insurance. This is definitely an area where we pharmacists can help our patients navigate affordability and resources - if they meet criteria for trying this medication!
Fremanezumab
In this 2018 NEJM article, two doses of fremanezumab were compared with placebo in 1130 mostly middle-aged females with chronic migraine (same definition as the erenumab trial). This was a randomized, double-blind, multicenter study conducted in the slightly wider net of North America, Europe, and Asia. There were 3 arms: fremanezumab quarterly (aka patients received one dose in this 12 week treatment study period), fremanezumab monthly (3 injections total), and placebo.
Baseline characteristics were relatively balanced across the groups, although the fremanezumab quarterly cohort did seem to have slightly more historical experience with onabotulinumtoxinA (Botox). Despite this, that group didn’t seem to necessarily exhibit more severe disease, at least as far as number of headache or migraine days at baseline (~13 and 16 per month, respectively, across all three arms).
A third of included patients were also allowed to continue one other migraine prevention therapy as long as they had been stable on it for at least 2 months. Like the erenumab study, the primary outcome being assessed was the mean change in the average number of headache days, as reported in an electronic daily diary.
So at least at this point, when comparing to the erenumab study, we’re looking at a similar population of middle aged female patients here with a similar headache severity as assessed by migraine days/month at baseline, although perhaps the decreased number of headache days overall in this study compared to erenumab could indicate a slightly less severe cohort?. The duration of study treatment was 12 weeks in both studies. So this was not necessarily an expansion in study population or indication.
But what did they find? Anything new or different for the CGRPs?
Both fremanezumab groups reduced the mean number of headache days per month by about 2 compared with placebo, although interestingly the placebo group also had a reduction from baseline by about 2 days. Makes you wonder about heightened patient awareness for taking baseline preventative medications simply from being enrolled in a study, doesn’t it…
Fremanezumab also decreased the number of migraines reported per month compared with placebo, and the active drug groups also had greater percentages of patients achieve a 50% reduction in headache days per month. So not only were absolute numbers of headaches and migraines lower in the fremanezumab groups, but they also achieved this milestone significantly more often.
Skeptical Dog isn’t sure where fremanezumab fits either based on this data. (Image)
Interestingly, they reported the average number of headache days per month in patients NOT receiving concomitant preventative meds, but what about the third of patients who WERE receiving other prevention? Why didn’t they report that, since it may have provided information about use of fremanezumab as an adjunctive rather than solo therapy!? Which would probably have helped guide real life a little more… Although perhaps they didn't have quite as impressive of numbers in that already-treated cohort.
In terms of safety, patients in the fremanezumab monthly group had significantly more adverse events compared with placebo, although most were considered to be minor (most common = injection site reaction in about 25-30% of patients).
There was this nagging question of LFT elevations…but the differences between active drug and placebo were not statistically significant. Potentially a good monitoring point to log away for the future though, especially if a patient has some baseline hepatic disease or multiple hepatically-cleared medications.
So where does that leave us after learning about fremanezumab?
Personally, I dunno that fremanezumab offers much on top of erenumab. In studies, they both reduced headache and migraine days similarly compared with placebo, they’re injections dosed at similar intervals, and they both have a handful of notable adverse effects, although fremanezumab with those questions of liver enzymes and higher rates of injection site reactions perhaps sticks out a smidge more. They’re both expensive. So, perhaps between the two, i’d reach for erenumab…
But what about galcanezumab?
Galcanezumab
So this brings us to the last new injectable CGRP inhibitor for chronic migraines. Because the study design is really quite similar, we’re just going to highlight the big stuff for this one.
In this 2018 study in Neurology, galcanezumab was compared to placebo in just over 1100 mostly middle-aged female Caucasian patients with chronic migraine (same definition as before). Included areas were North and South America, Europe, and Asia, so just a little wider net than previously. Baseline headache history and previous preventative treatments were similar in terms of headache/migraine days and number of other meds tried and failed.
Patients could remain on topiramate or propranolol prevention if they’d been stable for at least 2 months, although only 15% of included patients stayed on concomitant therapy for the full study. The investigators did limit opiate, barbiturate, and corticosteroid use this go around. So essentially, they got increasingly more clear about concomitant therapies for the galcanezumab study, but as part of this, it may be difficult to assess the CGRP inhibitor as an adjunctive rather than a replacement therapy.
(Although perhaps we want to use it as a replacement! Less is hopefully more with medications, right?)
The primary outcome was still the mean change in monthly migraine headache days from baseline over the course of 12 weeks. There were still 3 arms: placebo, galcanezumab 120mg, and galcanezumab 240mg. Data was still based on an electronic daily diary.
Feel like you’ve fallen into a time warp from 10 paragraphs ago, yet?
They did do a boatload more patient-focused questionnaires at their follow up visits to assess functionality and quality of life measures. So there, that’s something different.
(Image)
Oooo…here’s a new number!
Oh wait, nope.
Both galcanezumab doses significantly reduced monthly migraine days by about 2 days per month compared with placebo, although again the placebo group had a reduction in the primary endpoint of about 3 days all by itself. And given not that many patients were taking concomitant preventative therapies, it is even more difficult to interpret that decrease here! Placebo effect?
Galcanezumab also achieved greater rates of 50 AND 75% responses, and the investigators considered improvements in functionality and quality of life scores to be clinically meaningful.
It’s also important that the statistically significant differences in headache days between placebo and active drug, regardless of galcanezumab dose, was apparent even after 4 weeks. No waiting until month 3, as with erenumab!
Adverse event rates were low, with injection site pain being the most commonly reported (but only ~6-7% here…not the 30% seen with fremanezumab!). One patient in the high dose galcanezumab group had elevated LFTs, but ONE only. So 0.4%. Again, not the multiple patients noted with fremanezumab - although those numbers were still pretty low (~1%).
So, now where do we stand on the CGRP inhibitors?
To use a CGRP inhibitor or not?
After looking at these studies, it seems as though there are several takeaway points about using these new medications:
The CGRP inhibitors were really studied in a specific subset of patients:
Refractory and frequent, but not continuous, migraines
Failure of at least a couple of other preventative medications, including topiramate but not usually onabotulinumtoxinA
Fairly severe disease with around 20 headache days/month (and about 18-19 migraine days/month)
Most patients were 40-something year old white females. So it’s as yet a bit unclear whether these medications are applicable or safe in other populations. Use with caution.
When choosing between the 3 available CGRP inhibitors based on the clinical data, it seems as though galcanezumab offers similar efficacy to the other 2 in terms of headache reduction AND it shows that benefit earlier in the treatment course (by week 4 rather than week 12).
BONUS, it seems to have fewer adverse effects, although patients should still be counseled about injection site pain and reactions.
We still need to consider cost vs benefit when we’re talking about an average reduction in headache days of about 2 per month. For some people, maybe that’s worth the cost of the medication. For others, especially depending on insurance coverage, maybe not.
Patients would need to be willing to use an injectable medication.
Given the studies didn’t include high numbers of patients taking other preventative medications, it’s as yet unclear what the benefit of a CGRP inhibitor is when used on top of other therapies. Should these be adjunctive therapies or replacement?
The CGRP inhibitors may have a role in reducing acute migraine treatment utilization. We’re pharmacists, so if we can get away with less medication entering the system, that’s better! Especially considering what we suspect about medication-overuse headache these days.
You may also want to check out the American Headache Society’s 2018 position statement about how to make heads and tails of all these new treatment options here.
Thanks for coming with me on this chronic migraine and CGRP inhibitor ride! I hope it’s been as useful for you as it was for me to review this topic, and I look forward to learning together again in the near future. (I mean, I only name-dropped onabotulinumtoxinA in this post… It could - and may - be an entire future headache post!)