What Every Pharmacist Should Know about Chronic Care Management (CCM)
Steph’s Note: This week, we have the pleasure of welcoming a new voice to the site. Carley Moses, PharmD, graduated from VCU/MCV School of Pharmacy in 2021 and has been finding creative ways to incorporate clinical skills into her retail pharmacy practice since then! She works in the same community pharmacy where she had her first job as a cashier at 15, and she has experience in community, compounding, health system, and academic pharmacy. Talk about well-rounded! For funsies, she’s also a dog and cat mom, wife, tv-binger, and coffee shop addict. She’s passionate about advocacy, expansion of pharmacy access to the underserved, collaboration, and tacos.
When someone starts talking about a golden win-win opportunity, like CCM. (Image)
What is Chronic Care Management (CCM)?
So, you want to get into more clinical care as a pharmacist? Maybe you thought about creating your own pharmacy consulting business? Perhaps you always dreamed of working alongside or even in the office with another practitioner?
Well then do I have the opportunity for you!! Meet my lovely friend…Chronic Care Management.
Chronic Care Management (CCM) is a program offered to Medicare beneficiaries with 2 or more chronic conditions that are expected to continue at least 12 months, or until death.
But wait…that sounds like…everyone?
Correct. Most Medicare beneficiaries will fall into the “big 3” triad: hypertension, hyperlipidemia, and diabetes. Only 2 of those 3 are needed to qualify for CCM, and that doesn’t even take into account other chronic conditions, such as dementia, asthma, COPD…and the list goes on.
It’s important to note that CCM is NOT a collaborative practice agreement (CPA). CCM does NOT provide the authority needed to order labs or to initiate, change, or stop therapy. However, CCM trials are a great first-step to a CPA implementation! By providing CCM services to these patients, you will provide recommendations for guideline-directed therapy changes; engage with patients regarding diet, lifestyle, vaccination, and screening recommendations; and assist with coordination of care in the community.
Now that we know who our CCM patients are, who else is involved in implementation?
Partnering with a Prescriber for CCM
First, you’ll have your Qualified Healthcare Professionals, aka your homies with prescribing authority. These are typically physicians, physician’s associates/assistants, and nurse practitioners, etc. If they can write a prescription, they can enroll their patients in CCM. It is the prescriber’s responsibility to consent the patient for entry into the CCM program, either verbally or written. It’s also their responsibility to maintain documentation of the patient’s consent and comprehensive care plan in their electronic health record (EHR).
Since I brought up the EHR, let’s hang out here for a moment. It is REQUIRED that the practitioner implement the CCM services in an EHR. This is to ensure that the comprehensive care plan that I mentioned a minute ago can be securely delivered to the next person involved…YOU!! Whether you decide to implement your services in the same building as the physician, or in a community pharmacy like I did, the care plan can be shared to you via fax or electronic prescription from the EHR.
You and your prescriber-BFF, working towards a common goal…be it better patient care or simply running together with giant sticks. (Image)
After you provide your services to the patient, you will transmit any notes or documentation back to your prescriber in whatever means works best for them. They may give you access to the EHR to directly document your encounters, or you may use a secure fax or electronic mail to return your documentation, ensuring it gets placed in the patient’s EHR for billing.
So, your practitioner-BFF found your first couple of eligible patients, has obtained their consent, and is about to send you your first comprehensive care plan. What can you expect in that plan?
Most care plans consist of the following…
An updated problem list
Outcomes/prognosis
Treatment goals
Symptom management
Planned interventions
Medication management
Community service orders
Coordination of services
Periodic review of care plan
Sounds like a lot, right?
Really, it’s not so bad! And you can actually make your BFF’s life easier by creating a standardized template for them to complete during the consenting process that covers most of these considerations. Check out my example here:
This would be the document faxed to you, providing you with guidance for this patient’s specific disease states and goals. You would then review this care plan with the practitioner at whatever intervals you decide to ensure you’re working towards the same goals.
What does a CCM visit with a pharmacist entail?
Whoa there, Jerry, calm down. We’re getting to it. (Image)
As you begin to plan your visits, it’s important for us to discuss the different kinds of CCM visits and length requirements to ensure you get $$paid$$ for your brilliant clinical services. Medicare breaks CCM down into two categories: complex and non-complex.
The non-complex CCM patients require a minimum of 20 minutes to bill for reimbursement. In addition, you may also bill an additional 20 minutes for the same patient a total of twice, for a grand total of 60 minutes of service per calendar month. These are the patients who do not have significant changes or implementations to their care plans from month to month.
On the other hand, complex CCM patients are those who have had significant changes, such as therapy changes, or newly diagnosed disease states, that require additional time and effort. They require at least 60 minutes of care to bill for reimbursement. Like non-complex CCM, you may also bill for an additional 30 minutes of service once, for a grand total of 90 minutes of service per calendar month.
What should you do during visits?
That’s up to you, your patient, and their practitioner! Typical services that I provide during CCM visits include medication reconciliation, medication synchronization, guideline-directed therapy recommendations, vaccinations, screening for and coordination of preventative services such as eye or foot exams, and lifestyle recommendations/education.
As your patients visit each month, you’ll begin to learn their strengths and weaknesses and will be able to adjust accordingly to help them reach their chronic condition goals. Sometimes this looks like helping them to implement a written blood pressure or blood glucose log they can take back to their practitioner to make more informed therapy changes.
(And because you’re a super skilled CCM pharmacist, I bet you will already have recommended those changes to the practitioner within your note! Makes their life easier, right?)
Setting Up Your CCM Program for Success
When talking about recommendations, it’s important to remember that this isn’t a CPA. Depending on your practitioner, your recommendations may or may not be taken. This is where it’s important for you as the pharmacist to communicate clearly with your practitioner regarding what feedback you would like in order to make the CCM program as effective as possible.
This could look like you going to their office once a week to do a debrief and lab review together, or maybe you all communicate feedback through the EHR as you review each other’s notes. Regardless, it is important to be clear about where you will place your recommendations, what feedback you would like to receive, if any, and how you would like to receive that feedback. Every practitioner is different, and it’s up to you to be transparent in the amount of discussion you would like to have around your recommendations. Be confident - if they let you come this far, they trust you!!
I’m sure you’re wondering how these CCM visits fit in your busy day as a pharmacist – especially if you, like me, call a community pharmacy home. This is where it’s important to communicate with your manager and practitioner-team regarding the number of patients you have, time requirements, as well as expectations of you outside of CCM. For example, in my community pharmacy, I am still responsible for medication synchronization, vaccine administration, and medication reviews throughout the week.
When planning my week, I communicate 1-2 half or full days to my manager and practitioner-BFF that they can expect me to be solely working on CCM tasks. This amount varies based on the number of patients I have and the work required for these patients. This work includes note writing, the visits themselves, scheduling, making referrals, and any other clerical tasks I may need to complete related to the program.
This provides clear expectations for when your practitioner, patient, and manager can expect you to be reachable regarding CCM matters. If a patient were to come in or call unexpectedly, everyone involved knows the dedicated days and times to direct the patient to help when you are available. This creates structured boundaries for the remainder of your work week.
Oh, and did I mention that TELEHEALTH counts for CCM?? That’s right! If you’re having a busy month or the coverage isn’t quite there, you can complete your 20 minutes of CCM over the phone.
How profitable is CCM?
Now that we have all the logistics down, let’s talk moolah. This will be your big selling point for your practitioner-BFF as well as your manager. CCM serves as an excellent means to not only increase their Medicare star ratings but also to earn passive income from your visits. When pitching the concept to your manager, be sure to emphasize the improvement in star-ratings for your pharmacy, as well as the potential increase in prescription volume.
You’re right, Michael, CCM is! (Image)
CCM is also an excellent bridge to providing MTM services, vaccines, clinical screenings, and medication synchronization services for profit. Your pharmacy will not only profit from the visit itself as I’ll discuss in a few, but for each patient, it may also receive a medication review reimbursement, 2-3 vaccine reimbursements, and anywhere from 2-20 medications synchronized each month. In addition, there will be a steady influx of dedicated patients and prescriptions, as your practitioner-BFF will also probably want you handling the dispensing of your patients’ medications.
When approaching your manager with this information, I recommend having a draft of which practitioner(s) you have in mind, a sample comprehensive care plan, a sample schedule or workflow for review, as well as a sample contract draft, including the length of your services and how you would like to negotiate billing.
As you are discussing implementation with your practitioner-BFF, you should discuss who will be responsible for the billing of your services. (Remember, you want to get $$paid$$.) Typically, this task is assigned to the physician’s office that is providing the services, with you, the pharmacist, providing your times and billing codes each month.
Once your billing person is designated, you should negotiate at what rate you want to be paid. Personally, my pharmacy started with a 50%/50% profit share. The practitioner’s office staff billed my hours each month based on the CPT codes included in my notes, and I invoiced their office for 50% of whatever Medicare paid. It is important to note that, if the patient is solely enrolled in Medicare, they may have a copay for these services. It should be established if the practitioner’s office will collect these copays, or if you would only like to screen for dual Medicaid and Medicare eligible patients to avoid any cost for patients.
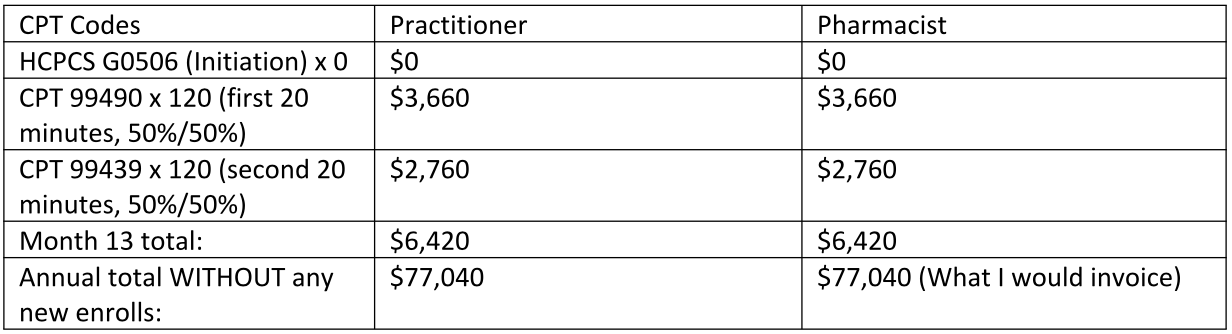
Below are the appropriate CPT codes to include with your notes for your billing staff, based on the complexity and amount of time spent with the patient. Of note, HCPCS G0506 is only billable for the visit in which the practitioner enrolls the patient. I typically don’t negotiate this reimbursement into my billing because this is an additional $60 incentive for the practitioner to consent patients and provide you with care plans!
Let’s play out the math here for a better illustration.
So, let’s say in your first month your practitioner-BFF consents 10 patients into your new CCM program. You see each of these patients for 40 minutes this month for their initial visit and medication review.
Now, let’s say that same BFF sends you 10 patients each month for the remainder of the year, bringing you to 120 patients by month 13, when you plan to do your annual medication reconciliation and plan review. Your month 13 breakdown would be:
So if you can gain 10 patients per month for 1 year, you AND your practitioner-BFF could profit ~$77,000 during year 2 – not counting any Medicare star bonuses!
Other than the money, why start a CCM program?
What good love story is complete without a happy ending? CCM has personally provided me with more fulfillment than I ever imagined. I’ve been able to share such comforting moments with my patients. As the pandemic progressed, I was able to serve as an immediate contact for all virus-related questions during a scary time.
In one instance, a patient referred to me had a blood pressure of 220/100+ (yowsers, right?!). I was able to recommend therapy, and his systolic blood pressure is now in the 130-140s. We repeated labs and used those new numbers to show him the improvement in his kidney health, as well as improvements in his ASCVD risk. These visits and interventions have motivated him to be one of my most adherent patients.
And they rode off into the sunset and lived happily ever after. That kind of happiness! (Image)
Ahhhh… pharmacy happiness!
My relationships with my patients have grown to open, honest ones in which they feel comfortable discussing aspects of their personal and social lives with me. This allows me to then advocate for them with their practitioners to receive the most holistic care possible. It is so fulfilling and empowering to watch people as they learn how to care for themselves!
The tl;dr of CCM for Pharmacists
Overall, CCM can be a win-win for you as an autonomous pharmacist and for your practitioner friends looking to improve their patient care. It increases collaborative trust, and your recommendations could be the next step to your first collaborative practice agreement! CCM is an excellent way to increase patient engagement, while also increasing Medicare star ratings and income for both the pharmacy/pharmacist and the practitioner involved.
The program can seem daunting to initiate at first glance, but here’s the quick break down:
Your prescriber-BFF will identify a patient with 2 or more disease states enrolled in Medicare.
They will consent the patient to seeing you, fill out their checklist for a care plan, and send it to you, the pharmacist, through the EHR.
You will schedule, see, and write notes for the patients referred to you and return said documentation back to your BFF’s office for billing.
Office billing will submit your codes and time monthly as they do their normal office billing.
You can invoice the office for your payment.
So essentially, all that is needed of the practitioner is the consent and care plan, as well as the additional billing services that are already being done within the office. The planning, scheduling, and implementation of the program would not interfere with your practitioner’s day at all. Rather, it would run simultaneously in the background, increasing touch points for their patients and decreasing the amount of material they need to cover within their own visits.
So, what are you waiting for???
Go find your favorite practitioner and begin your sales pitch for why YOU should be the improvement they make for their patients in 2023!!