The Pharmacist's Introduction to Burns Resuscitation
Steph’s Note: I love it when we have experts willing to share their brain with us at tl;dr - especially when it’s about a topic that isn’t really covered in the usual pharmacy school curriculum. What a treat to have this knowledge at our fingertips from people who work it firsthand!
This week is no exception. Dr. Josef Nissan is back yet again (check out his literal compendium of previous posts, including most recently sodium bicarbonate in cardiac arrest and SIADH), and this time he’s here to teach us about burn patients. Now you may be thinking that you’re not going to work at some ginormous health care institution with a burn center so you won’t ever need to know this stuff, but as you’ll see, there are definitely nuggets that any pharmacist can take away from this topic. Teach us, Joe!
Oh, and for all of you worried about gruesome pics with this topic, take comfort and read on. I didn’t use any because I do actually want you to learn the material rather than getting grossed out and clicking off this site. For those of you lookie loos who like working in the ER, Google at will on your own!
“Somebody call 911, shawty fire burnin on the dance floor” - Sean Kingston
A monumental and life changing lyric by the king, Sean KINGston himself. Well then, are you comfortable resuscitating shawty who is indeed burning on the dance floor? If you aren’t, keep on reading.
Between 2009 and 2014, over 3 million emergency department visits were for burn related injuries. While these patients may not get admitted at your facility (unless you’re a certified burns center), there is a very high chance that the initial resuscitation phase occurs in your emergency department. So, let’s get you prepared with the pharmacotherapy needed for initial burn resuscitation.
Burn Types & Classification
I’m sure a house fire is the first thing that comes to mind when you hear about burn-related injuries. But believe it or not, there are multiple types of burns that aren’t related to flames. These different types of burns include:
(Image)
Thermal Burn: burns secondary to an external heat source (e.g., flames, scalding liquids, hot metals, steam)
Fun fact, the first burn case I ever saw was a patient with diabetic neuropathy who was standing in boiling water trying to fix his hot water tank in the attic…
Radiation Burn: burns secondary to prolonged exposure to ultraviolet rays (e.g., sun, X-ray machine)
Chemical Burn: burns secondary to strong acids, alkalis, detergents, or solvents (e.g., sulfuric acid, hydrochloric acid, lime)
Electrical Burn: burns secondary to an electrical current (e.g., alternating current, direct current)
Burns are further classified by degree depending on the depth of skin surface penetration. Obviously, the deeper the burn, the worse the outcomes.
(Image)
First-degree (superficial) burn: effects on the epidermis (outermost layer of the skin)
Second-degree (partial thickness) burn: involves the epidermis and part of the dermis
Third-degree (full thickness) burn: involves the epidermis and complete dermis
Fourth-degree burn: involves both layers of the skin and underlying tissues, possibly including muscle and bone
Calculating the Total Body Surface Area (TBSA) Affected
As we will talk about later, estimating the total body surface (TBSA) affected is crucial in determining appropriate resuscitation measures. The easiest and fastest way to calculate a quick estimate of the TBSA involved is by using the Wallace Rule-of-Nines. The rule-of-nines assigns body surface area to each of the major body parts below:
(Image)
Let’s use an example. Patient AA was brought into your ED by ambulance following a house fire. On examination, it appears the entire abdomen, back, and both legs were severely burned. To get an estimated TBSA, add 9% (entire abdomen), + 18% (entire back) + 18% (left leg) + 18% (right leg) = 63% TBSA. Simple, right?
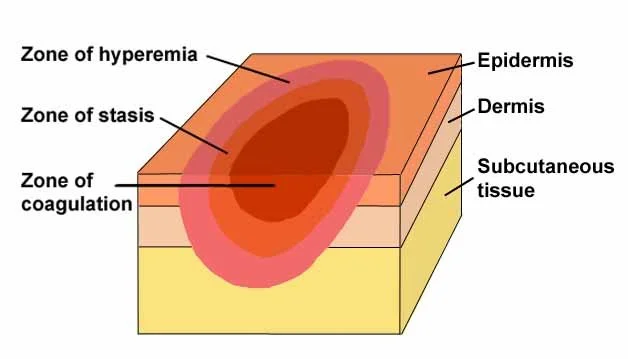
Pathophysiology of Burns (AKA Jackson’s Burn Model)
To understand the pharmacological treatments used in burns resuscitation, we must first understand the pathophysiology. As described by Douglas Jackson in 1947, when skin is exposed to excess heat, formation of three zones follows:
(Image)
Zone of Coagulation: occurs at the point of maximum damage. Irreversible tissue loss is experienced in this zone.
Zone of Stasis: surrounding tissue experiences decreased perfusion. Tissue in this zone is potentially salvageable as long hypoperfusion is quickly reversed.
Zone of Hyperemia: outermost zone tissue perfusion is increased. Tissue here will generally recover unless there is severe sepsis or prolonged hypoperfusion.
At the endothelial level, damage to the skin triggers several inflammatory responses including the increased release of nitric oxide synthase. Increase in nitric oxide causes vasodilation and massive capillary leakage into the interstitial space. This mass capillary leakage results in hypovolemic shock. If not quickly reversed, patients will develop multi-organ failure and death.
Pharmacological Treatment of Thermal Burns
Since the majority of burn cases are caused by thermal burns, we will primarily focus on the initial resuscitation of thermal burns. As with any trauma, our initial focus is on stabilizing the airway, breathing, and circulation (ABC’s).
Starting with “Airway”, burn patients are at an increased risk of upper airway and inhalation injury - specifically, carbon monoxide and cyanide poisoning. Let’s discuss.
Carbon Monoxide Poisoning
Carbon monoxide is one of the most frequent immediate causes of death following inhalation injury. Let’s simplify this a little to make it easier to understand. I’ll start by painting a picture for you.
When carbon monoxide sees your hemoglobin molecules, occupied by oxygen or not. (Image)
Boom. House fire erupts. Where there’s fire, there’s smoke (thank you, 1st grade science). Well, smoke contains a byproduct called carbon monoxide. Carbon monoxide is a colorless, odorless gas with an affinity for hemoglobin more than 200 times greater than that of oxygen.
Take a moment for that figure. Carbon monoxide wants to bind to your hemoglobin at least 200 times more than oxygen. That’s insane. So what happens when it does bind to hemoglobin?
Excess serum carbon monoxide kicks oxygen off hemoglobin and saturates red blood cells with carbon monoxide instead of oxygen. With minimal to no oxygen bound to hemoglobin, your tissues experience hypoperfusion and eventual death.
Carbon monoxide poisoning should be suspected in ALL patients who present following inhalation injury or house fires until it is excluded by a normal blood carboxyhemoglobin level. I repeat. Carbon monoxide poisoning should be suspected in all patients who present following inhalation injury or a house fire. And yes, it can ONLY be diagnosed by collecting a blood carboxyhemoglobin level.
REMEMBER THIS. You CANNOT use pulse oximetry since pulse oximetry does NOT differentiate carboxyhemoglobin from oxyhemoglobin. So your pulse oximetry may say that someone’s oxygen saturation is 99% even though their true oxyhemoglobin level is under 50%.
Sign & Symptoms: Highly dependent on the blood carboxyhemoglobin level.
The higher the level, the more severe the symptoms. In general, patients with mild to moderate carbon monoxide poisoning will present with headache, dizziness, weakness, upset stomach, vomiting, and confusion. Severe carbon monoxide poisoning may present in a comatose state.
Treatment: Hyperbaric oxygen
Mechanism of Action: Inhaling pure oxygen (100% oxygen) helps speed up the replacement of carbon monoxide with oxygen in your blood.
Treatment Criteria: In general, patients should be treated with hyperbaric oxygen if they meet the following criteria:
Carboxyhemoglobin level >25% (>15% if pregnant)
Patient has layered mentation or is comatose
Severe metabolic acidosis is present
Evidence of end-organ ischemia
Cyanide Poisoning
The other common inhalation injury is cyanide poisoning. Let me paint another picture for you.
Boom (again). House fire erupts (again). Fire is hot. Hot melts household items. When these products (especially plastic) are burned, a byproduct called cyanide is released. Cyanide is a colorless gas with the odor of bitter almonds.
Long story short (because the nitty gritty details aren’t that important right now), excess cyanide causes cessation of aerobic metabolism due to the depletion of ATP in the mitochondria. Lack of aerobic metabolism means your tissues aren’t getting oxygen. Without oxygen, you die. That was as simple as I could explain it.
Signs & Symptoms: Initial symptoms are generally nonspecific. Majority of patients will present with headache, anxiety, confusion, and abdominal pain. Severe cyanide toxicity can lead to seizures and coma.
First-line Treatment: Hydroxocobalamin
Mechanism of Action: Hydroxocobalamin binds to cyanide in our blood stream, converts it to cyanocobalamin (that’s right, vitamin B12), which is then excreted in the urine. *Okay, but how cool is that? This antidote literally converts a harmful toxin in our body to a vitamin. It’s turning the joker into a superhero. Pretty neat if you ask me!*
Adult Dosing: 5 g (IV/IO) as a single infusion over 15 minutes; may repeat a second 5 g dose over 15 minutes to 2 hours (total dose: 10 g), depending on the severity of poisoning and clinical response.
Second-line Treatment (only to be used of hydroxocobalamin is unavailable): Sodium Nitrite (3% solution) and Sodium Thiosulfate (25% solution)
Mechanism of Action: both of these agents work similarly to hydroxocobalamin. They bind to cyanide, free up cytochrome oxidase, and allow aerobic metabolism to continue.
Adult Dosing:
Sodium nitrite (3% solution): 10 mL IV (300 mg) at 2.5 to 5 mL per minute; may repeat once
Sodium thiosulfate (25% solution): 50 mL IV (12.5 g) immediately following sodium nitrite administration; may repeat once
Clinical Disclaimer: Hydroxocobalamin should ALWAYS be used when available. Since sodium nitrite and sodium thiosulfate are falling out of favor, the majority of hospitals carry hydroxocobalamin. Only use 2nd-line treatment options when hydroxocobalamin is absolutely not available.
Initial Fluid Resuscitation
Now that we’ve stabilized the “Airway & Breathing”, let’s move onto the “Circulation” portion of our ABC’s.
As we discussed earlier, during the first 24-48 hours following a major burn, patients have an increase in nitric oxide release, resulting in severe vasodilation and massive capillary leakage into the interstitial space. If left untreated, patients develop severe hypovolemic shock leading to anoxia and death.
Your fluid supply for burn patients. (Image)
Fluids. Fluids again. More fluids. This is the biggest theme of initial burn resuscitation. Given the severity of hypovolemic shock, you need MASSIVE amounts of fluid to reverse the shock and allow for tissue perfusion. And I mean MASSIVE.
How much exactly?
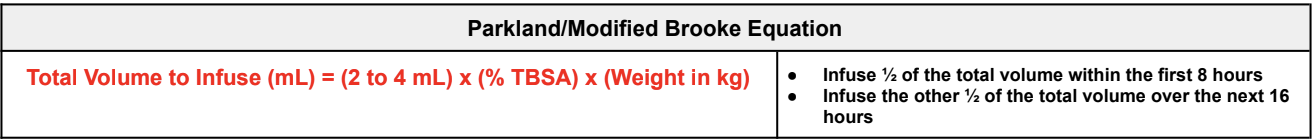
Thankfully we have a couple of easy equations we can use to help us determine the appropriate volume to be infused. Let me introduce you to the Parkland and modified Brooke formula. These equations can be used to determine the volume of fluid requirements during the initial 24 hours of resuscitation for adults with burns >20% TBSA.
Let’s try an example. A 48 year-old male (weight: 95.8 kg) is brought into your ED following a meth lab explosion and house fire (yes, I had to be dramatic). After physical examination, it appears the patient has suffered severe burns to the head, neck, chest, abdomen, and both arms.
First things first, we need to calculate the TBSA affected. Once we have that, all we need to do is plug and chug.
Calculate the TBSA:
9% (head & neck) + 9% (chest) + 9% (abdomen) + 9% (left arm) + 9% (right arm) = 45% TBSA
Since TBSA affected is >20%, patient qualifies for fluid resuscitation using the Parkland or modified Brooke Equation.
Calculate the Total Volume Needed to Infuse:
Total Volume to Infuse: 4 mL x 45% (TBSA affected) x 95.8 kg = 17,244 mL
First 8 hours: infuse 1⁄2 of the total volume within the first 8 hours; ~8.5 L (~1062.6 mL/hr).
Next 16 hours: Infuse 1⁄2 of the total within the next 16 hours; ~8.5 L (~531.3 mL/hr).
Not so bad right?
In terms of initial fluid selection, patients with moderate to severe burns should receive IV crystalloid solution, generally Lactated Ringers. Normal saline is typically avoided due to the risk of hyperchloremic acidosis that can occur with administration of large volumes of isotonic fluids.
Secondary Prevention
Awesome. So now we’ve stabilized the patients “Airway, Breathing, and Circulation” (ABC’s). The next and final step of initial burn resuscitation is secondary prevention.
First let’s talk tetanus. Make sure that burn patients are up to date on their tetanus immunization. If not, administer a tetanus shot for for any burn deeper than superficial-thickness (i.e., anyone with a 2nd degree burn or worse).
Next, what is our body’s first-line defense against harmful microbes? Yup, our skin! When you experience a deep burn, that defense mechanism is completely lost. So how do we prevent infection?
Topical antimicrobials. These should be applied in the emergency department, especially if there are delays in patient transfer. The most common topical antimicrobials used in burn patients include silver sulfadiazine, bacitracin, polymyxin B, and neomycin.
The tl;dr of Burns Resuscitation
That’s all folks. That right there is pretty much everything you need to know for the initial pharmacological management of burns. So now, are you more comfortable resuscitating shawty who is indeed burning on the dance floor? If you were too lazy to read this entire post, here is a tl;dr version (you’re welcome).
There are multiple types of burns, including thermal, radiation, chemical, and electrical. Burn are classified by degree depending on the depth of skin surface penetration, with classifications ranging from first-degree (superficial) to fourth-degree (possibly involving muscle and bone). Use the rule-of-nines to help estimate total body surface area (TBSA) affected.
Patients with major burns experience severe hypovolemic shock secondary to vasodilation and massive capillary leakage.