Diabetic Ketoacidosis: The ABCs of DKA
Steph’s Note: This week, we’re taking a ride back to one of our favorite tl;dr subjects: diabetes. If you didn’t already know from our posts on insulin and how to leverage it, oral anti-diabetic medications, insulin pumps, and yes, even a CHEAT SHEET, we love talking diabetes. And yet, something has been missing…
Which brings us here - diabetic ketoacidosis. Dr. Josef Nissan is here to save the day once again and fill a rather obvious gaping hole in our content by discussing this acute complication of diabetes using his critical care brain. He’s freakin’ amazing in his ability to take complex topics and make them way easier to understand than any lecture. (You don’t have to take my word for it - check out his previous posts on acetaminophen toxicity, vasopressors, and methemoglobinemia.)
Or you can start with this post - that works too. But I’ll bet you check out his others afterwards. Just sayin’.
Anyway, take it away for DKA!
Oh yes. I remember it like it was yesterday. My first PGY1 pharmacy residency interview. As if I wasn’t already nervous enough, they scheduled me to start the interview in the “clinical case” room. You know, where they give you clinical cases and ask you a million questions about pathophysiology, pharmacotherapy, clinical pearls, etc.
Yeah... It was a rough start.
Me, leaving my PGY1 pharmacy residency interview. (Image)
To make things worse, the first case they gave me was a DKA patient. I had a decent understanding of what DKA was, but I was absolutely clueless about insulin dosing, when to use sodium bicarbonate, which fluids to give, how much, etc. I left that room completely defeated and thought to myself, “Well, they for sure think I am an idiot.”
So put yourself in my shoes. Do you know everything you should about DKA? Pathophysiology, insulin dosing, fluid replacement strategies, potassium supplementation, when to use sodium bicarbonate, and so on?
If you can’t confidently answer all these questions, then stick around because I’m going to teach you EVERYTHING you need to know about the DKA.
P.S. Just to give you some encouragement, I actually ended up matching with that same hospital where I butchered the DKA case. So if you plan on doing a residency, don’t be so hard on yourself. Residency interviews are MUCH more than just your clinical knowledge.
Alright let’s start.
What’s the big deal with diabetic ketoacidosis (DKA)?
Diabetic ketoacidosis (DKA) is an acute, major, life-threatening complication of diabetes characterized by hyperglycemia, ketoacidosis, and ketonuria. DKA is characteristically associated with type 1 diabetes but can also occur in type 2 diabetes under extremely stressful conditions such as infection, trauma, cardiovascular emergencies, and certain medication use.
Fun fact, Klebsiella pneumoniae is the leading cause of bacterial infections precipitating DKA. Speaking of medications, the most common medications known to induce DKA include corticosteroids, antipsychotics, and pentamide.
If left untreated, DKA can cause potentially fatal complications, such as severe dehydration, coma, and swelling of the brain. Overall mortality rate for DKA is 0.2-2% with persons at the highest end of the range residing in developing countries.
Pathophysiology of DKA
I am going to simplify this as much as possible. Of course the pathophysiology of DKA is pretty complex, but we’re going to stick with the basics. If you want to dig deeper into the biochemistry of DKA and all of that junk…errr…stuff, please feel free to do so. But for my sanity, I will keep things more simple.
To start, what is the main source of energy in our body’s cells, tissues, and organs (especially the brain)?
Pizza = heaven. (Image)
Carbohydrates. I love carbs. Pizza, bread, fries, pasta, and so much more. And what does our body break carbohydrates down into? Yup, you guessed it. Glucose.
Glucose is the main source of energy in our bodies. Without glucose, we’d all be dead. So let’s say I eat a full KitKat bar. All that sugar (aka glucose) is going to pass through my GI tract to be absorbed into my bloodstream. Now that it’s in my bloodstream, I need INSULIN to help transfer that glucose from my bloodstream into my cells. Once the glucose is taken up into my cells, my body can now use that glucose as energy (aka for ATP formation). Without insulin, glucose continues to hang out in my blood unable to be utilized for energy. No energy means cell damage and eventual death.
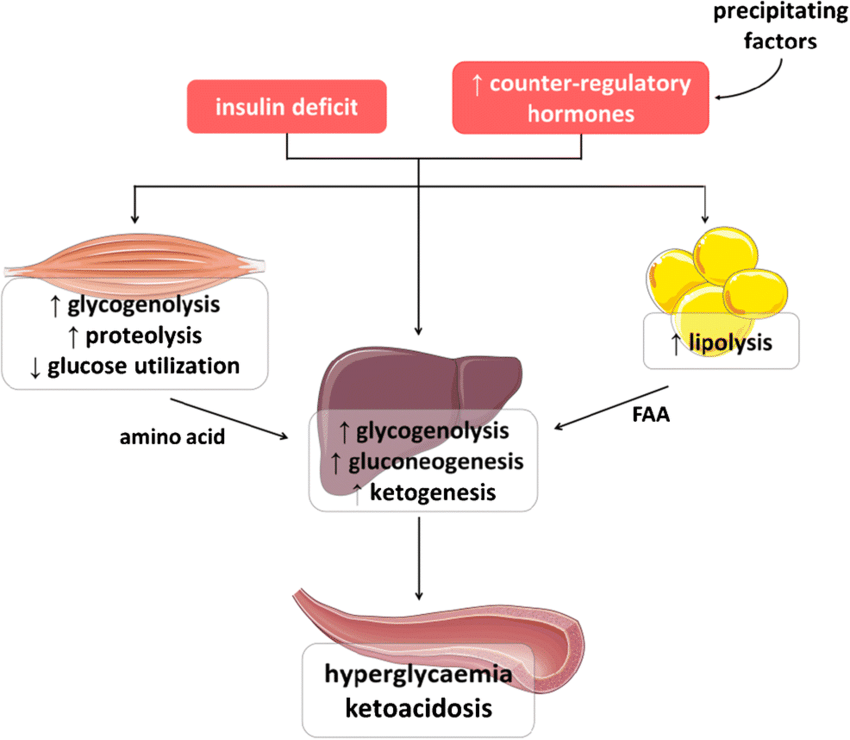
Now that we’ve reviewed the basics of endogenous insulin, let’s chat about the pathophysiology of DKA. DKA occurs as a consequence of absolute or relative insulin deficiency that is accompanied by an increase in counter-regulatory hormones, such as glucagon, cortisol, growth hormone, and epinephrine.
This hormonal imbalance enhances hepatic gluconeogenesis, glycogenolysis, and lipolysis. Pause.
These sound like super fancy scientific words, but don’t let them confuse you. More simply defined, they’re all mechanisms that our bodies use in order to compensate for the lack of glucose uptake into the cells secondary to endogenous insulin deficiency. Let’s review what these fancy shmancy words really mean.
Hepatic gluconeogenesis: the process of making glucose from other macronutrients, specifically proteins.
Compensatory Purpose: Due to the lack of glucose uptake into the cells, our body starts converting proteins into glucose. This new glucose is meant to be removed from the serum and used by cells for energy.
Negative Effect: Leads to worsening hyperglycemia.
Glycogenolysis: the biochemical pathway in which glycogen is broken down into glucose.
Compensatory Purpose: Just like gluconeogenesis, our body wants to increase serum glucose since the cells are experiencing a lack of glucose uptake secondary to absolute or relative insulin deficiency.
Negative Effect: Leads to worsening hyperglycemia.
Lipolysis: the breakdown of fats and other lipids by hydrolysis to release fatty acids to be used as energy.
Compensatory Purpose: Lack of insulin → cells can’t uptake glucose for energy → body breaks down fats as the new main energy source → release of fatty acids.
Negative Effect: Breakdown of free fatty acids releases an acidic byproduct known as ketones. (Yes, this is why it’s called diabetic ketoacidosis.)
When accumulated ketones exceed the body’s capacity to extract them, they overflow into the urine (ketonuria) and blood (ketonemia) causing severe metabolic acidosis (ketoacidosis) and electrolyte abnormalities. Ketoacidosis leads to muscle wasting, renal failure, altered mental status, hyperpnea, and death.
That, my friends, is the basic pathophysiology of DKA.
(Image)
Signs and Symptoms of DKA
Dwight knows how serious DKA is too. (Image)
The most common early symptoms of DKA include increased thirst (polydipsia), increased urination (polyuria), and dehydration. These symptoms typically present secondary to prolonged hyperglycemia.
Glucose is an osmotic diuretic, meaning it causes increased urination. Increased urination means dehydration and increased thirst in order to help compensate for the excess volume loss.
Other signs and symptoms associated with DKA include:
Malaise
General weakness
Nausea, vomiting, abdominal pain, anorexia
Altered consciousness
A thorough physical examination may be positive for:
Dry skin and mucous membranes
Decreased skin turgor
“Fruity Breath” - characteristic acetone (ketotic) breath odor
Tachycardia and hypotension
Hypothermia
Tachypnea
Confusion/Coma
Classifying DKA
DKA is characterized by ketonemia, ketonuria, high anion gap metabolic acidosis (pH < 7.30), hyperglycemia (serum glucose > 250 mg/dL), and a serum bicarbonate level < 18 mEq/L. Furthermore, DKA can be classified as mild, moderate, and severe. Let’s review.
Mild DKA
pH 7.25-7.3
Serum bicarbonate 15-18 mEq/L
Anion gap > 10
Moderate DKA
pH 7.0-7.24
Serum bicarbonate 10-14 mEq/L
Anion gap > 12
Severe DKA
pH < 7.0
Serum bicarbonate < 10 mEq/L
Anion gap > 12
How is DKA diagnosed?
There are multiple tests to consider when diagnosing DKA. We just talked about how DKA is characterized by ketonemia, ketonuria, high anion gap metabolic acidosis, hyperglycemia, and low serum bicarbonate. Therefore, our diagnostic approach is to either rule in or rule out these different DKA characteristics.
So how can we do that?
Lab tests, of course! Below are common laboratory tests that are critical in the diagnosis of DKA:
Treatment of DKA
When treating patients with DKA, our treatment goals include normalizing fluid-volume status and correcting hyperglycemia, electrolytes, and ketoacidosis. To do so, we must follow a step-wise approach that focuses on:
Correction of fluid loss
Correction of hyperglycemia
Correction of electrolyte disturbances (especially potassium)
Correction of acid-base balance
Treatment of underlying DKA trigger (if present)
So how do we correct all that? Well, I am awfully generous and made an algorithm table that goes over the step-wise approach of treating DKA. Let’s look below:
BTW - You can get an algorithm like this, plus algorithms and treatment pearls for dozens of other medical emergencies in our Acute Medical Emergencies Pocket Guide
The tl;dr of Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is an acute, major, life-threatening complication of diabetes characterized by hyperglycemia, ketoacidosis, and ketonuria. DKA is characteristically associated with type 1 diabetes but can also occur in type 2 diabetes under extremely stressful conditions, such as infection, trauma, cardiovascular emergencies, and certain medication use.
DKA occurs as a consequence of absolute or relative insulin deficiency that is accompanied by an increase in counter-regulatory hormones such as glucagon, cortisol, growth hormone, and epinephrine. This hormonal imbalance enhances hepatic gluconeogenesis, glycogenolysis, and lipolysis.
Lipolysis results in the breakdown of free fatty acids and release of acidic byproducts known as ketones.
Increased serum ketones leads to high anion gap metabolic acidosis, leading to potential muscle wasting, renal failure, altered mental status, hyperpnea, cerebral edema, and death.
DKA can be classified into mild, moderate, and severe DKA depending on blood pH, serum bicarbonate level, and anion gap.
Common symptoms associated with DKA include polydipsia, polyuria, dehydration, malaise, general weakness, nausea/vomiting, abdominal pain, and altered consciousness. Numerous laboratory tests should be collected to help in the differential diagnosis of DKA.
Treatment goals of DKA include normalizing fluid-volume status and correcting hyperglycemia, electrolytes, and ketoacidosis. When treating DKA, always follow a step-wise approach that focuses on:
Correction of fluids
Correction of hyperglycemia
Correction of electrolyte disturbances
Correction of acid-base balance
Treatment of underlying DKA trigger (if present)
Always utilize IV regular insulin dosed at 0.1 units/kg bolus, followed by 0.1 units/kg/hour as a continuous infusion to help correct hyperglycemia and increase the uptake of glucose into the cells to promote the inhibition of further lipolysis. Closely monitor potassium levels and supplement as necessary. IV bicarbonate should only be utilized in cases of severe DKA when the pH < 6.9.
And there you have it - DKA in a nutshell!