The tl;dr Pharmacy Journal Club: Sodium Bicarbonate Use in Out-of-Hospital Cardiac Arrest
Steph’s Note: Ahhh, you know we love journal club here at tl;dr. You also probably know it’s been a little while since we’ve had a really good, deep literature dive. Seriously, was the azacitidine journal club the last one?!? Eepers, we’re dropping the ball. (Although, I mean, we’ve had some pretty sweet content since then, so don’t be too mad at us, mmmk?)
Luckily, we know someone who loves journal club just as much as we do AND likes writing awesome critical care articles for us! Happy day. So please welcome back Dr. Josef Nissan, who (much like our recent oops-we’ve-been-doing-this-incorrectly-for-years post on vancomycin AUC dosing) is going to dispel some myths on the ubiquitous amp of bicarb during codes. Take it away, sir!
(Image)
Let’s admit it. We’re all guilty. I know I am. You’re pulling medications during a code when you’re tasked with the infamous, “We need an amp of bicarb, stat.” You probably have no idea why the team wants it, but nonetheless, you pull that amp of bicarb out, prepare it, and hand it to the nurse for administration.
I mean, come on, every single crash cart has multiple amps of sodium bicarbonate (when it’s not on shortage!). So clearly there’s an indication for it, right?
Well, not always.
To understand the role of sodium bicarbonate in out-of-hospital cardiac arrest, we must first understand the pathophysiology of this life-threatening emergency. During cardiac arrest, the body experiences global ischemia, which leads to:
Loss of membrane integrity
Increase of inflammatory mediators
Increased release of interleukin-1B and TNF-alpha leading to microvascular thrombosis, loss of vascular integrity, edema formation, and apoptosis
Lactic metabolic acidosis
Increase in anaerobic metabolism given lack of tissue perfusion, resulting in the release of lactate and lactic acidosis
Respiratory acidosis
Apnea during cardiac arrest results in increased CO2 retention leading to respiratory acidosis
Adverse Effects of Acidosis
Clearly, as stated above, cardiac arrest leads to both metabolic and respiratory acidosis. And yes, acidosis has numerous harmful effects on our bodies including…
Decreased cardiac output
Arterial dilation with hypotension
Altered oxygen delivery
Decreased ATP production
Predisposition to arrhythmias
Impairment of immune responses
Compromised anticoagulation
So then, what’s the potential role of sodium bicarbonate in cardiac arrest? Simple. Administering bicarbonate should reverse the respiratory and metabolic acidosis, thus (hypothetically) leading to:
Increased cardiac output
Prevention of arterial dilation and hypotension
Protection against further cardiac arrhythmias
Increased ATP production and reversal of tissue damage secondary to the lack of oxygen delivery
Sodium Bicarbonate - The Negatives?
This is us, taking the magic school bus to chemistry 101. (Image)
I know. So far it seems like I am doing a pretty poor job arguing against the use of bicarbonate for out-of-hospital cardiac arrests. I sure am making bicarbonate seem like a hero drug. But every “hero” drug comes with a laundry list of negatives as well. So what are the negatives of sodium bicarbonate use in cardiac arrest?
Simple.
To get a better understanding of the negatives of bicarbonate, we need to take the magic school bus back to chemistry 101.
What does sodium bicarbonate get broken down into in our bodies? Let’s take a look:
So where’s the harm? When we administer sodium bicarbonate (aka NaHCO3), one of the byproducts released is carbon dioxide (aka CO2). Increased serum CO2 secondary to sodium bicarbonate administration can lead to:
Worsening respiratory acidosis
Increased intracellular ion shifts, leading to hypokalemia
Worsening risk for hypernatremia and acute kidney injury
Increased risk of metabolic acidosis
Also, let’s not forget that an amp of sodium bicarbonate is hypertonic. As a matter of fact, one ampule of 8.4% sodium bicarbonate has about the same osmolarity as 6% NaCl (that’s right, about twice as hypertonic as 3% NaCl).
Evidence-Based Medicine
Enough of me blabbing on and on about sodium bicarbonate use for out-of-hospital cardiac arrest. Let’s review factual evidence-based literature…starting with the 2020 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
Believe it or not, the 2020 AHA guidelines recommend against the routine use of sodium bicarbonate for patients in cardiac arrest. If you don’t believe me, here’s the literal screenshot of the guidelines to prove it!
Furthermore, the AHA guidelines state, “No new evidence exists to show that routine administration of sodium bicarbonate improves outcomes from undifferentiated cardiac arrest and evidence suggests that it may worsen survival and neurological recovery.”
Ouch.
If that’s not convincing enough, let’s review the primary literature that led to this AHA recommendation.
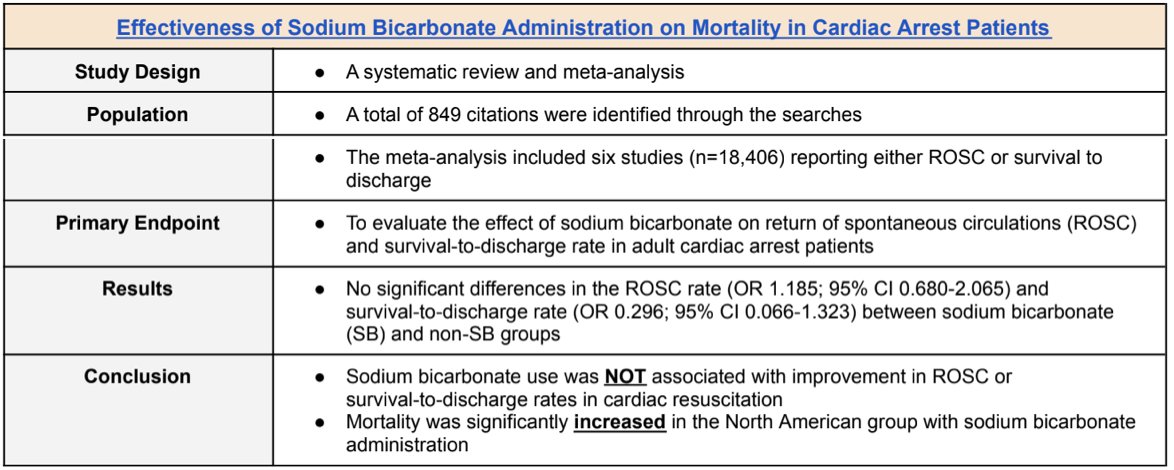
(Image)
Not convincing enough given the small population size? Okay, let’s take a look at another study.
(Image)
So far, we can all agree (along with the AHA guidelines) that older primary literature has NOT shown improvement with achieving ROSC, neurological outcomes, or survival when using sodium bicarbonate for cardiac arrest. Additionally, there may actually be an increased risk of mortality in North Americans that receive sodium bicarbonate during cardiac arrest.
Let the Journal Club Begin
Alright, enough with older literature. Let’s review literature that came out after the 2020 AHA Guidelines publication.
Alshahrani MS, Aldandnan HW, et al. published a systematic review and meta-analysis in International Journal of Emergency Medicine titled “Use of sodium bicarbonate in out-of-hospital cardiac arrest (OHCA).” The purpose of this study was to assess the effect of sodium bicarbonate on the survival rate to hospital discharge, ROSC, and good neurological outcomes at discharge in patients with OHCA.
Inclusion and exclusion criteria were as follows:
Whew. That was a lot of words and this is tl;dr. So I made this table that gives a brief summary of results between the sodium bicarbonate and control groups.
Based on these results, the authors concluded that current evidence demonstrated that sodium bicarbonate was NOT superior to the control group in terms of survival to discharge and return of spontaneous circulation (ROSC). Further, sodium bicarbonate was associated with lower rates of sustained ROSC and good neurological outcomes.
Clinical Applicability - the tl;dr version
Have I convinced you to put that bicarb away for out-of-hospital cardiac arrests? We must practice evidence-based medicine and follow guideline recommendations that recommend against the routine use of sodium bicarbonate for patients in cardiac arrests.
Let’s make it our responsibility to educate our providers with new literature so that we continue to provide the safest and most efficacious therapy. In conclusion, if you were too lazy to read the specifics of this post, here is the tl;dr version of everything you need to know about sodium bicarbonate use in out-of-hospital cardiac arrest:
(Image)
Given the AHA guideline recommendations and newly published primary literature, the routine use of sodium bicarbonate for out-of hospital cardiac arrest is NOT recommended.
Sodium bicarbonate use for cardiac arrest has NOT shown benefit with improving survival to discharge or achieving return of spontaneous circulation (ROSC).
Furthermore, use of sodium bicarbonate in cardiac arrest may be associated with worsened neurological outcomes and decreased rates of sustained ROSC.
Sodium bicarbonate should ONLY be administered for cardiac arrest in the setting of hyperkalemia or sodium channel blocker overdose (e.g., tricyclic antidepressants).