When Antidiuretic Hormone Malfunctions: The ABCs of SIADH
Steph’s Note: In our last post from Dr. Josef Nissan, he tackled the harmful effects associated with electrolyte deficiencies and how to properly replace certain electrolytes from an inpatient perspective. (If you haven’t read that post, check it out here!) So of course we have to keep the electrolyte theme going because who doesn’t love it when a provider asks you to verify an order for hypertonic saline stat. Take it away, Joe!
How you feel the first time you see an order for hypertonic saline in your verification queue. (Image)
I’m pretty sure I pooped my pants the first time I verified a hypertonic saline infusion for a patient with SIADH. Speaking of SIADH, I guess we can start talking about it now.
SIADH stands for Syndrome of Inappropriate Antidiuretic Hormone. However, that sounds kind of boring and honestly a little bit confusing because what exactly does the word “inappropriate” mean? Too much antidiuretic hormone (ADH) secretion is inappropriate but so is too little… Point proven.
So the more fun way (aka the Joe way) to remember SIADH is as “Such Immense Antidiuretic Hormone.” Now that’s more self-explanatory and is easier to remember. IMO. Before we dive into everything you need to know about SIADH, let’s review some background information that will really help clear up the pathophysiology of this disease state.
The Role of Antidiuretic Hormone (ADH)
Imagine this. You’re at Disney World. It’s 110°F out, and you’re sweating nonstop. It’s been over three hours, but the rollercoaster line doesn’t seem to be moving any faster. To make matters worse, your mouth's as dry as the Sahara Desert because you refuse to spend $18 on an 8 oz. bottle of water (ridiculous, I know).
Where am I going with this, you ask?
To combat dehydration, one of our body’s compensatory mechanisms is the increased release of antidiuretic hormone (ADH). ADH floats in our bloodstream until it reaches our kidneys where it agonizes vasopressin-2 (V2) receptors. This results in increased water retention and decreased urination.
Increased water retention in the kidneys leads to:
Increase in blood dilution
Decrease in blood osmolality
Increase in blood volume
Increase in blood pressure
Pathophysiology of SIADH
So then, what exactly is SIADH? Simply put, it’s a medical condition that results when our bodies secrete excess ADH despite normal or increased blood volume. The hallmarks of SIADH include hyponatremia, low blood osmolality, and high urine osmolality. (Basically, it’s diluted blood and concentrated urine, which makes sense when you consider the body is holding onto more fluid rather than peeing it out.)
One important thing to note is that this type of hyponatremia is the result of excess water retention rather than a deficiency of sodium. Think of an empty cup with 1 teaspoon of salt (solute). As you pour more water (solvent) into that cup, you’ll have a decreased concentration of salt per kilogram of fluid (decreased osmolality). Same thing happens in our blood.
As ADH release increases, there’s an increase in water retention, leading to an increase in blood volume and a decrease in our blood osmolality.
This mechanism is the cause of hyponatremia. Make sense? Cool.
Signs & Symptoms of SIADH
Signs and symptoms of SIADH are heavily dependent on the severity of hyponatremia. Depending on the serum sodium level, some patients may be asymptomatic, while others may exhibit more severe musculoskeletal and neurological symptoms.
Hyponatremia can be classified according to the serum sodium concentration:
Etiology of SIADH
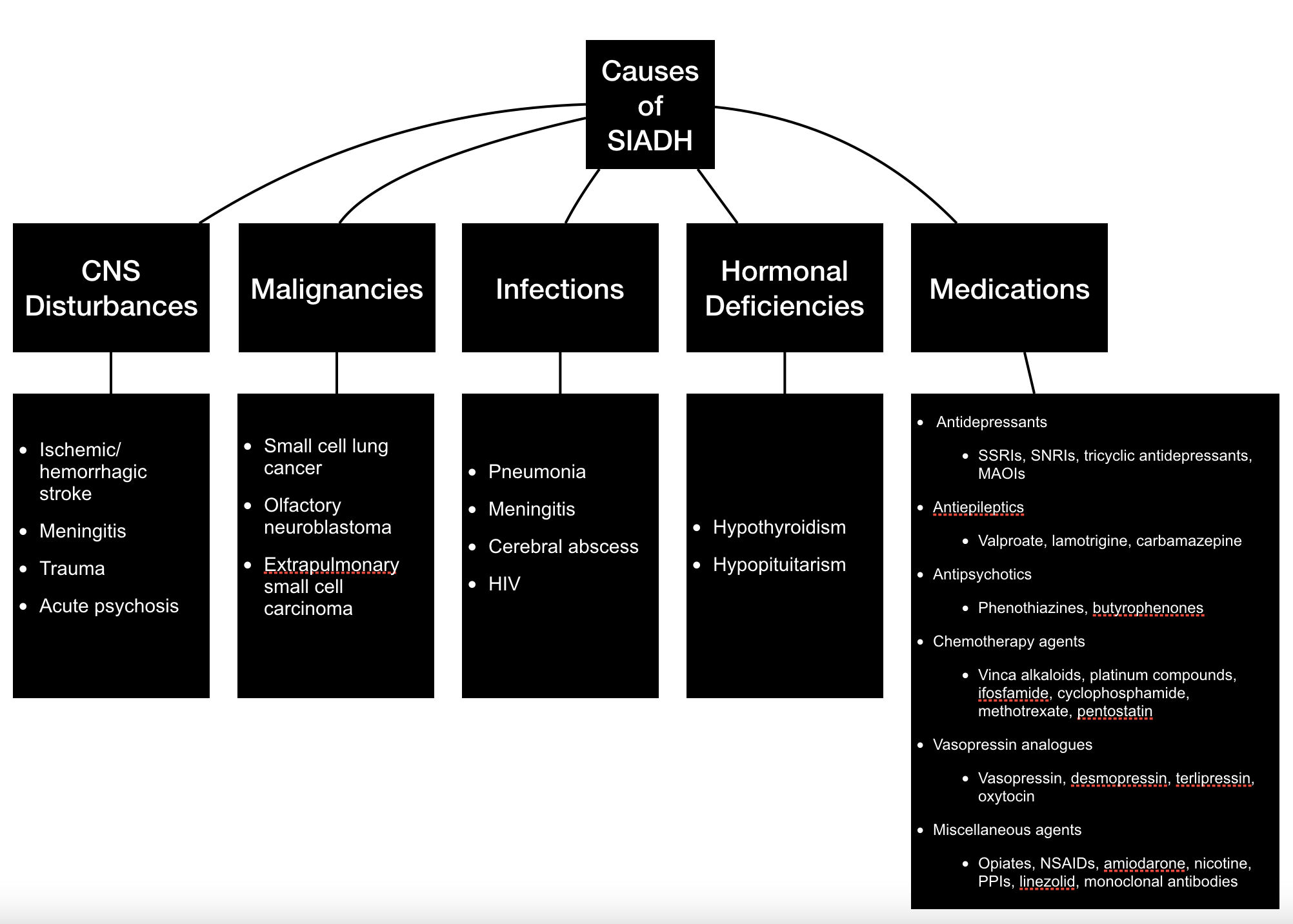
Just like with most disease states, there are numerous causes of SIADH. Check out the figure below to learn some of these etiologies, paying special attention to that right hand column noting medications (we are pharmacists after all!).
Diagnosis of SIADH
Dr. House diagnoses. But for the love of Pete, could they not have put a pharmacist on the team? Or at least consulted one for the screen writers?? (Image)
As pharmacists, we should always make it our responsibility to be the drug experts on any medical team. While we typically don’t diagnose, I highly encourage every clinician to familiarize themselves with medications known to induce SIADH. This will help expedite potential diagnosis and treatment as well as prevent future readmissions.
Other than a great medication reconciliation, additional exams and findings that are used for the diagnosis of SIADH include:
Fluid status
Patients with SIADH are generally euvolemic or hypervolemic.
If dehydration is present (aka hypovolemia), assess for alternative causes of hyponatremia.
Basic metabolic panel
Hyponatremia (Na <135 mmol/L) is present in patients with SIADH.
Plasma osmolality
Low plasma osmolality (< 275 mOsm/kg) is present in patients with SIADH.
Urine tests
Urine osmolality
High urine osmolality is present in patients with SIADH.
Urine sodium
Urine sodium must be elevated in patients with SIADH (Urine [Na+] > 40 mmol/L).
Imaging
Chest X-ray and/or CT of the chest may be utilized to rule out other causes of SIADH, including pneumonia and small cell lung cancer.
Thyroid panel
May be utilized to rule out other causes of SIADH including hypothyroidism.
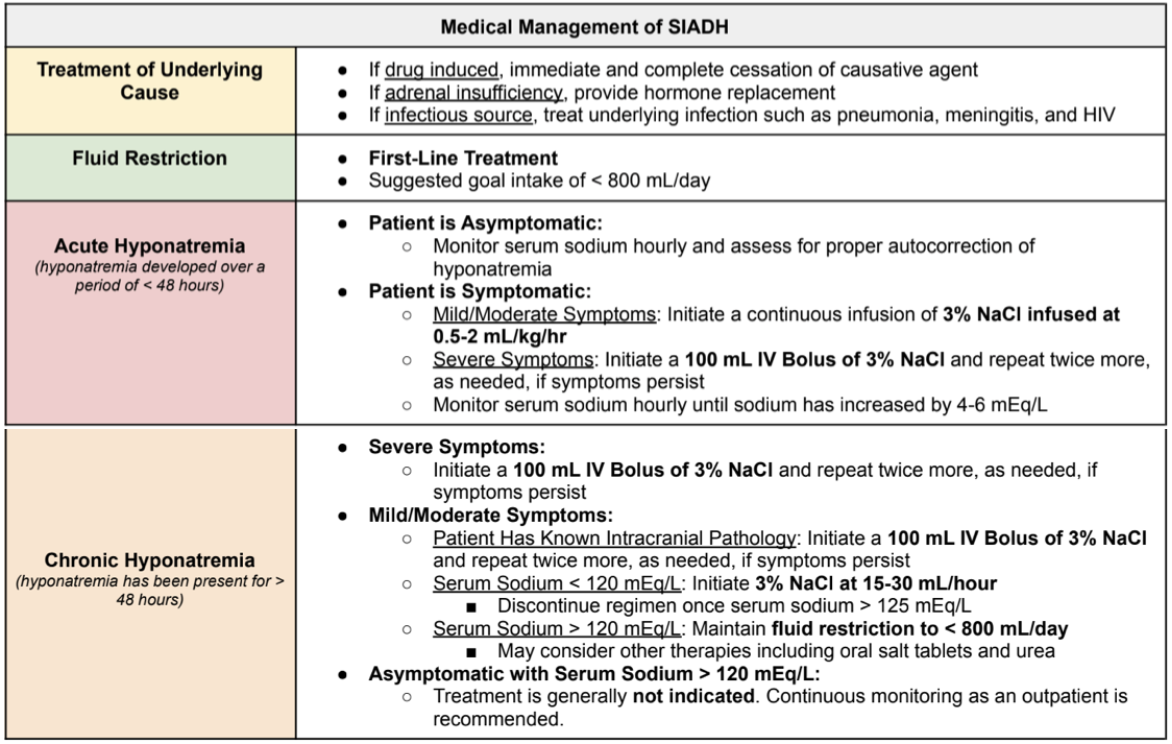
Treatment of SIADH
Management varies depending on the underlying cause of SIADH as well as the severity of hyponatremia. In general, our goals for SIADH treatment include:
Treatment of the underlying cause
Correcting hyponatremia
Prolonged therapy in patients with persistent SIADH
The Role of Vasopressin Receptor Antagonists in SIADH
I know what you’re thinking. What about -vaptans? Don’t those have a role in SIADH? When should we start those?
The deal with vaptans and SIADH just isn’t quite this easy… (Image)
Ugh, I really wish it was that easy!
Unfortunately, vaptans (aka vasopressin receptor antagonists) are fairly new and have not been established as a mainstay of therapy for every case of SIADH. Nonetheless, they may have a clinical benefit in certain SIADH cases. Let’s review.
On paper, vasopressin receptor antagonists sound like miracle drugs for the treatment of SIADH. As we stated earlier, SIADH is caused by the excess release of ADH, which then binds to vasopressin-2 (V2) receptors in the kidneys, resulting in water retention, hyponatremia, low blood osmolality, and high urine osmolality. So in theory, giving a vasopressin receptor antagonist should help block ADH from binding to the V2 receptor.
Voila, SIADH is cured, right!? Well, kind of.
Newer randomized controlled trials have shown that vasopressin receptor antagonists are more effective than placebo for raising serum sodium in SIADH patients. However, most of the patients included in these trials were asymptomatic or mildly symptomatic with an average serum sodium of 127 to 131 mEq/L. Clearly these mildly hyponatremic asymptomatic patients aren’t the ones that we usually worry about.
Additionally, these studies showed that vasopressin receptor antagonists only increase serum sodium by a small margin of ~ 1 to 5 mEq/L. So given their lack of use in moderate-severely symptomatic patients and their minimal increase in serum sodium, vasopressin receptor antagonists aren’t a first-line treatment option for SIADH.
So should we never use them? Not necessarily.
Generally, each institution will have differing restrictions on the use of vasopressin receptor antagonists. However, vasopressin receptor antagonists may be considered for refractory hyponatremia in patients who…
Have CHRONIC hyponatremia (NOT recommended for the treatment of acute hyponatremia)
Have failed fluid restriction
Have a serum sodium <125 mEq/L
Have a plasma osmolality of <285 mOsm/kg
Have moderate/severe symptoms and are resistant to fluid restriction
Do NOT have hypovolemic hypotonic hyponatremia or signs of dehydration
Are NOT anuric
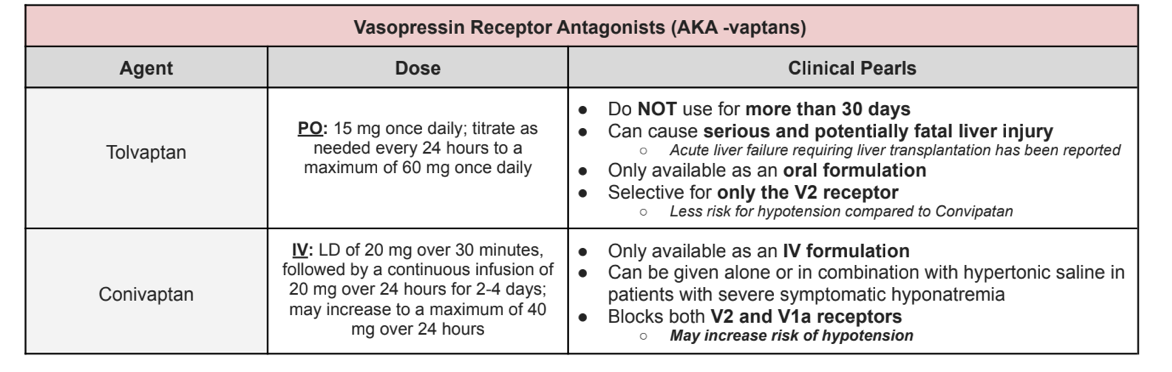
Yeah lol. There are a lot of restrictions on vasopressin receptor antagonists. They’re really not the miracle drugs that they seem to be. But if you do ever have a patient that fits the criteria for vasopressin receptor antagonists, use the table below to decide between the potential agents.
Maximum Rate of Correction
Contrary to popular belief, this is not an otherworldly monster. It’s an artist’s depiction of how terrifying osmotic demyelination actually is. (Image)
Ahhh yes. Osmotic demyelination. (Ominous booming music cues.) We’ve all been scared straight into making sure we never overcorrect hyponatremia. Why?
Because this really bad thing can happen called osmotic demyelination. Here’s the deal. If you correct sodium too rapidly, it can lead to the destruction of the myelin sheath covering the nerve cell in the middle of the brainstem. This can be FATAL. So please don’t correct sodium too fast. A good rule of thumb is this:
Maximum correction rate: 8 mEq/L in any 24-hour period
An initial rate of correction of 4-6 mEq/L in the first 2-4 hours may be beneficial in patients with severe symptoms.
The tl;dr of SIADH
SIADH is a medical condition that results when our bodies secrete excess ADH despite normal or increased blood volume. The hallmarks of SIADH include hyponatremia, low blood osmolality, and high urine osmolality. Signs and symptoms of SIADH are heavily dependent on the severity of hyponatremia. There are lots of potential causes of SIADH, but for us pharmacists, we should be aware that many of these are medications! And we’re talking common medications too, including antidepressants, antipsychotics, and antiepileptics. So have your eagle eye on the medication list when you see a low sodium on the BMP.
When treating SIADH, we want to make sure we not only address the current hyponatremia but also try to prevent future episodes by targeting any identifiable underlying causes and/or using medical management for persistent cases. Management of a current episode usually starts with fluid restriction, an assessment of symptom severity, and investigating whether it’s an acute versus chronic issue (which can sometimes be difficult to establish, fun fun). When needed, pharmacologic management includes 3% hypertonic saline, vasopressin receptor antagonists (aka the vaptans), salt tablets, and urea.
Vasopressin receptor antagonists are usually reserved for patients with severe refractory symptomatic hyponatremia and may be given alone or in combination with hypertonic saline. Tolvaptan is only available as an oral formulation and should NOT be used for more than 30 days given hepatotoxicity risk. Conivaptan is only available as an IV formulation and is known to block both V2 and V1a receptors, leading to increased risk of hypotension.
And last but certainly not least, REMEMBER THE MAXIMUM RATE OF CORRECTION: 8 mEq/L in any 24-hour period to lower risk of osmotic demyelination!