Acid - Base Disorders: Essentials for Pharmacists
A note from the tl;dr team: This content was reviewed and updated in November 2025 to ensure accuracy and relevance
I have a confession to make...
I didn't "get" acid-base disorders until well after pharmacy school. They were something I was willing to skate through. To take an "L" on the exam if I had to.
This was an unnecessary stance. Acid-base stuff isn't that hard once you crack the code.
And while I'm far from an expert now, I know enough to get by.
But, there are people who know a lot more than me about acid-base. And thanks to the wonderful world of networking (and working in the same building), I know some of those people.
So, recognizing my limitations, I asked for help. I asked some excellent colleagues who are smarter than me.
What results is the post you're about to read. After reading it, I'd like to think that you'll have your acid-bases covered (do you see what I did there?) for most test, NAPLEX, and practice scenarios.
You might need to dig a little deeper if you specialize in critical care, but this should serve as a nice overview either way.
Acid-Base Pathophysiology
They seem complex on the surface, but acid-base disorders aren't all that complicated. Like most areas of medicine, it's best to learn the fundamentals by starting with the pathophysiology.
And once you get the fundamentals down, you'll find that most acid-base disorders don't require the use of complex math formulas or nomograms.
So let's start with the patho. What actually determines acid base status? What are the players involved?
Obviously, there’s pH. Remember from biochem that pH is a way of measuring the concentration of hydrogen ions. It's an inverse and logarithmic scale. What does that mean?
Low pH = high hydrogen ion concentration
High pH = low hydrogen ion concentration
That covers the "inverse" part. Logarithmic means that a small change in pH is actually a large difference in hydrogen ion concentration. Moving from a pH of 7 to a pH of 8 is a 10-fold difference in hydrogen concentration.
At the end of the day, pH is the actual ‘thing’ that determines if something is acidic or basic. Luckily, we can measure the pH of a patient's blood directly and get some essential info for our workup.
But what drives the pH of your blood?
There’s a lot of enzymes and chemical reactions involved. But even so, your blood pH is determined by the balance of only two metabolic products:
Carbon dioxide (CO2) and bicarbonate (HCO3).
The levels of (and balance between) carbon dioxide and bicarbonate play in a beautiful symphony (usually Beethoven's 9th) that determines blood pH.
When levels of carbon dioxide get too high, an acidosis eventually develops. When bicarbonate gets too high, an alkalosis develops.
Before we move on, let’s cover a few quick definitions…
Acidosis = a process that leads to an abnormally low pH
Alkalosis = a process that leads to an abnormally high pH
Acidemia = an acidosis of the blood
Alkalemia = an alkalosis of the blood
Notice the very similar (yet different) definitions for acidosis/alkalosis vs acidemia/alkalosis.
Your body is pretty complex (citation needed).
It can actually have a number of things going on at a given point in time that result in a local acid-base disorder.
For example...
Overdosing on opioids can cause respiratory depression (i.e. your breathing gets slower and shallower). Slower and shallower breathing cause carbon dioxide to accumulate (because you exhale carbon dioxide).
And as we learned above, increased CO2 leads to acidosis. Specifically here, you’d have a “respiratory acidosis.” There are too many hydrogen ions in your respiratory system.
That’s an acidosis. Not an acidemia.
Acidemia refers specifically to the pH of your blood. It’s sort of like the “sum total” of all underlying acidosis and alkalosis processes in your body.
For now, just know that an acidosis or alkalosis can lead to an acidemia or alkalemia.
In practice, you'll find that acidosis and acidemia are often used interchangeably. The same is true for alkalosis and alkalemia.
This is technically incorrect. As we’ve learned above, there is an important difference in the definitions.
For the purposes of an exam, make sure you know the difference between the terms. Once you start practice, recognize that either may be used (and the attending probably won't like you very much if you correct her all of the time).
I dare you. Say "it's actually an acidemia" ONE more time... (Image)
Normal Ranges
Blood pH: 7.35 – 7.45
pCO2 (mm of mercury): 35 – 45
Bicarbonate (mmol/L): 22 - 28
Regarding the normal ranges above, you may see slightly different numbers depending on your institution. Everyone’s lab equipment is calibrated differently, so check the accepted ranges at your place of practice.
A normal blood pH is 7.4, but we generally consider it acceptable if pH is between 7.35 or 7.45 (7.4 +/- 0.05). And thanks to the magic of science, your body is incredibly good at keeping pH in that range. It can correct most imbalances before they become problematic.
How does the body keep everything in check?
There are “buffers” in the blood that make it resilient to pH changes.
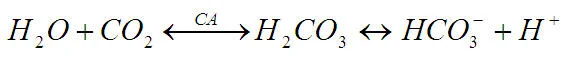
You've probably come across this equation that describes the activity of Carbonic anhydrase:
Carbonic anhydrase is one of the major players in your buffer system. It keeps your blood pH remarkably stable.
On top of that, your body “compensates” if a local system gets out of whack. This ensures that the system as a whole (your blood pH) stays in that 7.35 – 7.45 range.
More on compensation in a bit...
Problems occur when you get out of range. If blood pH dips below 7.35, you have an acidemia. If it’s above 7.45, you’ve got alkalemia.
If this pH range seems small, it is. But think back to your high school chemistry class. You learned there that chemical reactions are extremely sensitive to pH. And remember again that pH is a logarithmic scale (did I mention it's a logarithmic scale?).
A seemingly small change in pH is actually quite a large one. And it's enough to derail many chemical reactions.
"Derailed" chemical reactions in a body are bad news. Chemical reactions are how your body survives and gets things done.
All of the "stuff" happening in your body is either caused by or influenced by chemical reactions. Heart beats, DNA synthesis, urine formation...pretty much everything.
So what happens to a patient with an acidemia or alkalemia? In mild cases, it might just be vomiting, lethargy, and confusion. In the worst cases, you'll see heart arrhythmias, respiratory failure, seizures, and death.
Bad stuff all around.
Anion Gap
Before getting into the nitty gritty of diagnosing acid-base disorders, we need to understand the Anion Gap.
The anion gap is the difference in electrical charge between the cations (positively charged ions) and anions (negatively charged ions) in your blood.
Practically speaking, the number of positively charged molecules and negatively charged molecules in your blood should be equal. The net charge should balance out to 0.
Ernest P. Worrel - Electro Man (Image)
Otherwise you’d be walking around with an electric charge. It would really screw up most of the systems in your body.
Your body likes balance and homeostasis, so it keeps your cations and anions in equilibrium.
However, there’s a problem.
Our routine tests do not measure all of the ions in your blood. It’s unnecessary and/or unpractical to do so.
If you were to sum up the net electrical charge after running a CMP on your patient, it would seem like their blood has a positive charged. Obviously this isn't the case.
So our lab equipment must measure more cations than anions.
The anion gap is our correction factor. It's a calculation we use to account for the unmeasured anions in your blood.
Some of those unmeasured anions include sulfates, phosphates, and blood proteins like albumin. To be clear, we can measure many of these anions. We have tests to measure phosphate and albumin. But we don’t usually consider their electrical charge.
The anion gap is the difference between cations and anions that would bring the net electrical charge of your blood to 0.
Most likely, your practice institution will calculate it for you. But you won't be so lucky on a test in pharmacy school. Plus it's pretty easy to do yourself.
The calculation is as follows:
Anion Gap = Sodium – (Chloride + Bicarbonate)
Written another way, it would be:
AG = Na – (Cl + HCO3)
A normal anion gap is 12 mEq/L, but the range of 8 – 16 is acceptable. You can think of it as 12 mEq/L +/- 4. When things get outside of the 8 - 16 range, something is wrong.
And we use that information to diagnose acid-base disorders.
Diagnosing Acid Base Disorders
There is a phenomenal review that was published in 1991 in The Western Journal of Medicine by Richard Haber, MD (hey, acid-base disorders haven’t changed much in the last couple of decades). It's short, practical, and easy to understand.
A good part of my acid-base understanding comes from that article. As a result, a lot of what you're about to read stems from Dr. Haber.
It's not an exhaustive review, and there are other ways to diagnose. This is where you'll need to dig a little deeper if you work in critical care. But if you're in pharmacy school or do not spend all of your time in a MICU, the following should be more than enough.
Alrighty then, moving on.
There are 3 primary “steps” to diagnosing acid-base disorders.
Step 1: Look at the pH (to determine the primary abnormality)
Step 2: Calculate the anion gap (to determine if there is a primary metabolic acidosis)
Step 3: Calculate the excess anion gap and add it to the bicarbonate level (to further distinguish between metabolic acidosis versus alkalosis)
We’ll go through each step in turn. And explain the why behind all of it. First some additional framework…
When we talk about acid-base disorders, we are really speaking about 4 disorders.
Respiratory Acidosis (elevated pCO2)
Respiratory Alkalosis (decreased pCO2)
Metabolic Acidosis (decreased HCO3)
Metabolic Alkalosis (elevated HCO3)
Every acid-base disorder fits into one of (or is a mixture between) those 4 categories.
The categories themselves are self-explanatory. An acidic pH can be caused by either a metabolic or a respiratory acidosis. And a basic pH can be caused by a metabolic or respiratory alkalosis.
What changes is the cause of the acidosis or alkalosis. If it's a respiratory disorder, it's due to the CO2 level being out of range. Conceptually, this makes sense because we exhale from our lungs when we breathe.
And if it's a metabolic disorder, the bicarbonate (HCO3) level is off. Again, this makes sense because our kidneys and the enzyme carbonic anhydrase regulate HCO3 levels.
Additionally, there is the concept of Compensation. I mentioned before that the body “compensates” for acid base disorders.
For example, if there is a respiratory acidosis present, the body will compensate by raising HCO3. And if there is a metabolic acidosis, the body will compensate by decreasing CO2.
So if there is a respiratory disorder, the metabolic system compensates. And if there is a metabolic disorder, the respiratory system compensates.
Compensation is important when diagnosing acid-base disorders. It can tell you how long the disorder has existed.
For example, let’s take a patient with respiratory acidosis.
With respiratory acidosis, our pCO2 is too high. The metabolic system will attempt to counteract this by telling the kidneys to reabsorb (i.e. hold on to) HCO3. Basically (I just can't help myself with these puns), less bicarbonate will be excreted through the urine.
However, metabolic compensation takes about 3 – 5 days. It’s a slow system. So, if you see a patient with respiratory acidosis, and their bicarbonate is also elevated…
Then the patient has suffered from the respiratory acidosis for at least a few days.
On the other side of the coin, if you have a metabolic acidosis, your HCO3 is too low. The respiratory system will compensate by having you breath out more CO2. It accomplishes this by increasing your respiratory rate (i.e. hyperventilating).
Respiratory compensation happens within minutes to hours. So if you see a metabolic acidosis without respiratory compensation, then it is a very new disorder.
Got it? Good.
Let's move on to the 3 steps to diagnosing acid-base disorders.
Step 1
The first thing we look at is the blood pH. Whatever side of 7.4 it is on, the disorder that caused it to get there is the primary disorder.
For example, if the blood pH is 7.28, then either an increased CO2 (primary disorder = respiratory acidosis) or a low HCO3 (primary disorder = metabolic acidosis) caused it to get there.
The opposite, of course, is also true. If the pH is > 7.40, then either a low CO2 (respiratory alkalosis) or a high HCO3 (metabolic alkalosis) is the primary disorder.
The reason for this "rule" is that although the body does compensate for acid-base disorders, it never completely compensates. In other words, no matter how much CO2 you breathe out, you won’t be able to make your blood pH completely normal.
Step 2
The next thing we do is calculate the anion gap. Why? Because if the anion gap is extremely high, (> 20) then there is a primary metabolic acidosis (regardless of pH or HCO3 concentration).
The principle at work here is that the body does not create a large anion gap for no reason. If the anion gap is above 20, it’s due to some disorder.
There are a few common causes of an elevated anion gap (often called high anion gap metabolic acidosis). You’ll find that many of them are due to ingestion of a toxic substance. They are conveniently organized into the acronym MUDPILER:
M – Methanol
U – Uremia
D – Diabetic Ketoacidosis
P – Propylene glycol
I – Isoniazid
L – Lactic Acidosis
E – Ethylene glycol
R – Renal failure
Different incarnations of this acronym (and others) exist. There are some camps that say that GOLDMARK is the new MUDPILER. But in general, an elevated anion gap (> 20) means that you have a metabolic acidosis…and it is most likely caused by something in the MUDPILER acronym.
Call me old fashioned, but I prefer MUDPILER.
Step 3
The last step is to calculate the Excess Anion Gap. This is done by the following formula:
Total anion gap – 12
So it's your actual anion gap minus a normal anion gap (hence the "excess").
Then we take the Excess Anion Gap and add it to the bicarbonate (HCO3) level.
As a reminder, here's the formula for calculating the anion gap:
AG = Na – (Cl + HCO3)
And whatever number you get from that, subtract 12 to get the Excess Anion Gap.
Then take THAT number and add it to our measured HCO3 level.
What does this tell us?
First, refer to the normal values earlier in this post. A normal HCO3 level is typically 22 – 28 (again with some measurement variation in each institution).
If the Excess Anion Gap (EAG) + HCO3 is significantly higher than a normal HCO3 level (i.e. > 28), then there is a metabolic alkalosis.
If the EAG + HCO3 is significantly less than a normal HCO3 level (i.e. < 22), then there is an underlying non-anion gap metabolic acidosis.
You know it’s a non-anion gap acidosis, because we diagnosed any anion gap acidosis with Step 2.
Putting it all together….
The 3 Steps get us pretty far in terms of diagnosing an acid base disorder.
First we determine if the patient is acidic or basic.
Then we determine if it is an anion gap acidosis (and those are normally caused by the MUDPILER acronym).
Then we dig a little further and determine if we have a metabolic alkalosis or a non-anion gap acidosis.
It’s Practice Time
I know. I threw a lot of information at you and you may feel slightly overwhelmed. Well, the best way to review what we’ve learned is by applying all that knowledge to a case. And yes, I promise to explain every step of the way to avoid any confusion. So, without further ado, here’s your case.
P.S. I made this case very NAPLEX esque. Speaking of the NAPLEX, be sure to check out our NAPLEX resources here. Anyway, enough with the shameless plugs. Back to the case.
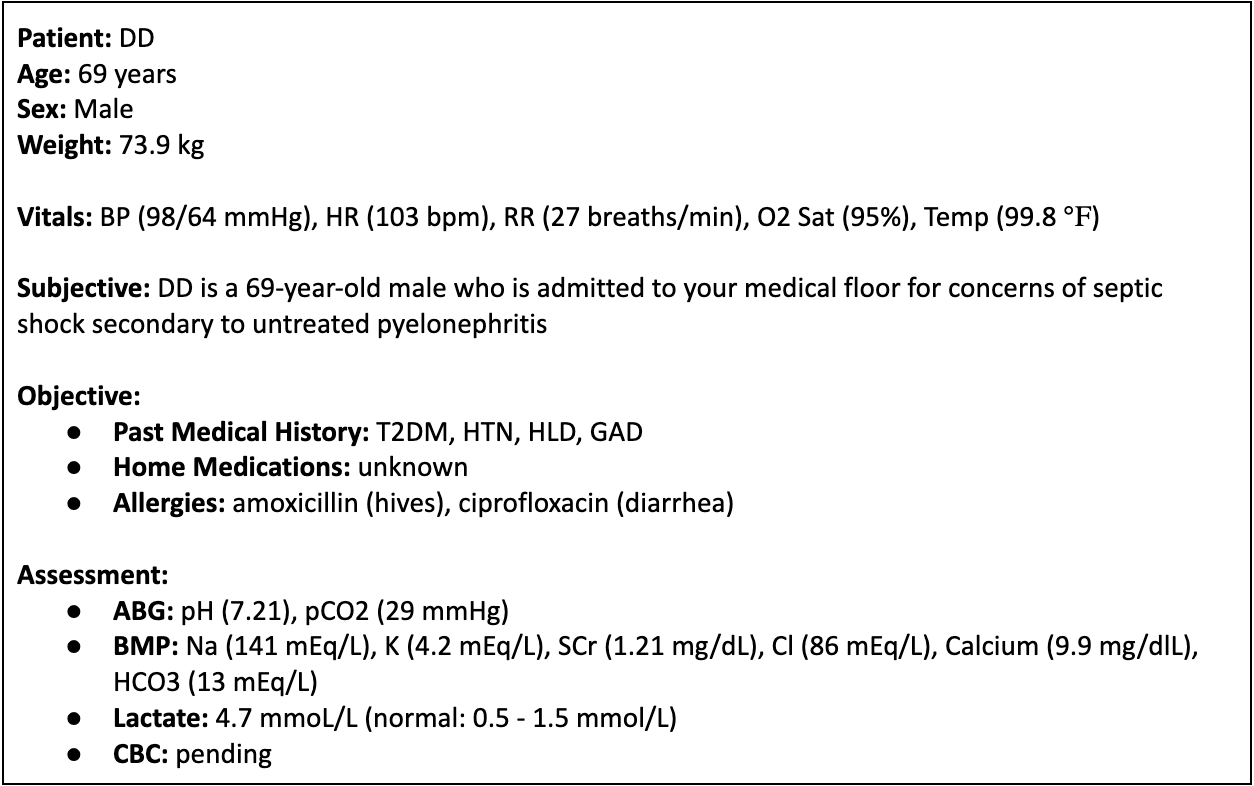
Which acid-base disorder best describes this patient’s laboratory findings?
A) Respiratory alkalosis with metabolic compensation
B) Respiratory acidosis with metabolic compensation
C) Metabolic alkalosis with metabolic compensation
D) Metabolic acidosis with respiratory compensation
E) Mixed respiratory and metabolic acidosis
I don’t want to leave you on a cliffhanger. The answer is D. Specifically, this patient has signs of anion-gap metabolic acidosis. Let’s walk through it using the steps we talked about above.
Step 1: Look at the pH. This patient has a pH of 7.21. We said normal blood pH is 7.35 to 7.45. Anything below 7.35 is acidosis and anything above 7.45 is considered alkalosis. Therefore, we can all agree that this patient has acidosis.
Step 2: Calculate the anion gap. AG = Na - (Cl + HCO3) —> AG = 141 - (86 + 13) —> AG = 45.
Okay we’ve made it pretty clear that this patient has anion gap acidosis. Now let’s determine if it’s respiratory or metabolic in nature. To do so, let’s take a look at our pCO2 and HCO3 levels. Remember, pCO2 is acidic and HCO3 is alkalotic. This patient has low HCO3 and low pCO2. Low HCO3 means acidosis but low pCO2 means alkalosis. So what’s going on here?
This patient is exhibiting metabolic acidosis given the pH and low HCO3 levels. The low pCO2 is a compensatory mechanism to combat the metabolic acidosis our patient is experiencing. His body is forcing him to hyperventilate to expel more CO2 and reduce the acidity. However, this patient appears to be in early stages of compensation as the pH is still very acidic.
Now let’s dig even deeper. What is the cause of this patient’s anion gap metabolic acidosis? Well, he’s in septic shock. Meaning that he is hypotensive leading to hypoperfusion of his tissues. This leads to increased anaerobic metabolism and lactate production. His lactate is elevated leading to lactic metabolic acidosis. Makes sense? Great!
Additional Info for Diagnosing Acid-Base Disorders
Again, there are ways that this gets more complicated.
The chloride ion (Cl) level has a role in diagnosing acid base disorders. There are mixed acid base disorders…where there are components of both acidosis and alkalosis.
You may also hear about Winter's Formula, which is used to assess respiratory compensation if a metabolic acidosis is present.
But for a general understanding, and for most practice settings, the 3 step process above from Dr. Haber is a good starting point.
I'll anxiously await the hate mail from the critical care practitioners...
Other good resources are the Life in the Fast Lane medical blog. They have a pretty handy diagnostic worksheet here.
There's also this review (warning: NEJM paywall ahead). It's more thorough than the Haber article, so it's a great place to go if you're seeking more information.
And finally, there's a bunch of other acronyms used to help diagnose acid-base disorders.
There's HARDUP for Non-Anion Gap Metabolic Acidosis.
There's CLEVER PD for Metabolic Alkalosis.
And there's also stuff like CANS and CHAMPS for respiratory acidosis and alkalosis respectively.
There's a lot of different systems and acronyms available, so find one that's easy for you to memorize or make up your own.
Treating Acid Base Disorders
In general, acid base disorders are treated by correcting the underlying problem. Not by administering acid or base to “reverse” the blood pH.
This is why diagnosis is so important.
If a patient has a metabolic acidosis and we give them sodium bicarbonate, their blood pH will indeed rise. But it will be short lived and it does nothing to correct the underlying problem. It’s symptom management.
Usually you'll see this in very sick patients as a sort of last-ditch effort to keep their heart and other organ systems working.
For everyone else, we give supportive care and try to figure out the root cause.
For example, if a patient has diabetic ketoacidosis (a type of metabolic acidosis), we’re better off lowering their blood sugar and keeping their heart rhythm stable instead of giving bicarbonate to correct the pH.
Correct the underlying problem, and the acid-base disorder will correct itself.