The Ins & Outs of ESBLs
A note from the tl;dr team: this article was reviewed and updated in February 2026 to ensure accuracy and relevance
Steph’s Note: Today, we’re going back to another favorite tl;dr topic arena - infectious diseases and antibiotics. If you’re like me, ID scared the bejesus out of me as a student. I knew my gram positive and gram negative bacteria, but for the life of me, I couldn’t keep straight what medications to use for what bugs in different locations. And to make it worse, you then add resistance issues…^head explodes^. Yeah, you’re not alone. So to help you guys along this journey, we have Kelsey Clark, a new tl;dr contributor and ID guru extraordinaire!
Dr. Clark is an Antimicrobial Stewardship Clinical Pharmacist from Shreveport, Louisiana. Her current stewardship interests are Merrem de-escalation and Teflaro use only when necessary. She has a passion for education at every level of the healthcare field (from pharmacy and med students to long term practicing physicians) and loves to take the complexities of antimicrobials and make them clear. (What did I tell you, she’s perfect for us!) Outside of the pharmacy, her interests include her massive collection of houseplants, game nights with friends, and giving her 4 dogs as many pets & snuggles as she can.
Remembering all of the bacteria and which antibiotics have the appropriate coverage is hard enough without the introduction of bacterial resistance. (If you need a refresher on the basics, be sure to grab your copy of our FREE tl;dr antibiotic cheat sheet here!) With this article, I hope to clear up some of the mystery around one of the more common resistant mechanisms we see in gram negative bacteria – the ESBLs.
Let’s do a few definitions and recall some basics first.
What is an ESBL?
ESBL stands for extended spectrum beta-lactamase. This is the enzyme that breaks down (hydrolyzes) the antibiotics structure, making them ineffective. It’s produced primarily by gram-negative bacteria.
Remember, an “–ase” ending tells you it’s likely an enzyme! Also recall that enzymes are proteins, which are created by the reading of an organism’s mRNA by ribosomes. This is important because the ability to produce this enzyme that makes bacteria resistant to certain drugs is actually coded into the bacteria’s genetic material.
Which Bacteria Can Develop ESBL Resistance?
Like we alluded to earlier, ESBL resistance is primarily produced by gram-negative bacteria. The most common offenders usually belong to the Enterobacteriaceae class. E. coli is often the top producer of ESBL, followed closely by Klebsiella spp. Other common producers include Proteus spp., Enterobacter spp., and Citrobacter spp.
Okay now let’s summarize everything in simple terminology to understand how these bacteria develop resistance.
Bacteria are smart. When they’re exposed to antibiotics for an extended period of time, they learn to fight back. One way to fight is by learning to produce certain enzymes (e.g. beta-lactamase) to develop resistance against certain antibiotic classes (e.g. beta-lactams). That way, the next time they go to war with the antibiotic, they release this new enzyme which breaks down the antibiotic’s structure making it ineffective. Pretty dang cool, right? Well, cool for science but bad for mankind.
What are Extended Spectrum Beta Lactams?
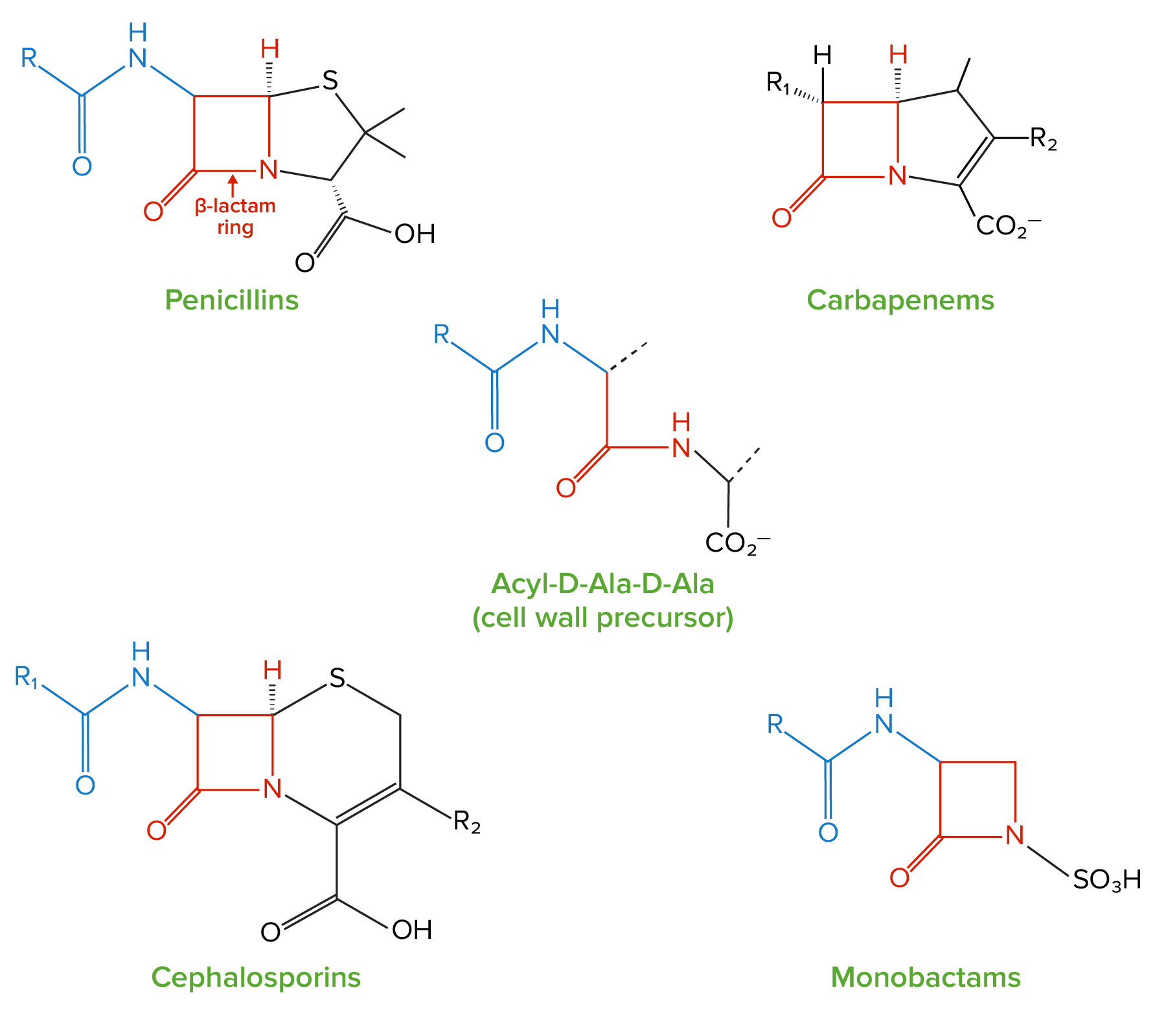
Check out the beta lactam rings (highlighted in red), and compare them to the cell wall precursor molecule in the center. It makes sense that these beta lactam antibiotics can fool the bacterial penicillin binding proteins (PBPs) into thinking that they are the desired cell wall precursor! Too bad (or actually oh-so-good for us humans…) that the beta lactams actually inhibit cell wall synthesis by playing Trojan horse with the PBPs. (Image)
Ok, no “-ase” on the end here. These are NOT the ESBL enzymes we just talked about. These are the third generation cephalosporins:
ceftriaxone (Rocephin),
cefotaxime (Claforan), and
ceftazidime (Fortaz/Tazicef).
What makes these medications extended spectrum? Is it that they cover more bacteria than the previous two generations of cephalosporins? Well…to be specific, these third generation cephalosporins are active against more gram negative bacteria than the first and second cephalosporin generations.
(Some of the first generation cephalosporins are actually better for certain gram positive infections than the 3rd generation! So it’s not that the third generation - aka the extended spectrum cephalosporins - is necessarily “better”, it’s just that they extended into more gram negative coverage than previously.)
Anyways, cephalosporin generation tangent aside…
It’s ok… You can’t always anticipate that a patient will grow an ESBL, but you CAN make sure they get the appropriate treatment ASAP once you know! (Image)
ESBL bacteria develop extrinsic resistance to more than just third-generation cephalosporins. Generally, they develop resistance to all penicillins, cephalosporins (1st gen through 5th gen), and monobactams (aztreonam). So if you’re treating an ESBL bacteria, rememebr that none of the antibiotic classes mentioned above will work.
It is well known that delay in appropriate antimicrobial treatment increases morbidity and mortality, so making sure your patient has the proper treatment for the ESBL is now your number one priority.
What is the proper treatment for ESBL-producing organisms?
Carbapenems are the empiric drugs of choice for ESBL infections:
meropenem (Merrem),
ertapenem (Invanz), or
imipenem/cilastatin (Primaxin).
With three medication options in this class, how do you approach selecting the best one? Let’s examine the differences…
All three carbapenems require adjustment for renal dysfunction. The least complicated adjustment is ertapenem (you just change the dose from 1000 mg to 500 mg when the CrCl is less than 30 mL/min - easy peasy! There’s not even a schedule change required when speaking in terms of adults.)
On the other hand, the most complicated renal adjustment is imipenem/cilastatin, which essentially requires a chart. Fun fun. For additional fun, imipenem/cilastatin is the hardest on the kidneys. So it typically isn’t used in practice unless it’s the drug of choice for a very specific infection (e.g., Nocardia pneumonia) since there are other (read: better/easier/safer) carbapenems.
NAPLEX question alert! Ertapenem (Invanz) is the only carbapenem which does NOT cover Pseudomonas spp. or Acinetobacter spp.! Imipenem/cilastatin and meropenem do have Pseudomonas coverage. For the record, Pseudomonas can produce ESBL – so don’t forget to cover the actual bug as well as the mechanism of resistance!
“If you don’t need Pseudomonas coverage, don’t use Pseudomonas coverage.”
Sometimes choosing the right antibiotic feels like searching for the Holy Grail… (Image)
In practice, this is typically hard to follow as some of the common antibiotics used for empiric coverage do have Pseudomonas coverage (e.g., piperacillin/tazobactam, cefepime). But this important thought about being intentional in your antibiotic choices applies to ESBLs as well.
Pseudomonas can produce ESBL, but don’t forget about the most prevalent players in the ESBL ring – E. coli, Klebsiella, and Proteus. The frequency with which you see each of these bugs as an ESBL differs depending on your specific location. Consult your hospital’s antibiogram, and remember, there IS a carbapenem that has a “narrower spectrum” than the others in that class. If you don’t absolutely need Pseudomonas coverage but still need a carbapenem for ESBL coverage, maybe give ertapenem a try!
How Do I Treat ESBLs in These Special Patient Populations?
The Patient Allergic to Beta Lactam Antibiotics
Cross-reactivity in patients with a true penicillin allergy (i.e., patients who have had a positive penicillin skin test) is 1% for carbapenems. That’s right, it’s RARE. So carbapenem use should not be withheld from penicillin allergic patients. For cephalosporins, there is less data available, but cross-reactivity does appear to remain low.
Anaphylaxis is a different story, and carbapenems should be given with caution to patients who have had an anaphylactic reaction to beta lactams. Consider giving a test dose of carbapenems to these patients, which means administering approximately 20% of the ordered dose, pausing the infusion, and monitoring the patient for 15 minutes for any reaction before proceeding with the remainder of the dose.
The Patient with a History of Seizures
While it’s true that the risk of seizures with carbapenems is higher than with other antibiotics, the risk is still very low. We’re talking less than 1% incidence total as listed for adverse effects. HOWEVER, the incidence of seizures with carbapenems is higher in patients who have a history of seizures than in patients who do not.
If your patient has a seizure history but is currently well controlled on their anti-epileptic medications, it is likely safe to give the carbapenem and monitor for any changes. If your patient was admitted with uncontrolled seizures and was also found to have an ESBL infection, it may be prudent to try a different antibiotic until the seizures are under control.
And with that segue…
What Non-Beta Lactam Antibiotics Cover ESBLs?
Let’s talk about aminoglycosides and fluoroquinolones.
The same genes that are responsible for ESBL production have been shown to contain other genes that code for resistance to aminoglycosides. Some studies have revealed quinolone resistance in bacterial strains that produce ESBL, though likely unrelated to the ESBL enzyme itself.
IDSA released guidelines in March 2022 on the Treatment of Antimicrobial Resistant Gram-Negative Infections, and these do a very good job of addressing issues with these infections in Q&A format.
SIDE NOTE: You should always use clinical practice guidelines with local resistance patterns when it comes to antimicrobials. Clinical guidelines should ALWAYS be used in combination with clinical judgement!
But do you really want to test those odds? (Image)
An example of what this looks like… A set of guidelines you pulled state that you should use levofloxacin for UTIs. You are aware most of the UTIs at your hospital are caused by E. coli, and your antibiogram shows 50% susceptibility of E. coli to levofloxacin in the last year. That means there’s a 1 in 2 chance your patient will not be appropriately treated. Probably don’t want to use levofloxacin here even though that’s the guideline preference.
Anyways, these new IDSA guidelines state levofloxacin and aminoglycosides may be safely used in patients with pyelonephritis or complicated UTIs caused by an ESBL. However, for infections outside of the urinary tract and for more invasive infections caused by ESBL-producing organisms, carbapenems are still recommended, although there’s a possibility to transition to fluoroquinolones (ciprofloxacin or levofloxacin), if the bug is identified as susceptible. The hope is to spare carbapenem use as much as possible!
And pretty much the same hold true for all non beta-lactam antibiotics that typically cover the ESBL producing bacteria. While resistance rates may be higher, these non beta-lactam antibiotics may still be utilized to treat the infection. Definitely not the best empiric coverage especially for a systemic infection, but may be an option pending susceptibilities.
For example, Bactrim generally has decent coverage against E. coli (~80% susceptibility based off my local antibiogram). If a culture ends up growing ESBL E. coli, Bactrim will probably have a lower chance of treating it. But, pending susceptibilities, transition from a carbapenem to Bactrim may be appropriate as long as the culture shows susceptibility. And the same goes for other non beta-lactam antibiotics such as Macrobid and Fosfomycin.
Long story short, beta lactamase only causes extrinsic resistance to beta-lactams. Non beta-lactam antibiotics may still have a chance to win the battle.
Piperacillin/tazobactam (Zosyn) has a beta-lactamase inhibitor! Can I use pip/tazo??
Piperacillin/tazobactam for treatment of ESBL-producing bacteria sparks a complicated discussion… Research hasn’t quite proven anything for this argument. The aforementioned IDSA guidelines addressed a few different scenarios that can play out with piperacillin/tazobactam, and these are driven by the site of infection:
If your patient was started empirically on pip/tazo for uncomplicated cystitis but the bacteria turns out to be an ESBL producer, let the patient’s clinical improvement be your guide. If they are improving, there is no need to change antibiotics. If they are not improving on pip/tazo, now we know why.
For pyelonephritis or complicated UTI caused by an ESBL, while treatment failure rates with pip/tazo may be low, it is still recommended to use a different agent, such as carbapenems or fluoroquinolones.
For infections outside the urinary tract, pip/tazo is not recommended – even if susceptibility is demonstrated.
Yeahhhh, let’s not help the enemy if we can help it, k? (Image)
For piperacillin/tazobactam, think about it this way. Even if the bug is susceptible now, it may not be susceptible a few days into treatment as the ESBL already has beta-lactamase enzymes. It would just need to make a few adjustments to make the enzymes needed to get rid of pip/tazo. And by using pip/tazo, you are literally giving the bug the blueprints.
What about Amoxicillin/Clavulanic Acid (Augmentin) and Ampicillin/Sulbactam (Unasyn)?
Just like tazobactam, clavulanic acid and sulbactam are also beta-lactamase inhibitors. Theoretically, they should inhibit the beta-lactamase enzyme that breaks down our antibiotics. That being said, theories don’t always translate to real life. The Infectious Diseases Society of American (IDSA) does NOT suggest use of Augmentin or Unasyn for ESBL E. coli cystitis, as robust data demonstrating clinical effectiveness are lacking. For blood stream infection and other serious infections outside the urinary tract, these agents are NOT recommended even when susceptibility is demonstrated.
So no, let’s not use Unasyn or Augmentin for the treatment of ESBL infections. Carbapenems remain the empiric treatment of choice.
How do I know if my patient has an ESBL?
If you’re very lucky, your clinical microbiology laboratory has resources to identify resistant bugs quickly. The lab can run genetic testing on the bacteria when blood cultures result as positive, identifying genes that give the bacteria the ability to produce the ESBL enzyme.
If you’re kind of lucky, your clinical microbiology laboratory can test for ESBL and will indicate on the culture and sensitivity report that the organism is a confirmed ESBL-producing bacteria.
However, for those of you who aren’t so lucky, routine testing for ESBL may not be done by your clinical microbiology laboratory. In this case, let ceftriaxone (Rocephin) be your guide. In terms of E. coli, Klebsiella pneumonia, Klebsiella oxytoca, and Proteus mirabilis, if the organism is non-susceptible to ceftriaxone (with an MIC > 2), you can use this as a proxy for ESBL identification.
DISCLAIMER: Using this method of identification can lead to false identification of ESBL if the organism is resistant to ceftriaxone for reasons other than ESBL!
If you have to use the Rocephin Proxy, consider risk factors for multi drug resistance to weigh the likelihood of a person having a true ESBL:
Patients with prolonged recent hospital stays and prolonged recent antibiotic use. These patients have had time to be introduced to bacteria that already know how to make ESBL, as well as giving the bacteria they have previously grown time to learn the antibiotics they are getting and become resistant.
Patients who may be immunosuppressed (e.g., patients undergoing chemotherapy or those with a history of transplant on daily immunosuppression)
Patients who have previously been identified as having an ESBL infection. If you grow it once, you can grow it again!
The tl;dr of ESBLs
ESBLs can be tricky, but they can be treated. The top 3 things to remember are:
Make sure the patient has appropriate treatment as soon as possible for their suspected site of infection.
Empirically reach for the carbapenems and de-escalate when (and if) possible.
Get as accurate of a patient history as you can – allergies, risk factors, prior microbiology results - to help you weigh ESBL likelihood and treatment options.
And there you have it! ESBLs in a nutshell. Hopefully this helps to make one of the murky resistance mechanisms more clear, and you now have the tools in your arsenal for identifying and managing an infection caused by these tricky bugs. Go forth, and be antimicrobial stewardship champions!