Diabetes Management Part 2: Building a Regimen
Steph’s Note: Well, we may have made y’all wait a couple extra days past our usual Monday post date on this one, but trust me when I say it’s worth the wait!! We have quite the writing crew on this one (because multiple brains are better than one, right???). You know them from their contributions to Part 1 of this series on diabetes management, but now you’re going to get to know them even better. I’m going to let the lineup introduce themselves.
Michelle Ton: I am a fourth year student pharmacist at the University of North Carolina Eshelman School of Pharmacy. I first stumbled upon tl;dr by a recommendation from my classmate when I was struggling to understand chemo-induced nausea and vomiting (CINV). I am honored to contribute to a resource that has helped me survive pharmacy school! After this year, I would like to pursue an acute care residency and specialize in...something. I am interested in ambulatory care, psychiatry, pediatrics, and more. Eventually, I want to go into academia. In my spare time, I like to find random art and music events, catch up with family and friends for hours on end, and watch Virginia Tech football - Go Hokies!
Sabrina Dunham: I am a graduate of UNC Eshelman School of Pharmacy and a current PGY1 Acute Care Pharmacy Resident at Moses Cone in Greensboro, NC. I will be starting a PGY2 specialty residency in cardiology this summer. My interests are in cardiology (no kidding), academia, and research. When I'm not nerding out, I like to spend time with my hubby and our 3 dogs, catch-up on good shows, catch-up with friends, and read things that have nothing to do with pharmacy.
Daniel Wadsworth: I am a third year pharmacy student at UNC. I love all things outpatient! I am currently on a summer-long ambulatory care internship at Moses H. Cone Memorial Hospital in Greensboro, NC. During the year, I work in the community setting as a intern with Harris Teeter Pharmacy in Chapel Hill, NC. <I assure you, Taylor and I are indeed separate people>. I first heard about tl;dr pharmacy through Michelle (she is just as enthusiastic about it irl), and I figure I should probably do what she's doing cuz she's pretty smart. In my free time I enjoy running, hiking, gardening, and making the most of my free university access to photoshop.
Taylor Sprague: I am also a third year pharmacy student at UNC. This summer I am an ambulatory care intern at the Moses Cone Internal Medicine Clinic. I am also a intern at Harris Teeter Pharmacy in Chapel Hill, NC (different pharmacy from Daniel’s). I am still determining what area of pharmacy is best for me, but right now ambulatory care is really piquing my interest. I enjoy hiking, running, a good book, and a Harry Potter movie marathon every once in a while.
Jennifer Kim: I am the Assistant Director of Pharmacy Education at the Greensboro Area Health Education Center in NC, Assistant Professor of Clinical Education at the UNC Eshelman School of Pharmacy, and a Clinical Pharmacist at Cone Health Internal Medicine Center. I enjoy doing anything with my family, swimming, skating, going to the park, movies, beach, or just staying home!
Whew, now that you know the whole first string, let’s get to learning!
What if Metformin isn't Meantforme?
Okay, some of you may have realized that diabetes can be a complicated disease state. To make it more complicated, the American Diabetes Association (ADA) released an update in 2019! Fear not, metformin is still the first line pharmacologic treatment for type 2 diabetes mellitus (T2DM).
Metformin for Halloween! Because everyone should have it, right? (Image)
But what if your patient is not at his/her goal? What if he/she cannot tolerate metformin (is metformin not “meant-for-them”)? What about other comorbidities? In this article, we will go through the guideline-directed recommendations about what the next steps are after metformin.
First, as a refresher on oral diabetic medications, check out this fantastic review post.
Second, if you need this info with you in your hip pocket, check out the Diabetes Cheat Sheet.
Ok, now that you’re up to speed on what medications are available, let’s chat about how to use them!
ADA 2019 Update
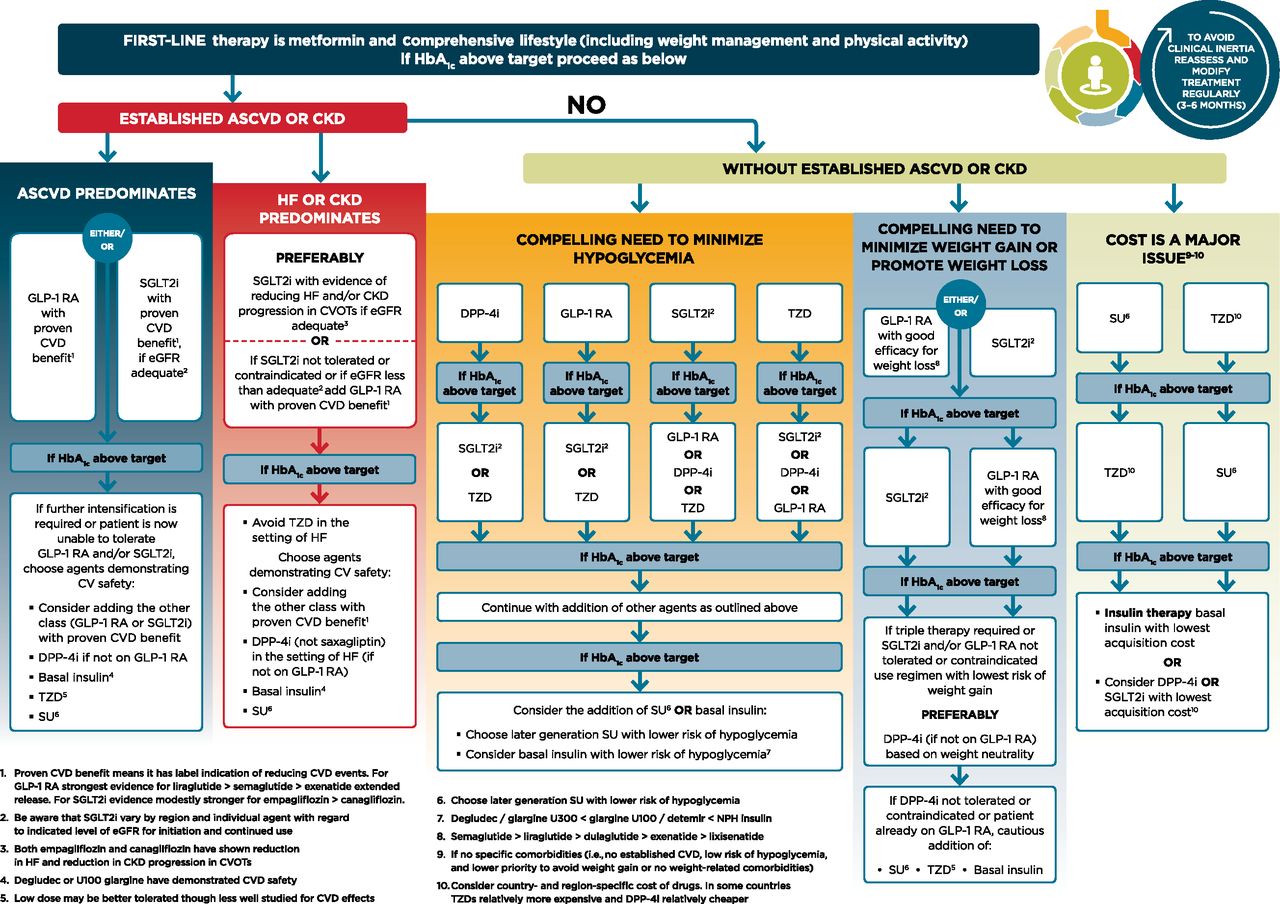
I’ve never met a healthcare professional who doesn’t love a good flow chart… so here you go, you’re welcome. (But beware, it’s a beast.)
From this point onwards, we’re going to take down this beast. We’ll break down each section of this diagram to give you a crash-course about how/why/when we got to these updates. Again, this flowchart is assuming your patient is on maxed dose metformin OR could not tolerate metformin.
Now, buckle up because here we go!
First and foremost, always think about the patient. What comorbidities do they have? How do they feel about needles? Is adherence an issue? Do they have insurance?
Major change: the ADA no longer recommends A1C to guide therapy selection. They recommend co-morbidities to be the guiding light when choosing which medication to add.
Patients with Atherosclerotic Cardiovascular Disease (ASCVD)
Both SGLT-2 inhibitors (empagliflozin and canagliflozin) and glucagon-like peptide-1 (GLP-1) agonists (liraglutide and semaglutide) have demonstrated in multiple randomized controlled trials their cardiovascular protective benefits.
SGLT-2 inhibitors were talked about in the previous post, but peep the table below for their proven cardiovascular benefits.
GLP-1 agonists are injectable non-insulin treatments and are pretty hype to be honest.
These drugs are analogs of human GLP-1, which increases glucose-dependent insulin secretion, decreases inappropriate glucagon secretion, and slows gastric emptying (this makes people feel fuller faster - spoiler alert! This leads to weight loss).
GLP-1 agonists have a lower risk of hypoglycemia compared to insulin.
There is a higher incidence of gastrointestinal side effects, but these usually pass. However, be aware of an increased risk of cholelithiasis (a fancy way to say gallstones) and pancreatitis (a fancy way to say pancreatitis).
Almost all of the GLP-1 agonists are long-acting:
Exenatide, dulaglutide, and semaglutide are dosed once weekly, and liraglutide is dosed once daily!
Up and coming: Do you have patients who don't like injections, but you still want them to try a GLP-1? Say goodbye to needles and hello to new ORAL semaglutide! This GLP-1 agonist is being studied for efficacy and is hopefully going to be brought to market soon. Check out the PIONEER-3 trial to learn about its comparison to a DPP-IV inhibitor for efficacy!
So how do you choose between SGLT-2 inhibitors and GLP-1 agonists? IDK…maybe ask the patient what his/her preference is for oral versus injection!
What major trials should you be aware of to impress your preceptor?
**It should be noted that in 2008, the FDA mandated safety trials in order to rule out CV risk (an initial concern found with rosiglitazone which was later uplifted). Some trials were designed to demonstrate noninferiority but subsequently estimated superiority. Inferring superiority in these cases is debatable since it may not have been pre-specified in the study methods.
For the post-hoc empagliflozin analysis regarding kidney disease progression, see here.
Patients with Chronic Kidney Disease (CKD)
Aw, aren’t your kidneys thoughtful? Return the favor! (Image)
Bam! SGLT-2s and GLP-1s strike again. From the trials mentioned above, these drugs have shown their ability to reduce the risk of CKD progression. The much anticipated 2019 CREDENCE trial helped reinforce canagliflozin’s safety profile in patients with CKD. It’s important to note that SGLT-2s have been shown in both the EMPA-REG and CREDENCE trials to have a greater initial reduction in estimated GFR (eGFR) during the first ~3 weeks than placebo, but the subsequent decline in eGFR was slower than placebo as the trials continued, showing renal protection benefits!
Important FYIs
For the most part, GLP-1 agonists don’t need renal dose adjustments in mild renal impairment (CrCl 50-80 mL/min/1.73m2). However, read the package insert to see which ones should be adjusted or avoided in moderate or severe renal disease/ESRD.
For SGLT-2s, look at the package inserts for specific eGFR cutoffs! These agents lose efficacy as eGFR declines, and there is an initial reduction in eGFR after starting therapy.
Now, let’s say your patient doesn’t have established ASCVD or CKD. This section has three main categories for deciding which way is best to go.
Compelling need to minimize hypoglycemia
Compelling need to minimize weight gain or promote weight loss
Cost is a major issue
Patients with a Compelling Need to Minimize Hypoglycemia
Are you significantly concerned about hypoglycemia for your patient? If so, there are four options to choose from to add to metformin:
(Image)
DPP-IV inhibitors
GLP-1 agonists
SGLT-2 inhibitors
Thiazolidinediones (TZDs)
These agents can minimize the risk for hypoglycemia. This is in contrast to sulfonylureas (SU), which increase the secretion of insulin without regard to a person’s blood glucose level. Basically, SU don't care if your blood glucose is high or not.
DPP-IV inhibitors and GLP-1 agonists are good in this case because their mechanisms are glucose-dependent. This means they are not going to increase insulin all willy-nilly without any glucose to act on.
The SGLT-2 inhibitors, when used as monotherapy, are associated with a lower risk of hypoglycemia. How, you ask?
They work in the kidneys to increase the excretion of glucose by blocking its reabsorption. Primarily, SGLT-2s decrease the renal glucose threshold to promote glucose excretion at lower plasma glucose concentrations (thus, not completely depleting the body of glucose). Since this group’s mechanism works only in the presence of elevated glucose in the blood and does not have control over the release of insulin in the pancreas, there’s less risk of hypoglycemia!
The TZDs do not come with an increased risk for hypoglycemia due to their mechanism of action. These agents help increase insulin sensitivity rather than having an effect on how much insulin is released. This results in less risk when they are used on their own.
Patients with a Compelling Need to Minimize Weight Gain (or Promote Weight Loss)
There are various options that can help patients lose weight. The first agent has already been mentioned multiple times in this article: GLP-1 agonists. These agents decrease gastric emptying and cause early satiety. Basically, your food is going to be around a little longer which is going to make you feel fuller sooner and longer. This helps patients to not eat as much. (There’s also a risk of diarrhea upon initiation, which certainly doesn’t promote weight gain - just not in as friendly of a way).
Now add this to some lifestyle modifications (always recommended!), and our patients should hopefully be making some progress in the weight loss division!
Remember to be careful in your GLP-1 agonist selection because not all agents will give the same level of weight loss, and we want to try and get the best bang for our buck when prescribing this agent.
Pro tip: Liraglutide and semaglutide produce the largest weight reductions (whether insurance covers these is another story…).
A second class used in this category are the SGLT-2 inhibitors. We all know the concept of water weight and that our body fluids can make that weight higher. SGLT-2 inhibitors are not considered diuretics, but they do have this type of effect. As glucose moves into the urine, more water follows it (a “-flozin” will get the urine flowin’). This will result in a diuretic effect, which results in weight loss in some diabetic patients.
You may be wondering… how large of a weight loss can you really expect for your patients? Is it going to be a significant amount? Will they even notice? Is it worth it?
YES!
If you don’t get the A1c control you need with just one of these agents alone, you can add on the other as well.
Now what if you have tried both agents and either the patient isn’t controlled or they can’t tolerate one of them? Well that’s it, no other options… NOT!
You can try adding a DPP-4 inhibitor! Here are some things to know:
A DPP-4 inhibitor should not be used concomitantly with a GLP-1 agonist. Think about it. You would be increasing GLP-1 in two different ways: via receptor agonism with the GLP-1 and by inhibiting endogenous GLP-1 breakdown through DPP-4 inhibition.
DPP-4 inhibitors are more weight-neutral and really have no bearing on weight loss. But hey, neutral is better than adding weight!
If this STILL is not helping to adequately reach A1c and glucose goals, there are more options!
You can consider the addition of a TZD, sulfonylurea, or basal insulin. These agents will not have the weight loss benefit we are ultimately looking for, but if the patient’s glucose isn’t controlled, we have to do something.
We will do a little pro and con chart in the next section, but just be careful with the addition of these agents and think about the patient’s comorbidities when considering which agent may be best to add or avoid.
Patients for Whom Cost is a Major Issue
In the world of medications, many of these agents are not cheap! It could be cheaper with insurance depending on the company, but the main idea is even if these agents may be doing well in lowering A1c and have other added benefits, we have to think about our patients. Try patient assistance programs, copay cards, or Medicare Extra Help if you want to maintain the clinical benefits of these high-dollar options. Some patients can get them for free!
Not everyone can afford these, but that doesn’t mean we are at a loss. There are still agents out there that we can use for our patients to help get their diabetes under control.
We can start off with a sulfonylurea or TZD in patients for whom cost is a major issue. These agents have some important pros and cons to think about with our different patients and their possible comorbidities. Who here doesn’t love a good ole pro/con list.. don’t see any raised hands, so here we go!
TA-DAHHHHH! You are now up-to-date about how to navigate the other drug therapies available after metformin. We wish you the best when engaging with your patients in meaningful conversations about their diabetes. Afterall, we’re all aiming towards the same goal: kickin’ diabetes to the curb!
(Image)