What Every Pharmacist Should Know about Grapefruit Juice
Happy Thanksgiving, everyone! When trying to figure out what to write for this week’s post, I wavered between a couple of topics, and I was rather struggling with what would light the writing fire. Then, when we had some friends over for pie and drinks, the topic dropped into my lap like a ton of bricks.
We were mixing up some Deep Eddy’s Ruby Red with lemonade for our guests (IYKYK), when one of our friends said, “Mmm, I’m on atorvastatin, and I’m supposed to avoid grapefruit juice. Will it be ok?” And of course, everyone stared at me, the pharmacist, for an answer.
Which got me to thinking… how much do we really understand this grapefruit-drug interaction deal? Sure, we all memorize which drugs carry the major warnings to avoid the combination, but as with anything in medicine, there’s always more to the story. So how much do you know about this, and is it truly an absolute contraindication?
This is what we’re here for today! Let’s learn together!
What is CYP3A4?
“CYP3A4” is a smushed moniker meaning cytochrome P 450 enzyme, family 3, subfamily A, and protein 4. The CYP3A superfamily of enzymes is largely comprised of CYP3A4. And when I say largely…I mean it takes the cake. On mass spectrometry, CYP3A4 is ~85% of the total CYP3A protein in the body with families 3A5, 3A7, and 3A43 accounting for only 3-5% each. Like all of the CYP450 enzymes, CYP3A4 is an oxidizer, and it is vital for metabolism of both endogenous and exogenous substances, including medications.
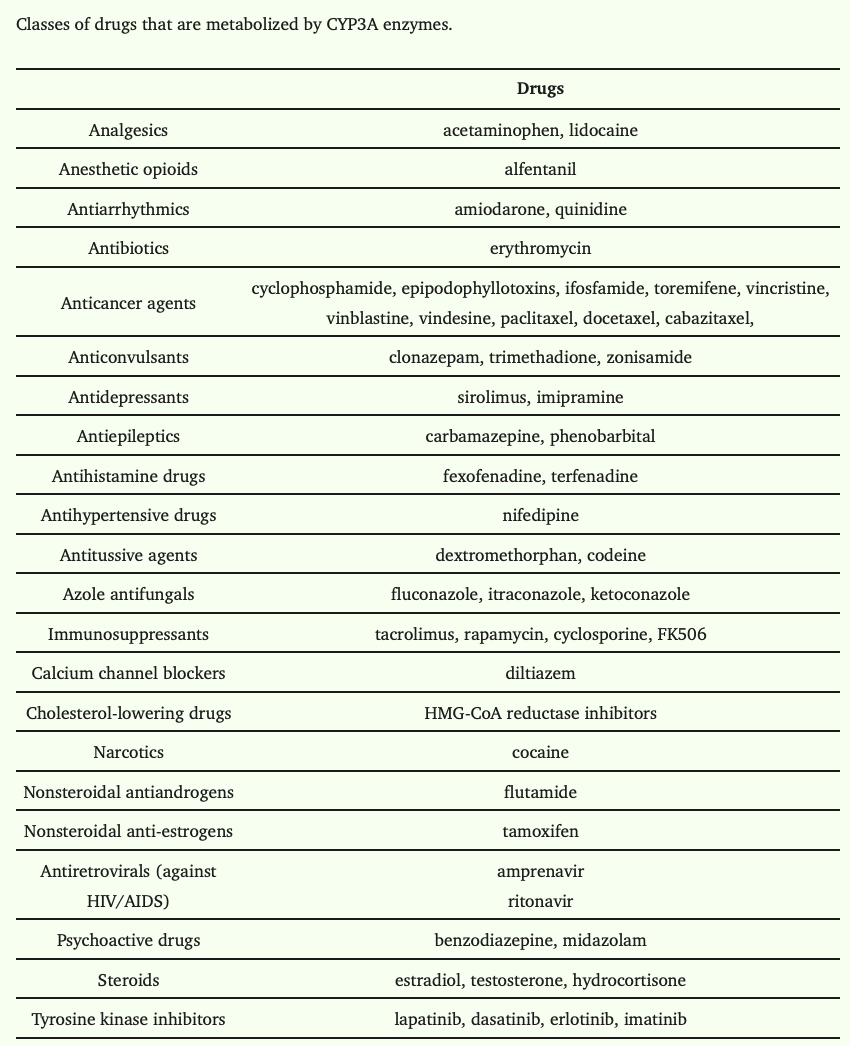
For the record, CYP3A enzymes aren’t exactly picky. Due to their substrate non-specificity, it’s estimated that up to 60% of pharmacotherapeutic agents on the market today undergo metabolism by CYP3A enzymes. And since CYP3A4 is the mega member of this family, that’s why we need to know more about this protein. It literally affects over half of the meds we manage. (Image)
CYP3A4 is found in the liver and intestines of humans. Although the liver is certainly a powerhouse of metabolism, let’s not downplay the role of intestinal metabolism. With a convenient location right at the site of medication absorption, intestinal CYP3A4 is heavily involved in the biotransformation and first pass metabolism of many, MANY agents. (Image) As such, it’s an important gatekeeper for bioavailability and therapeutic effect.
An example of first pass metabolism by both intestinal (1) and hepatic (2) CYP3A4 enzymes. Note how the actions of CYP3A4 in both locations occur before the medication is transported systemically for clinical effects.
Consider this… If CYP3A4 isn’t at the intestinal wall as usual - or isn’t functioning normally (ahem, ahem) - then medications that are usually metabolized at the intestinal wall won’t be. Which means more of the medication is absorbed into the bloodstream, leading to potentially increased effects - and adverse effects.
So why might intestinal CYP3A4 not be present or functioning appropriately… Good question and precisely why we’re here today!
What’s the big deal about grapefruit?
You might be wondering, “What’s the deal with grapefruit? Are all citrus fruits a problem, or just this one?”
Well, it really is mostly just grapefruit that’s the issue, although Seville (sour) oranges, pomelos, limes, and tangelos can also be implicated in this food-drug interaction. While the acidity from lemons and sweet oranges may wreak havoc on someone’s GERD, those fruits don’t have any foul play with CYP3A4. So what is it about grapefruit (and friends) that makes it a problem child, and how was this curiosity uncovered?
It was actually totally coincidental. (Image) In the late 1980s, there was a study conducted to evaluate the effects of ethanol on felodipine concentrations, and grapefruit was used to mask flavors. Incidentally, the investigators noticed that felodipine patients who were exposed to grapefruit had about 5 times higher felodipine levels. And voila! The interaction was discovered. Happy accident, right?
So now as far as grapefruit itself… This citrus fruit has been touted for its positive health effects, due to its antioxidants, vitamin C, fiber, and phytochemicals. Phytochemical is just a fancy word for a substance found in plants that’s supposed to have beneficial health effects in humans. (Think polyphenols from tea or anthocyanins from berries as common examples. Not necessarily useful for nutrition but thought to be helpful in preventing diseases.) Phytochemicals found in grapefruit include flavonoids and coumarins.
Don’t worry, you’re not alone. My brain went down that same rabbit hole when researching this coumarin-containing Jergens as a bug repellent for my toddlers. I also went there when I heard about coumarin-containing (illegal in the US) tonka beans for the first time on The Great British Baking Show.
Yes, you read that right. “Coumarins.” Your brain may have just gone down a pharmacy rabbit hole, where you’re now trying to figure out if grapefruit contains natural anticoagulants. BUT this is not the case. While Coumadin (aka warfarin) is a potent anticoagulant and coumarin derivative, coumarins themselves have no blood thinning properties and are actually often used for their vanilla-like fragrance in the cosmetic and food industries. (Image)
Now that we’ve dug ourselves out of that rabbit hole, check out the info below noting the theorized health benefits of grapefruit’s phytochemicals:
Flavonoid: naringin
In addition to giving grapefruit its bitter taste, this component is thought to be antioxidant, anti-inflammatory, anti-apoptotic, anti-ulcer, anti-osteoporotic, and anti-carcinogenic. A bit of everything, eh?
Furanocoumarins: bergamottin and 6,7-dihydroxybergamottin (DHB)
In addition to helping grapefruit plants ward off pests and diseases, these phytochemicals are thought to have antioxidant, anti-inflammatory, and anti-cancer properties. More wonder substances!
These 3 phytochemicals - naringin, bergamottin, and DHB - are found in varying levels in all 3 grapefruit varieties (white, pink, and ruby red). In general, white grapefruit has more of all 3 phytochemicals than pink or red. The seeds and pulp of the red grapefruit have the least of them. However, other factors such as where the fruit are grown, fruit maturity, storage, and processing have all been associated with variations in phytochemical levels, so it’s hard to even make generalizations about phytochemical distribution.
All this to say that not all grapefruits are created equally when it comes to these substances…and not even all parts of the grapefruit are consistent. Eating grapefruit flesh delivers different quantities of these substances than drinking commercial grapefruit juice (or even home squeezed grapefruit juice). Why do we care? Well, these 3 phytochemicals are suspected to be the main culprits responsible for interactions between grapefruit and medications. Let’s talk about how.
Naringin weakly inhibits intestinal CYP3A4. So while it’s a player in the game, it’s second string. The furanocoumarins are the stars of the drug interaction show. They inhibit intestinal CYP3A4 in 3 ways:
Competitive inhibition (most common)
Reversible
Occurs after the first dose of grapefruit
Permanent inactivation
Irreversible
Must regenerate new CYP3A4 to restore activity
Occurs within 30 minutes after grapefruit ingestion and lasts 2-3 days after last grapefruit
Complete loss of enzyme
Of note, the grapefruit furanocoumarins do not inhibit CYP3A4 in the liver - only the intestine. Studies have also demonstrated no impact from grapefruit’s CYP3A4 inhibition when medications are administered intravenously, further supporting that this interaction occurs at the intestinal wall.
So then the next question is this: what factors affect the degree of grapefruit’s CYP3A4 inhibition?
Grapefruit Quantity
Simply put, the amount of grapefruit and/or juice consumed matters. The more grapefruit products ingested, the more impact on intestinal CYP3A4. (Image) Along the same lines, frequency of ingestion also influences the impact on medication levels. Elevations in felodipine went from 3 times higher to 5 times higher when consumption increased from 250mL (about one grapefruit) once to 250mL of juice 3 times daily for 6 days.
Check out this sampling of severe adverse effects from grapefruit-medication interactions, and pay special attention to the quantities of grapefruit consumed prior to the events. Note that a whole fruit is considered to be about equal to 200-250mL of juice for reference.
Timing of Grapefruit Ingestion
Again, simply put, how much time passes between grapefruit and medication ingestion matters. The more time between grapefruit products and medication, the less effect there is from intestinal CYP3A4 inhibition.
For reference to give some idea, in that same felodipine - grapefruit juice study, the greatest interaction (aka the most inhibition) occurred when there were 4 hours between ingestion of the 2 substances. That interaction dropped by 50% with a 10 hour gap and to 25% with a 24 hour interval. So the time gap matters.
Medication and Dose
Obviously, some medications depend on CYP3A4 metabolism more than others. I could never make a 100% inclusive list of medications that rely on CYP3A4, (ain’t nobody got time for that), that’s what LexiComp is for. But here’s a decent overview of classes with sample drugs to refresh your memory (Image):
I know, you were expecting an Avril “Complicated” meme here. But this was just funnier. Sad because it hits close to home…but funnier.
FYI, don’t forget to consider the compounding effect of a person taking multiple medications that influence CYP3A4 activity! While grapefruit inhibits intestinal CYP3A4 enzymes, other medications could do this as well AND may inhibit liver CYP3A4 too. So be sure to account for drug interactions on top of food interactions.
We told you being a pharmacist is complicated, didn’t we? Have we said that? If we haven’t in all these years…being a pharmacist is complicated. There you have it. (Image)
Oral Bioavailability
Medications with innately low oral bioavailability stand the highest chance of causing issues in the presence of grapefruit. Again consider felodipine.
This drug normally has an oral bioavailability of about 15% after being metabolized by CYP3A4 in the intestine and then the liver (before even reaching systemic circulation!). However, this bioavailability significantly increases in the presence of grapefruit’s enzymatic inhibition, which is why the potential clinical effect is markedly increased.
If a drug isn’t so reliant on CYP3A4 in the first place, the presence of grapefruit won’t really be that big of a deal. That’s why medications with low oral bioavailability carry the potential for higher risk in the presence of grapefruit.
Individual Patient
Somewhat unfortunately for us pharmacists, there’s not exactly an easily available assay for our patients to use to evaluate variations in intestinal CYP3A4 expression and distribution… But we do know there are differences between patients. Not only are there allelic variants which affect individual enzyme function, but there are also differences in protein expression throughout the enteric tissue. In studies, the largest increases in drug concentrations under the influence of grapefruit juice were in patients who had the highest amounts of CYP3A4 in their intestines.
Makes sense, right? More enzymes to inhibit, bigger effects on dependent drugs. But how does a person with normal CYP3A4 in their gut compare with a person who has low amounts of high metabolizer CYP3A4? Or high amounts of slow metabolizer CYP3A4?
So while a patient could theoretically undergo pharmacogenomic testing to determine if they have a wild-type CYP3A4, there’s no way as yet to figure out if the expression through the intestinal tissue is normal, high, or low, or even distributed geographically in a common pattern. (Try convincing a doctor or your patient they need to have an intestinal biopsy to take that statin. Yeah, not happening…)
Also, don’t forget that each medication is absorbed (and metabolized) across different sections of the GI tract, so enzyme LOCATION in addition to function and amount could also compound the variability of this medication-food interaction!
You can see how trying to predict which patients are more susceptible to the impact of grapefruit juice’s inhibitory properties at baseline is kind of a…crapshoot. Potentially you could theorize that patients who require higher doses of a CYP3A4 medication for desired clinical effect may have higher amounts of intestinal enzyme, but that’s even a stretch.
In terms of patient characteristics, we should also suspect older adults (especially those over 70) of being at higher risk for grapefruit-drug interactions. First, they’re the ones who eat the most grapefruit. It’s not just a stereotype! Consumer data shows that people 45 years and older buy the most grapefruit. (Although you could argue that this flavor is making a comeback in seltzers, sodas, and alcoholic beverages that younger generations also like, it’s pretty rare to run into young folk straight up eating grapefruit everyday).
Second, older adults take the highest number of medications, thereby creating the most potential to have some sort of interacting drug. Third, they are likely more susceptible to the adverse clinical consequences of the interaction due to lack of physical compensation or tolerance. For example, those baroreceptors just don’t signal hypotension quite so quickly at 75 years old as they do at 25, so get ready for the orthostatic fallout.
As pharmacists, it’s important to consider our patients as individuals and assess their risk outside of general statements. This is just one more example of that.
The tl;dr of Grapefruit Interactions with Medications
Grapefruit contains flavonoid and furanocoumarin phytochemicals that inhibit the activity of intestinal CYP3A4. There can be significant variability in the degree of this inhibition depending on grapefruit type, source, processing and product, storage, as well as individual patient factors.
While this makes it tricky (to say the least) to determine what scenarios might produce clinically significant drug elevations and adverse effects, the factors we can account for include asking patients about how much grapefruit they’re ingesting, when do they consume it in relation to their susceptible medications, and are they experiencing any possible adverse effects. We can review medication lists to assess for potential additive inhibition or clinical effects, and we can inquire about their medical history to see if they’re at elevated risk from consequences of the interaction. From there, it’s clinical judgment.
As for my scenario that started this whole shebang, it turned out our friend forgot to take his dose of atorvastatin the day before. The time gap was over 24 hours from his last dose, and he had at least 10 hours until resuming his statin. He was on the lowest dose of atorvastatin with no other medical history or medications. And the drink, while advertised as being “infused” with real grapefruit juice, was mixed conservatively with a much larger quantity of lemonade (we were certainly nowhere near the 200-250mL of a whole grapefruit referenced in the above studies!). So grapefruit quantity was very restricted. All in all, in this particular scenario, I told him he should enjoy his beverage and have some pie! But this is definitely to be taken on a case by case basis.
Let’s contrast this with the example of my then 69 year old dad, who at one point was taking nilotinib, atorvastatin, amlodipine, and apixaban (to name just a few of his meds). Did I advise that he avoid any grapefruit juice at all? YES.
Consider your own clinical judgment. What would you have done?