Polypharmacy: Putting the HARM in Pharmacy
Steph’s Note: Jessica Boh, PharmD, MPH, BCPS, BCACP is a Clinical Pharmacy Specialist practicing within the Washington, DC Department of Veterans Affairs system. She graduated from the University of Florida College of Pharmacy (obligatory GO GATORS!), completed a PGY1 residency at the Memphis VA, and a PGY2 in Ambulatory Care at the North Chicago VA. She earned her Master of Public Health at Florida International University with the goal of utilizing population management to improve patient outcomes. During her PGY2, Jessica led facility-wide implementation of a nationally-developed deprescribing tool to reduce polypharmacy. Jessica loves to teach, cook (hello fellow foodies!), read (science fiction and psychology-related nonfiction), advocate for the pharmacy profession, and write for fun (duh). Check out this PCSK9-inhibitor article she previously wrote for tl;dr!
Have you ever seen a patient’s medication list that gave you immediate anxiety? The total number of medications is 20 or even 30-something? Six different medications for blood pressure, and none are at an optimal dose? Multiple medications with 3 or 4-times daily administration instructions? Amphetamine in the morning and zolpidem at night? A bunch of dietary supplements and herbals to boot? What does this poor patient even have time for in the day, besides taking medications?!
In this article we’re talking about the poly-harms of polypharmacy. As the Baby Boomer (born 1946-1964) generation ages, we are seeing increasing numbers of older adults with chronic diseases. Furthermore, as medicine continues to evolve within a culture that values quick-fix solutions, we not only have an app for everything but also a pill for everything.
In 2020 alone, 53 new drugs were FDA approved. But does more or newer medicine also mean better outcomes? Let’s peel apart the poly-layered pill problem (say that 5 times fast).
The Polypharmacy Problem: How Bad Is It?
One 2016 study on Medicare beneficiaries found that patients were prescribed an average of 14 medications upon discharge from acute hospitalization to a skilled nursing facility. In addition, 43% of the medications prescribed at discharge were medications associated with geriatric syndromes (MAGS), such as cognitive impairment, delirium, falls, unintentional weight loss, urinary incontinence, and depression.
When an elderly patient presents with a possible medication-related symptom, it can be especially difficult to pinpoint the problem as a medication’s fault. Is the patient’s constipation caused by his verapamil or because he’s 82 years old, doesn’t drink much water, and takes OTC calcium supplements? Is the patient’s forgetfulness a normal aging process or a result of his long-term use of benzodiazepines?
Not-so-fun fact, long-term use of benzodiazepines is associated with cognitive impairment. Other medication side effects that can be confused with signs of normal aging include dizziness, falls, weakness, tremor, and skin rashes.
Besides, who are we to say they don’t need all those medications? After all, we humans tend to have more health problems as we age, right?
The time to intervene in polypharmacy is right MEOW! Super Troopers, anyone?
FREEZE! Enter stage left: THE POLYPHARMACY POLICE.
Pharmacists are perfectly positioned in the healthcare system and expertly trained in medication management. If we don’t blow the whistle, who will? If you’re not comfortable waving your name badge in authority on medication expertise, at the very least we pharmacists can be the ones to start conversations with prescribers about medication safety and polypharmacy.
Mo’ Meds, Mo’ Problems
Studies have shown that the higher the number of medications a patient is taking, the higher the risk of drug interactions and adverse effects. One such study showed that, of older adults in the community taking at least 5 medications, 50% had possible drug-drug interactions. In the same study, the percentage of drug interactions increased dramatically to 81% for patients taking 10-14 medications, 92% with 15-19 medications, and 100% for patients taking 20 or more medications.
Although that study included less than 300 patients, another study examining adverse drug event (ADE)-related outpatient and emergency room visits across 11 years also showed that the risk of adverse drug events increased with age and number of medications. In that study, 88% of adults 65 years and older had an increased risk of adverse drug reactions.
If that’s not enough evidence yet for you, a nursing home study showed that residents with 9 or more medications had double the risk of experiencing an adverse drug reaction. Polypharmacy and potentially inappropriate medications (PIMs) significantly increase risk of hospitalization, outpatient visit days, and medical costs.
The Poly Definitions of Polypharmacy
There is no single widely accepted definition. Polypharmacy can refer to the number of medications, the nature of the medications, and/or the appropriateness of therapy.
Polypharmacy has been defined in the literature as:
A large number of medications (most commonly considered to be more than 5, but as high of a threshold as 11 medications)
“Too many” medications (think: patient noncompliance, inappropriate for goals of care)
Potentially Inappropriate Medications (PIMs) per the American Geriatric Society Beers Criteria (FYI, the Beers Criteria list was updated in 2019…might be a good time to review!).
What do you see? Niagara Falls or sildenafil for SSRI-related sexual dysfunction? (Image)
Perhaps you have also heard the term “prescribing cascade,” which immediately conjures (at least in my brain) the image of a waterfall made entirely of pills. The prescribing cascade describes the process when a medication causes a side effect and so another medication is prescribed to treat the side effect of the first medication (and potentially so on and so on and...)
Other examples of inappropriate prescribing can include:
Duplicate therapy (using 2 medications when 1 would do the trick)
Example: ranitidine and omeprazole, when adequate relief of symptoms is obtained with one or the other
Medications that the patient is unwilling, unlikely, or unable to adhere to
Example: insulin aspart TID for a patient with trypanophobia (fancy word for scared of needles)
Unnecessary medications (no longer indicated or never was indicated)
Example: pantoprazole continued twice daily on discharge from the hospital despite no history of GERD or any other indication for a PPI
Medications with a dose or frequency not appropriate based on patient-specific conditions
Example: ignoring the apixaban age and renal function dose adjustment for atrial fibrillation
One thing that is NOT technically polypharmacy (but sometimes mistakenly described as such) is when patients pick up medications at multiple pharmacies, often due to price shopping (poly = many, pharmacy = an actual pharmacy building). This can certainly lead to medication errors since each pharmacist may only have a partial medication list for the patient, and it is an unfortunate way to miss drug interactions and duplicate therapies. However, that specific concern, along with doctor shopping, is a separate issue outside the scope of this polypharmacy discussion.
The Deal with Deprescribing
Most people think of deprescribing as discontinuing a medication for any of the above polypharmacy-related reasons. It can also describe dose or frequency reduction, switching to an alternative medication with a more favorable side effect profile, or switching to a medication the patient is more likely to adhere to.
Deprescribing has been shown to improve quality of life among older adults by decreasing pill burden, reducing side effects, and improving adherence to medications treating chronic illnesses.
Wait...then isn’t deprescribing the same thing as medication reconciliation?
Pharmacists across many healthcare settings already do a great job of deprescribing when identifying unnecessary or inappropriate medications during a medication reconciliation. Medication reconciliation can be a tool to aid in deprescribing, but it is not the same thing as deprescribing. Med rec is an evaluation (often with recommendations) while deprescribing is the act of making an intervention to address polypharmacy.
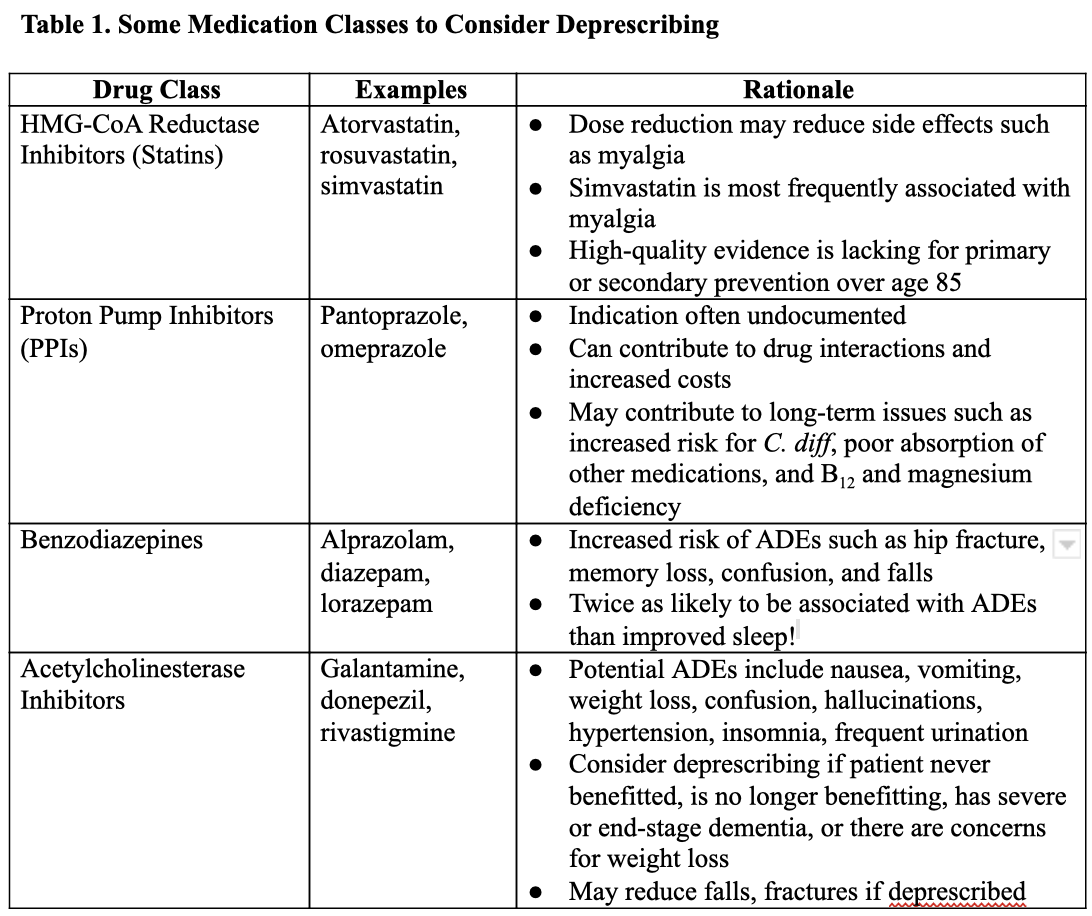
The following drug classes in Table 1 are just the tip of the iceberg for potential deprescribing opportunities! Some other medications to consider deprescribing not listed below include aspirin for primary prevention, antipsychotics, digoxin, and nitrates. See the Resources for Polypharmacy and Deprescribing section below to explore more!
Want to see more data? Check out the following links for the HMG-CoA reductase inhibitors (statins), proton pump inhibitors, benzodiazepines, and acetylcholinesterase inhibitors.
Deprescribing: A Tough Pill to Swallow?
So, what’s keeping us from cleaning up those medication profiles left and right? Many barriers to deprescribing at all levels of care have been identified:
Patient/Caregiver: Patients or family can be reluctant to discontinue medications that a patient has been on for a long time for a variety of reasons including fear of an adverse event, fear of change in health status, and difficulty accepting changes in goals of care.
For example, often the family of a patient will choose to continue galantamine even after a patient reaches end-stage dementia for fear of worsening cognitive decline once stopped.
Prescriber: Physicians and other prescribers may also share fears of an adverse event upon discontinuation of a medication.
For example, discontinuing simvastatin in a 90-year old patient with no history of cardiovascular disease for fear of causing a first heart attack or stroke.
Lack of well-established guidelines: The less-than-defined guidance for deprescribing and/or a lack of knowledge of current deprescribing evidence can contribute to fears of adverse events.
Clinical inertia and multiple providers: The “if it ain’t broke, don’t fix it” mentality may play a role in patients continuing medications that may or may not cause issues in the future (if they aren't already). Additionally, when there are multiple providers managing one patient, one or more of them may be reluctant to deprescribe.
For example, the primary care physician may not want to adjust or discontinue a medication initiated by a specialist.
Pharmacists can help patients and prescribers to overcome these barriers. Deprescribing can be approached with patients and family members as an ongoing discussion of risks and benefits with each medication. Pharmacists can encourage prescribers to continually assess goals of care with patients and family, and they can discuss how medications may or may not fit with their established goals of care.
For example, if a patient/family decides that comfort is a goal of care, pharmacists can reduce pill burden and recommend medications that may be discontinued, reduced, or switched to medications with a lower risk of side effects. Pharmacists can also share evidence and resources with prescribers to increase their comfort level with deprescribing.
Resources for Polypharmacy and Deprescribing
Deprescribing.org contains evidence-based Canadian guidelines for deprescribing a variety of medications, including deprescribing algorithm charts that make it even easier to decide.
STOPP/START stands for Screening Tool of Older Persons’ Prescriptions and Screening Tool to Alert to Right Treatment. These are criteria that help guide medication-related interventions in older patients with multiple comorbid conditions.
LESS/CHRON stands for List of Evidence-Based Deprescribing for Chronic Patients criteria. This tool can be implemented into the electronic health system and has 27 criteria to guide deprescribing.
VIONE is an acronym-based tool initiated within the Department of Veterans Affairs health-systems to guide deprescribing. All medications on a patient’s profile can be classified as V (vital, life-sustaining), I (important for quality of life), O (optional), N (not indicated or may do more harm than good), or E (no documented indication—E stands for Every medication has a documented indication). Medications in V and I should be continued while medications classified as O, N, or E may be recommended to discontinue.
ChoosingWisely.org promotes conversations between clinicians and patients in choosing care (including medications) that is supported by evidence, not duplicative, free from harm, and truly necessary. This website also features patient-directed educational materials.
The TL;DR of Polypharmacy
Polypharmacy is a widespread problem with widespread consequences on risk of ADEs and quality of life in the elderly. Information is growing on the safety and impact of deprescribing certain medication classes, but more evidence and guidance should be published to increase provider and patient comfort levels with deprescribing. Deprescribing should be an ongoing provider-patient discussion weighing risks and benefits of medications along with patient preferences and goals of care.
Pharmacists are uniquely positioned to aid in these conversations between providers and patients by providing expert advice on medications and medication safety. Availability and utilization of deprescribing tools may serve as an impetus to changing the culture of prescribing and medication management.