What Every Pharmacist Should Know about Breastmilk
Steph’s Note: This week, we’re taking a dive into what I think is one of the most fascinating functions of the female human body - milk production. Although the topic of medications and lactation doesn’t arise every day on the job, when it does, wouldn’t it be lovely to have a grasp on what’s happening in this process? Sure, you can read the “Breastfeeding Considerations” section of Lexi, but if you’re like me, you want to understand a bit more behind the scenes!
Disclaimer: this is NOT a post listing what medications are or are not safe for lactation. That’s what drug references are for. This is for understanding the physiologic processes that shape how medications enter and exit milk. Now that we have that out of the way, let’s learn.
Badass Breastmilk
Breastfeeding - an upper body workout akin to wrestling or MMA.
Mother’s milk. Call me biased (given I’m currently nursing my third nugget), but the human body is just so freaking cool. Not only does mom’s milk turn skinny premature legs into adorable chunky trees, but it literally transforms to be exactly what baby needs at each stage of life. On top of this, it transforms across the course of a day. And it’s not just food… It’s protection, both now and in the future. It’s developmental aids. It’s communication and bonding between mom and baby. It’s literal magic, like a mom’s hidden superpower.
Some evidence-based benefits of breastfeeding include decreased risks of:
Infections (especially GI and ear infections)
Lymphoblastic and myeloid leukemias
Types 1 and 2 diabetes
Asthma
Sudden Infant Death Syndrome (SIDS)
(Not necessarily due to the milk itself, but breastfeeding is also thought to promote better speech development because of all the facial muscles needed for nursing. And it has multiple health benefits for mom too! Win win!)
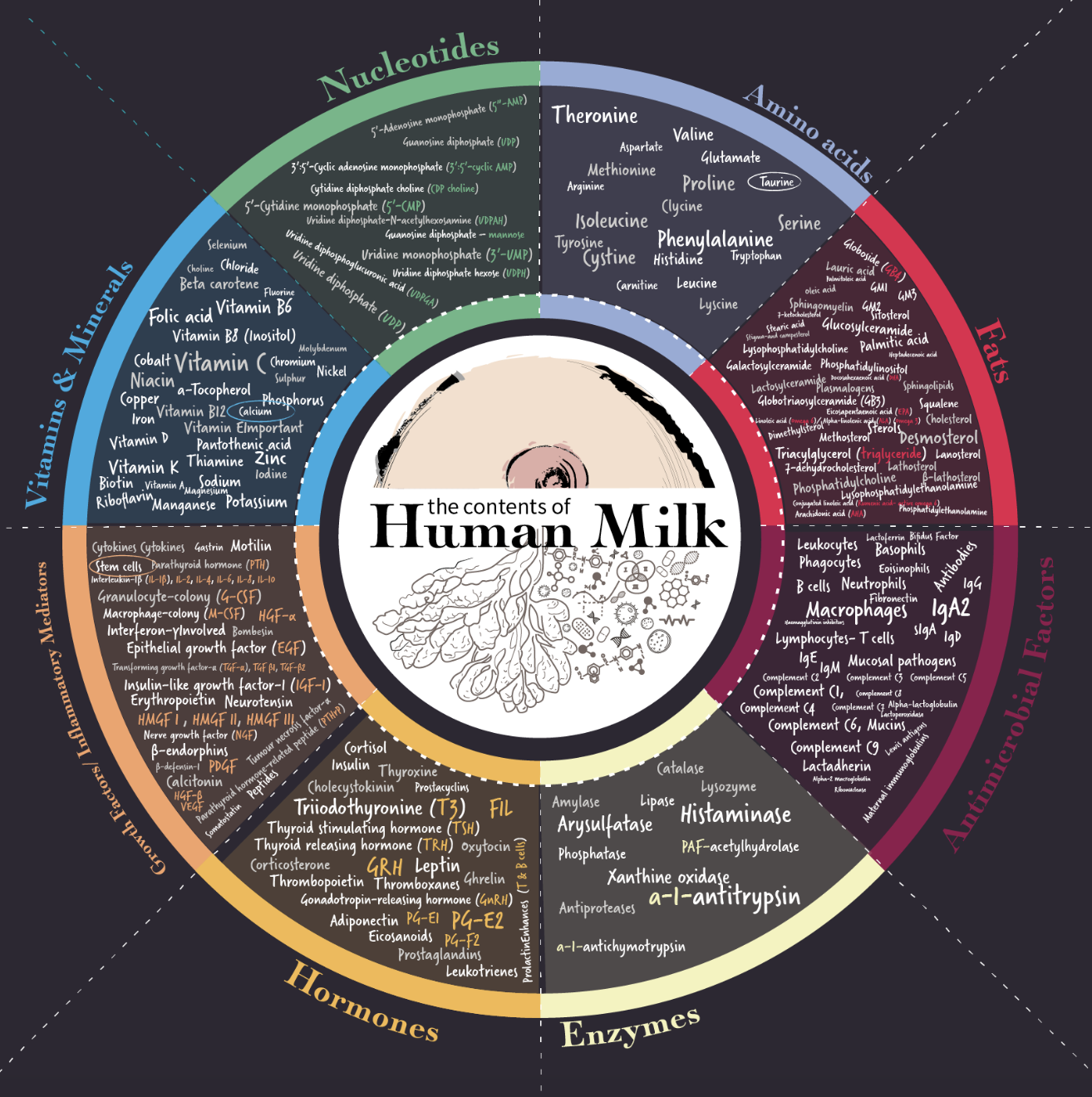
So what’s in this magic drink?
This pretty famous infographic from the Human Milk Foundation illustrates just how wonderfully comprehensive and complex this ambrosia is:
I guarantee this mom knows how uncomfortable breastfeeding can be…that little one’s grip lol
When I say it has everything…I mean it has everything. Which is why the World Health Organization recommends exclusive breastfeeding for the first 6 months of life and complementary breastfeeding (along with solids and other foods) through at least 2 years.
Time for a summary reality check. Breastmilk is 100% magic. But just FYI, breastfeeding is also hard. Sure, it’s been done for how many tens of thousands of years, so you would think it’s this primitive, easy thing to accomplish. (I know that’s what I thought before I had my first.) But it’s actually really really hard, which truly surprised me.
But then they look up at you like this, and who cares about the discomfort??
It’s hard to find the right position, get the right latch, find time to pump to get the supply going (and keep it going as needed), get up every 1-2 hours at night for months on end, not end up with milk everywhere…and I could go on. And yes, for the record, it hurts (no matter what every lactation consultant tells you in the hospital).
But helloooo, check out those benefits!!!
So now that we got a grip on what’s in breastmilk and how awesome (albeit often hard) it is to achieve successful breastfeeding, let’s take a look at the physiology.
How is Breastmilk Made?
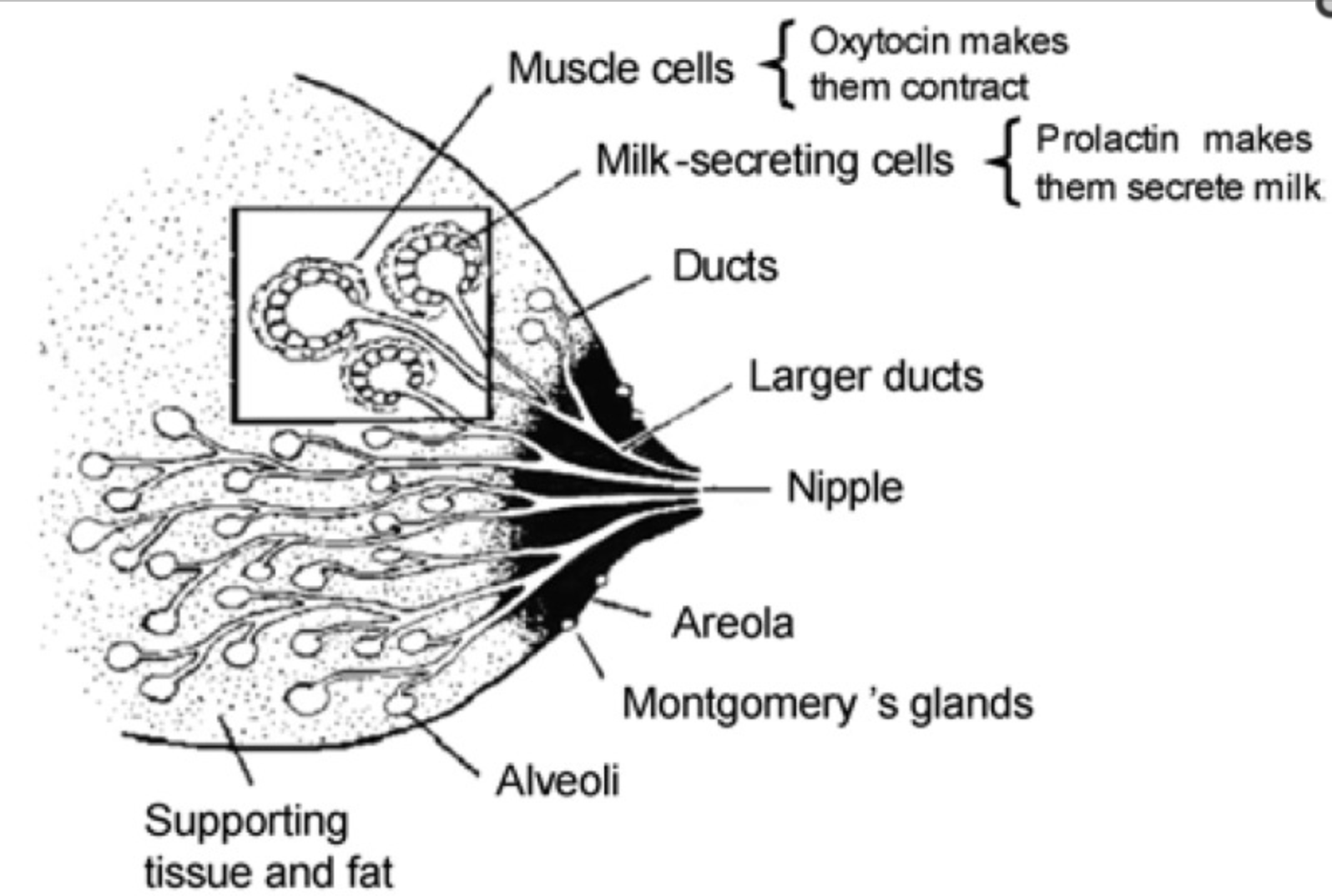
Just like every other part of the body, breasts are comprised of specialized tissues to fulfill their purpose of feeding a baby. Let’s take a look at the anatomy of a female breast:
Squished in with the supporting tissues and surrounding fat are the alveoli, which (just like the alveoli you think of in the lungs) are sacs. Except instead of being filled with air (as in the lungs), these alveoli fill with milk made by the milk-secreting cells. Each alveoli is encased by myoepithelial cells, aka muscle cells, that squeeze the milk from the alveolar lumen into the milk ducts during lactation.
The milk ducts carry milk from the alveoli to the nipple and then outside to a hungry, nursing baby. Each nipple has about 9 ducts that feed it, along with muscles and nerves. The areola (the pigmented circle around the nipple) has Montgomery’s glands, which (fun fact) produce a unique “mommy scent” to help baby know where to latch right after birth.
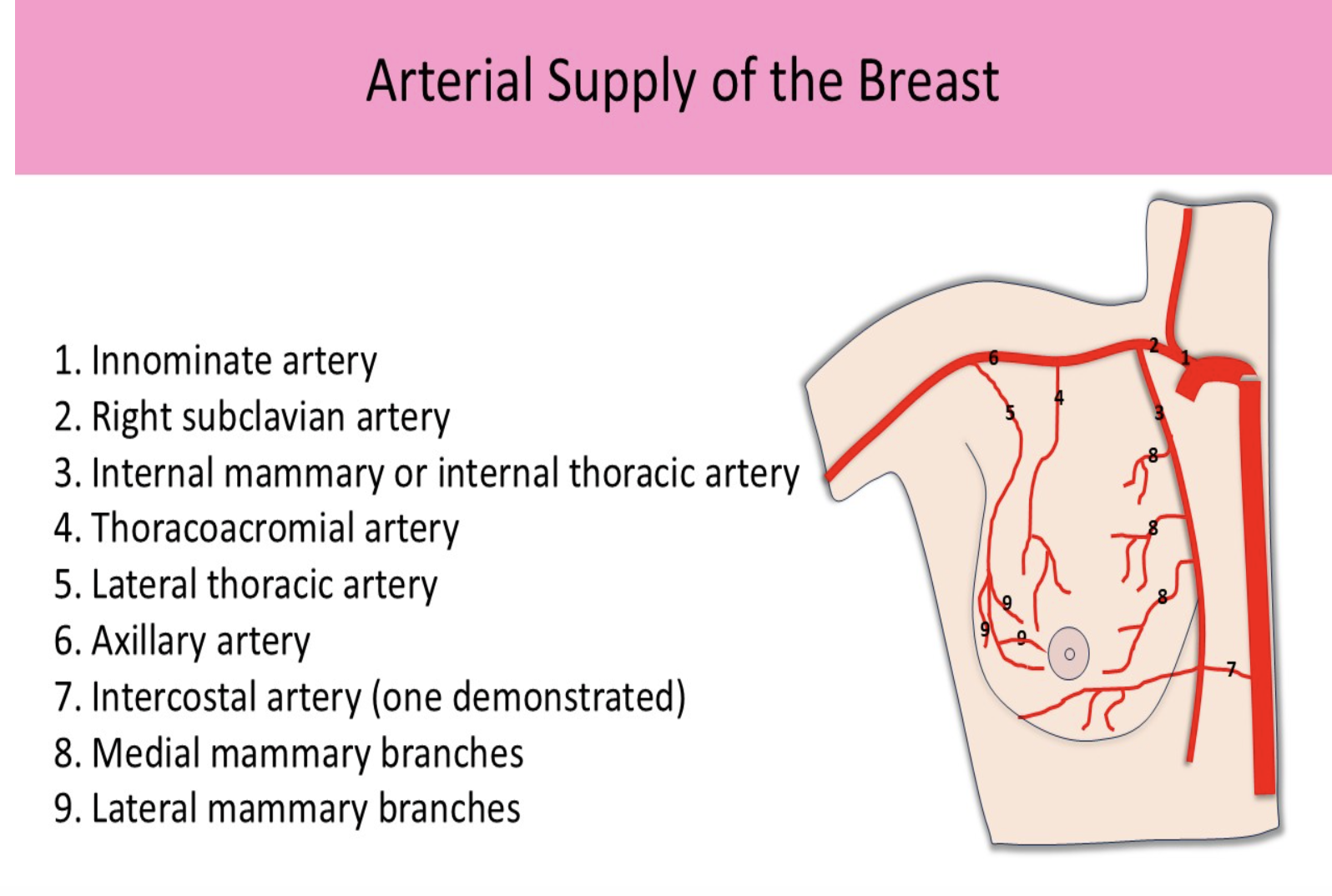
Breast tissue is supplied with blood by several main arteries as shown in the figure below.
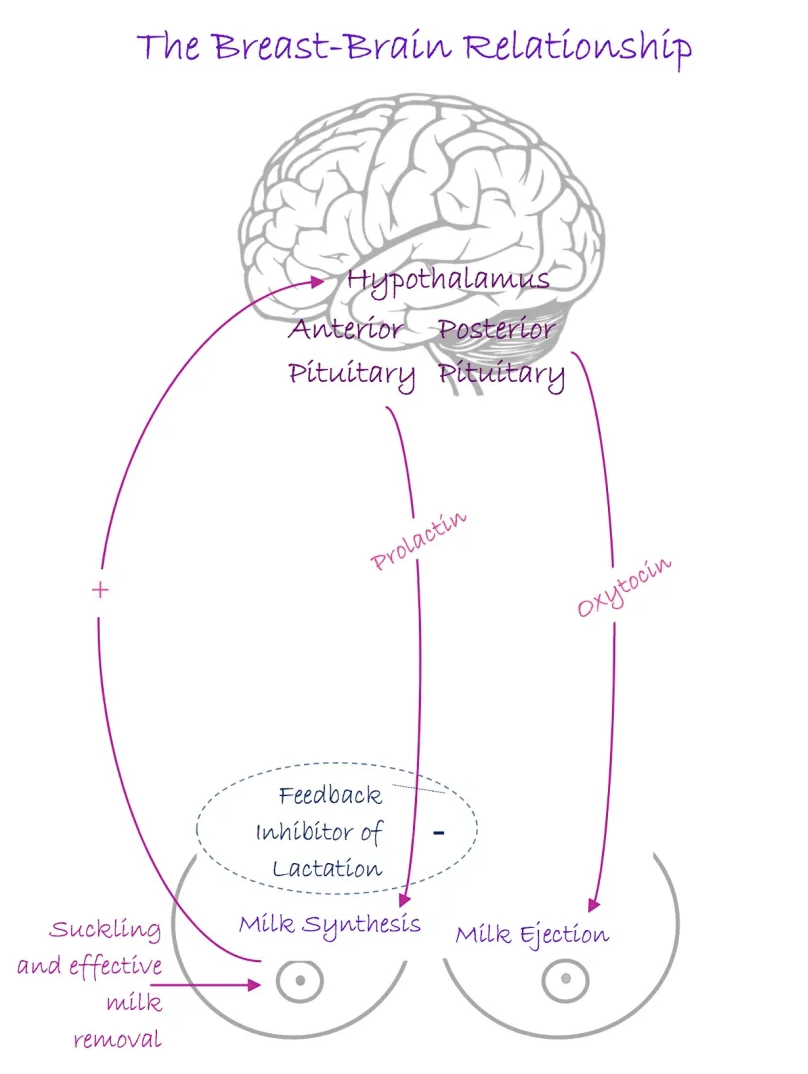
That’s the anatomy. Now let’s talk physiology. Breastmilk is made and released by a system of 3 main substances:
Prolactin
Oxytocin
Feedback inhibitor of lactation (FIL)
Check out the figure to see how these substances play together in the sandbox.
Basically, prolactin stimulates milk production. Oxytocin stimulates milk release (or letdown) via ductal smooth muscle contraction. And FIL is the negative feedback loop to prevent overproduction if milk is not removed from the breast (because clogs are no fun).
Another fun fact is that each breast operates independently of the other. Leftie may be the “hero boob,” producing enough fatty milk for your infant along with 3 others, while Righty is lucky to make 30ml of skim milk. Don’t give up on Righty though… production may be ramped up by continuing to let baby nurse there because production is triggered by suckling and removal of milk!
That is, you can try this if baby doesn’t get too frustrated about the slow tap. #hangrybaby
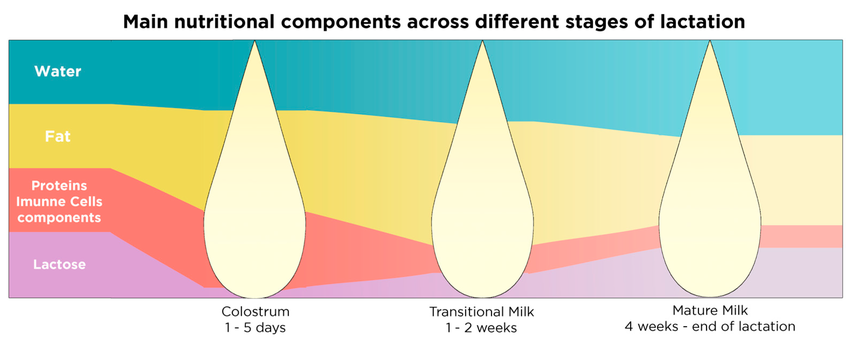
Lactation and milk production are broken down into the 3 stages of lactogenesis as noted below. Although some moms can and do begin pumping colostrum before delivery, appreciable milk production is inhibited by mom’s own placental progesterone. It isn’t until delivery of the placenta (the so called 3rd stage of labor!) that the progesterone blockade drops and full manufacturing can begin.
Alright. Now that we’ve talked about how and where milk is made, it’s time to move into the pharmacy part of this post…
How Medications Interact with Breastmilk
Research is ongoing, but to date, there have been 4 identified modes of transport for drugs to get from mom’s bloodstream into her milk:
Passive diffusion
Active transport
Lipid co-transport
Transcytosis
Let’s take a closer look at each one of these.
Passive Diffusion of Medications into Breastmilk
Passive diffusion is the most common way for drugs to enter the breastmilk from the blood. As you may remember from chemistry class, diffusion is the movement of a substance down a gradient - from higher concentrations to lower concentrations. So it makes sense that medications the mom takes are absorbed into her bloodstream and then travel passively into the breastmilk, where that medication is not initially present.
However, the story isn’t quite so simple as this. Of course, there are other factors that influence how well a drug is able to passively diffuse into milk. They include…
Molecular weight
Medications with lower molecular weights passively diffuse more easily. (Makes sense, right? Larger molecules have a harder time getting through the myoepithelial and glandular cell layers than small molecules.)
Plasma protein binding
Medications that are highly protein bound to mom’s plasma proteins do not diffuse as easily into milk. They’re kinda “stuck” in mom’s serum.
Milk protein binding
While this isn’t thought to be a major factor, it does still seem to play into the equation of creating a gradient. Some medications may bind to proteins in the milk, changing the gradient for passive diffusion.
Drug ionization
Remember, it’s easier for non-charged particles to cross cell membranes than charged ones. Milk’s pH is ~7.1-7.2, which is slightly more acidic than mom’s serum (pH 7.4). So nonionized, weakly basic drugs may cross mammary epithelial cell membranes relatively easily but then become “trapped” after ionizing in the more acidic milk environment. On the other hand, ionized, weakly acidic drugs may not diffuse easily from mom’s serum. These trapping scenarios can alter the gradient for passive diffusion.
Lipid solubility
Medications with higher lipid solubility more easily cross mammary epithelial cell membranes.
So you can see that even though passive diffusion seems like a simple high concentration to low concentration transport method, exactly what that gradient looks like is influenced by a number of factors. On to the next method.
Active Transport of Medications into Breastmilk
When the milk to plasma ratio of drug concentrations is higher than that predicted by (not-so-simple) passive diffusion, it seems to suggest there is another mode of drug transport at play, which leads us to active transport. This is when substances are transported across a membrane using energy and/or protein carriers. Basically, transport proteins in the membranes of the mammary epithelial cells give medications an assist in crossing from blood to milk.
You might think these carrier proteins are special to the mammary cells, but interestingly, I bet you’ll recognize quite a few of these! Some of the mammary epithelial cell transporters thought to influence drug concentrations in the milk include…
P-gp (yep, that same efflux pump protein)
OATPs (organic anion transporters)
OCTPs (organic cation transporters)
BCRP (breast cancer resistance protein)
Now, what’s really intriguing is that expression of these transport proteins changes during lactation! For example, BCRP is upregulated during lactation, which can alter transport of medications like nifedipine and lamivudine. To complicate matters further, expression is not only altered during lactation in general but changes throughout the period of lactation. For example, expression at 2 months post partum is different than at 5 months post partum.
Talk about tricky!
Lipid Co-Transport of Medications into Breastmilk
To understand this method of transport, it’s important to first understand that the fat content of breastmilk is not consistent. And I'm not just referring to being consistent from one breast to the other as previously mentioned. I’m saying fat content changes from the beginning of a nursing session to the end.
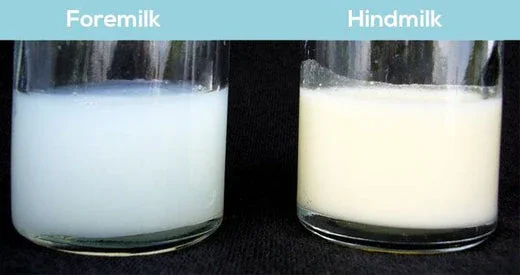
The milk at the beginning of a feed is called the foremilk, and it is equivalent of skim milk from mom. Still full of good stuff, just not as fatty. This is in contrast to the hindmilk, which is the milk released towards the end of a feeding session. It can have up to 5 times more fat than the foremilk! Why does this matter when it comes to medications?
Well, it’s thought that when the mammary epithelial cells are making and secreting milk into the lumen of the alveoli, fat is added by a budding process. Yep, much like we talk about viruses budding off and taking bits of the host cell with them, these fat globules may bud from the mammary cell membrane, taking bits of the cytoplasmic contents with them.
What might be in that cytoplasm? You guessed it. Drugs.
So when fat globules bud off from the mammary cell into the lumen to become part of the milk, they may very well take medication particles with them. Another thought is that medications may cross from mom’s blood into the milk through previously discussed methods only to dissolve into the fat of the milk stored in the alveolar lumen.
Either way, medications may be transported into the milk via fat. And this is where the foremilk versus hindmilk matters. Because some medications have a higher affinity for fat, the amount of medication transferred from mom to baby can vary depending on whether baby consumes foremilk or hindmilk during a feed!
For example, one study found that duloxetine had a 1.4-2 fold higher concentration in hindmilk compared to foremilk. So consider the potential implications for transfer to baby if mom pumps before nursing to encourage a milk letdown, if baby falls asleep before finishing a feed, etc.
Transcytosis of Medications into Breastmilk
Finally, there’s transcytosis, which is the transfer of large molecules across a membrane. These large molecules are endocytosed from the blood into the mammary epithelial cell, transported across the cell, and then exocytosed on the other side into the lumen.
This mode of transport is largely for immunoglobulins, and it is thought to be mediated by the neonatal Fc receptor (FcR). While this method has been studied with regards to transfer of mom’s endogenous immunoglobulins (e.g., SARS-CoV-2 antibody transfer to breastmilk), it’s also been observed with exogenous IVIG therapy. So what does that mean for all the new monoclonal antibody therapies being developed? How will they transfer to breastmilk?
Medications and Breastfeeding
Armed with this background knowledge about how medications pass into breastmilk and what factors may influence that passage, now let’s get practical. You’re at work, you get an order for a medication, and you see that the patient is newly post partum. You think, mmm, is she breastfeeding, and if so, is this medication ok?
This is where your drug references come in handy, especially information from Brigg’s Drugs in Pregnancy and Lactation. And your clinical judgment.
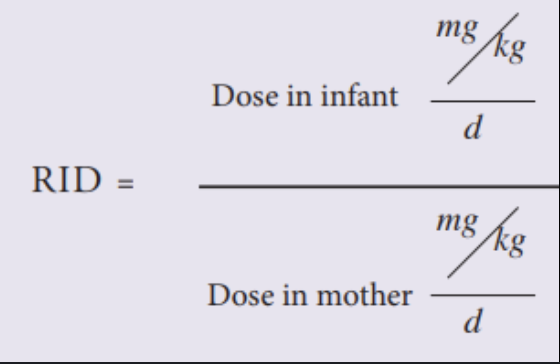
When you look up the drug, it reports an RID, or relative infant dose. This is a calculation based on breastmilk sampling that is supposed to impart information about drug exposure to the infant. The classic formula for RID is in the image here.
Most texts consider RIDs less than 10% to be compatible with breastfeeding, and medications with RIDs greater than 25% should be avoided due to significant potential risk to the baby. However, some countries/organizations are pushing for lower thresholds (e.g., <5% for compatibility) and/or greater breakdowns to assist with decision making. For example, one scheme advocates for classifying RID as follows:
<2%: minimal exposure
2-5%: small exposure
5-10%: moderate exposure
>10%: high exposure
But really, please remember that (like our other big calculations, CrCl, etc) RID is not a black and white tool! It is one piece of a puzzle that should include your clinical judgment. Hypersensitivity can occur in a nursing infant regardless of RID. Breastfeeding should be avoided when moms need cytotoxic therapy, regardless of RID.
Additionally, consider that RIDs are calculated from moms taking standard doses of medications. If your patient is taking a high dose, the RID may be higher than that reported. If your patient is on a normal dose but has genetic factors, drug interactions, or organ dysfunction that impact drug clearance, the RID may not be as reported either.
Baby’s weight, age, and gestational age/maturity should also be taken into account when making determinations. Younger infants tend to be more sensitive to the effects of medications (as you would expect). The liver and those kidneys just aren’t fully mature at birth, not to mention newborns weigh less!
For babies who are not exclusively breastfed, meaning they receive supplemental formula in addition to breastmilk, it’s possible their RID is lower than reported.
So please do use the RID as one tool in your arsenal for making recommendations during breastfeeding. But please do not fall into the trap of forgetting to think critically about each individual patient.
The tl;dr of Medications and Breastmilk
To review, moms make magic milk (ah, you like that alliteration?!). But really, breastmilk is the most complete and individualized functional food there is. With benefits for both baby and mom, it nourishes development efficiently and completely. The breast is anatomically formed to be a micro dairy farm, adding all the necessary components to the milk and then delivering it on demand.
As milk is made, substances from mom (including medications) can be added to the mix by passive diffusion, active transport, lipid co-transport, or transcytosis. How much makes it into the milk from her bloodstream and then into baby’s stomach depends on a wide variety of factors, including drug molecular weight, lipid solubility, ionization, protein binding, transporter protein expression, milk fat content, and nursing practices.
The relative infant dose (RID) is a calculation intended to assist with making decisions about medication use during breastfeeding. Although it is generally considered acceptable to breastfeed if the RID is <10%, additional factors should be taken into consideration, including baby’s gestational age, current age, weight, mom’s dose and drug clearance, and whether baby is exclusively breastfed. Discussions with providers and patients are useful when weighing risk and benefit so that a fully informed decision can be made.
There you have it - the long and short of the wonders of breastmilk. Hopefully this post helps you to better understand the mechanisms by which medications can pass from mom to baby post partum so that you can help your patients make informed decisions about their pharmacotherapies.