'Tis the Season: Let's Chat about the Flu
Steph’s Note: So I’m standing here at work checking prescriptions, and an entire family of Tamiflu scripts comes across my desk. I’m talking everybody from the 4 month old on up to the 37 year old mom. And as I work my way through the verification process, it hits me that I really don’t know as much as I’d like to about this not-quite-so-seasonal-anymore medication. (My thought train really started with the thought of, “Tamiflu for a FOUR month old? Is that worth it?”) Fast forward, and we have this post. Absorb what you need to because we just may see a lot of it this year… Happy holidays!
What is Influenza?
When you think of the flu, you may envision what Hollywood tells us: splayed out on a couch, violent vomiting into a bowl, freezing under a blanket while simultaneously sporting pink fever cheeks, and draining snot like a faucet. (Image)
While some of this portrayal is accurate, once again (just like with its horribly off-base depictions of CPR) Hollywood can be a bit misleading…
Generally speaking, having the “flu” means contracting a strain of the influenza virus, which is a respiratory pathogen. GI symptoms are not usually part of the picture. (Now, if someone says they have the “stomach flu,” that usually does refer to violent emesis and/or diarrhea but is associated with norovirus, which is totally separate from the seasonal flu.)
Let’s take a little trip down influenza lane to make sure we’re all on the same page.
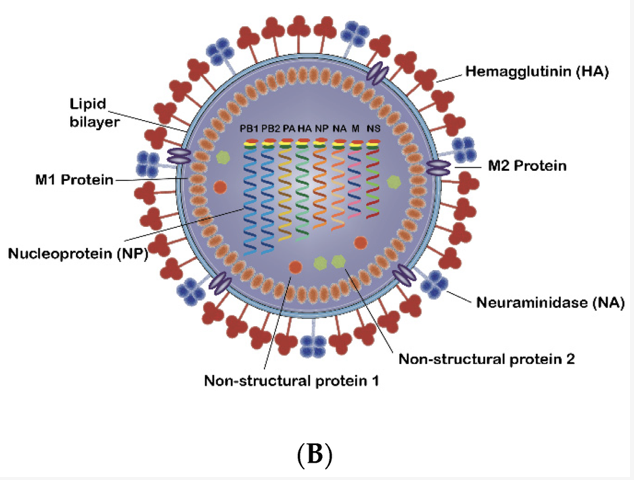
Influenza is caused by the influenza virus. It is an enveloped virus with a lipid bilayer that it steals from its host. (Image) The lipid bilayer is dotted with surface glycoproteins known as hemagluttinins (HA) and neuraminidases (NA), as well as the transmembrane protein M2. Hemagluttinins facilitate viral binding and fusion with the host cell. Neuraminidases aid with viral release from the host. Inside the lipid bilayer is the M1 matrix protein, which contains the viral genetic material and also helps with viral budding.
In the case of influenza, the genetic material is segmented, single stranded, negative sense RNA (ssRNA). Like other viruses (including HIV), this ssRNA must be “read backwards” by viral RNA-dependent RNA polymerase to create messenger RNA (mRNA) that can then be translated into proteins. The segments of RNA can be rearranged…this fun mix and match is the major antigenic shift that causes pandemics. (This is opposed to more minor antigenic drift that drives vaccine makers crazy trying to predict and occurs from smaller mutations in the glycosylation of HA and NA.)
The influenza virus life cycle follows a usual viral hijacking process:
Attachment via hemagluttinins to siliac acid receptors in human bronchial and upper respiratory tissues
Entry into the host cell by endocytosis
Fusion and uncoating of virus particle after pH-dependent opening of the M2 transmembrane protein
Invasion of the host cell nucleus by viral genetic material, where transcription and replication transform viral RNA into viral proteins
Assembly of newly-made viral parts
Budding of new viruses through the host membrane
Release of new viruses after siliac acid residue cleavage by neuraminidase
Viruses aren’t really our friends… but they ARE mooches.
Although the exact receptors and proteins are different, the general scheme is similar to viruses such as HIV: attach, enter, use the host to make more viral stuff, assemble new viral stuff, new viral stuff peaces out to infect other cells. Viruses - such users (and abusers). But it does make it easier to remember since it’s a similar mooching scheme. (Image)
Influenza viruses are classified into 4 flavors based on differences in their proteins: A, B, C, and D. For us humans, types A and B are clinically relevant. Type C usually causes mild symptoms only, and type D infects cattle, sheep, and pigs, not humans.
The subtypes are defined according to variations in their HA and NA glycoproteins. To give some frame of reference, for influenza A, there are currently 18 known subtypes of HA and 11 subtypes of NA. So when you see a designation like H1N1, that’s referring to the H1 hemagluttinin subtype and the N1 neuraminidase subtype. And when you see A/H1N1 or A/H3N2, that refers to influenza A with those subtypes of HA and NA.
It’s not actually gibberish…like it may sometimes seem.
Influenza Season 2025
While it’s not a novel COVID pandemic, the seasonal flu remains a major public health concern every year. For last year’s flu season (Oct 2024 through May 2025), this wily virus is estimated to have caused…
Up to 82 million flu cases
Up to 37 million medical visits
Up to 1.3 million hospitalizations
As many as 130,000 deaths
Looking at CDC estimates for this year’s flu season (through December 13, 2025), so far influenza is thought to have caused…
Up to 8.2 million flu cases
Up to 3.7 million medical visits
Up to 97,000 hospitalizations
As many as 9600 deaths
And we’re only about halfway through the season with the peak numbers usually occurring between December and February! Actually, in the last 40 years, the peak month for flu cases has been February. So TBD on how we’ll fare after making it through the whole season.
What we do know so far is that there may be a mismatch between the influenza strains covered by this year’s vaccine and what is actually circulating. Since the strains to be covered are picked in advance (how else would they be produced for administration ahead of flu season!?), there is a bit of a gamble involved.
It appears that there’s a surprise H3N2 subclade K causing some hubbub since the vaccine was targeted towards the H3N2 subclade J2 based on the end of the 2024-2025 flu season. Apparently, summer vacation allowed the flu virus to do some unexpected changing (much like the kids who come back to school a foot taller than when they left!). (Image)
That being said, experts are still recommending flu vaccination since it is the best way to protect against severe disease. For children especially, the flu vaccine is effectively preventing hospital attendance up to 75% (while adult efficacy is 30-40%). I mean, sure, it’s not as high as we’d maybe like to see, but I’d certainly take a shot in the arm for that reduction in possible hospitalization!
Oseltamivir for Influenza
Now that we know a little more about the lay of the land when it comes to the flu and what’s going on this year, let’s move on to the star drug of the season: oseltamivir. Although there are some other medications that may be used for influenza management (amantadine, zanamivir, baloxivir, etc), this post focuses on oseltamivir as it is by and large the most commonly encountered.
Oseltamivir (Tamiflu) is a prodrug, which when hydrolyzed to its active oseltamivir carboxylate form, inhibits viral neuraminidase. This prevents cleavage of new viral buds from host cells, preventing release and proliferation of the virus.
Dosing for adults is straight-forward. Treatment of influenza calls for 75mg by mouth twice daily for (at least) 5 days, although longer durations up to 10 days may be considered for more severe cases or those who are immunocompromised. Post-exposure prophylaxis dosing is 75mg by mouth daily for 10 days. It is conveniently available as both capsules and a suspension for those unable to swallow pills. Renal adjustments are recommended for CrCl < 60 mL/min and for those on hemo- or peritoneal dialysis.
While not non-existent, the drugs that interact with oseltamivir aren’t exactly numerous or your every day, run of the mill meds. (When was the last time you had someone on probenecid?). But because interactions do exist, albeit with less common (but still used) meds like teriflunomide and leflunomide, it’s always a good idea to cross check.
Oseltamivir is generally well-tolerated with the most commonly reported adverse events being nausea/vomiting (up to 16%) and headache (up to 17%). For the GI adverse effects, these usually occur within the first 2 days of the course and are usually short-lived. Higher doses are also implicated. As for the headache, if you have the flu, what are the odds you also have a headache… Hard to tease out the chicken and the egg there.
One oddity to be aware of is the possibility of psychiatric side effects. Although causation has not been established (and influenza with subsequent encephalitis or encephalopathy could also be responsible), there have been a handful of reports of confusion, delirium, and/or hallucination within the first couple of days of using oseltamivir, especially in children and teenagers. Counseling of patients and/or their caregivers is important so that monitoring is in place.
Evidence for Use of Oseltamivir
As we move into discussing efficacy, we need to take a trip down memory lane. Let’s take a quick look at the study that started it all.
Published in JAMA in 2000, efficacy and safety of oseltamivir was assessed in this randomized, placebo-controlled, double-blind study. It included 629 febrile but previously healthy adults from 60 American health centers who were symptomatic for no more than 36 hours. Of note, these were unvaccinated patients meaning no receipt of the flu vaccine in the previous 12 months. They were followed for 21 days, and the primary outcome was time to resolution of illness after starting study drug. The majority of patients who ended up having the flu had influenza A and were symptomatic for about 24 hours before starting therapy. Oseltamivir 75mg PO BID reduced duration of illness by about 30 hours compared with placebo, and severity was reduced by 38%. Oseltamivir patients returned to their regular activities 2-3 days sooner than placebo patients.
And voila, the oseltamivir era was born.
But has this benefit been seen in the real world? And does it matter that this original study was only in unvaccinated patients? Is the external validity there in a vaccinated (or at least partially vaccinated) population?
Well, good thing we have more info. A new 2024 meta analysis published in The Lancet sought to answer this question using 8 published trials of 1424 eligible patients who received an antiviral against seasonal flu (including oseltamivir, but also peramivir, zanamivir, rimantidine, and baloxivir). For the 4 trials that evaluated mortality, there was very low certainty evidence of antiviral effect with anywhere from 18 fewer to 4 more deaths per 1000 cases of seasonal flu. For the 2 trials that assessed ICU admissions, there was a similar issue of very low certainty: anywhere between 29 fewer to 43 more ICU admissions per 1000 patients. In 1 included trial, oseltamivir decreased duration of hospitalization by 1.63 days compared with standard of care/placebo. In 3 included trials, oseltamivir’s time to alleviation of symptoms was actually longer (albeit by 0.34 days).
Soooo, a bit of a different story than the original 2000 study in terms of efficacy. While current IDSA guidelines do recommend initiation of antivirals for seasonal influenza, those guidelines are also from 2018… It will be interesting to see what changes (if any) are made in future guidelines based on the most recent data.
We’ve talked about the potential benefits of oseltamivir, but does that benefit vary based on time of medication initiation? Let’s look at some details.
If you look at those same 2018 IDSA guidelines, they recommend starting antiviral treatment for outpatient adults and kids with severe flu regardless of illness duration OR those within 2 days of documented or suspected flu onset who are not high risk. But how much does that timing really matter?
In this 2024 study from Clinical Infectious Diseases, over 26,000 adults with lab-confirmed flu were assessed for association between delayed antiviral initiation and 30 day mortality. Mean patient age was 71, and over 90% had at least 1 other health condition. Thirty-day mortality rates were as follows: 7.5%, 8.5%, and 10.2% in those who started treatment on day 0, day 1, and days 2-5 (median 2 days), respectively. Based on adjusted odds ratios, there was a 14% increased risk of death in those who started on day 1 and 40% increased risk in day 2-5 starters compared with those who started on day 0.
Even Arnold’s scary face says not to delay the oseltamivir…
Basically, this study said don’t delay antiviral initiation. (Image)
This 2024 study of 840 hospitalized flu patients also encourages early use of oseltamivir on the day of admission, noting lower peak pulmonary disease severity, as well as lower risks of ICU admission, kidney replacement therapy, vasopressor use, and in-hospital death. So again, don’t delay initiation.
BUT then the question becomes whether it’s still worth starting oseltamivir if it’s been more than 2 days since symptom onset.
Resoundingly, the general consensus is yes. Even if the medication appears to have its greatest benefits when started within 2 days of symptoms, this 2025 study of over 6000 flu patients demonstrated a 30 day mortality benefit of oseltamivir even when started after the 2 day mark (weighted HR, 0.66 [95% CI, .49-.90]). Also of interest, they found that oseltamivir’s benefit was present with influenza A but not B, and vaccination status did not influence this benefit.
The tl;dr of Oseltamivir for Influenza
Flu season is upon us, and we’re heading into peak months now. So bolster your oseltamivir supply because the patients are coming.
So to summarize (we are tl;dr after all!), oseltamivir’s efficacy and benefits are still somewhat uncertain, although evidence seems to point to mortality benefits as well as amelioration of disease severity, especially in hospitalized patients. If the decision is to initiate treatment, earlier is better, whether a person is vaccinated or not.