The Pharmacist's Primer on Anaphylaxis
Carley’s Note: Hi again my phavorite pharmacy phriends! Let's be real, we've all rolled our eyes at an allergy that was very obviously some form of adverse reaction…but that annoyance brings up a much more serious question - what do we do when it's a true, life-threatening anaphylactic reaction? Thankfully, our go-to critical care expert Joe is back to tackle this…no pun intended…critical topic. I know you're going to get a ton of value out of this one. Ready when you are, Joe!
Most of the time, we are overly cautious about avoiding medications because a patient has a documented allergy to X drug. But if you dig deeper and question the allergy, you’ll realize that the majority of these “allergies” are in fact drug intolerances. For example, how many times have your providers avoided all beta-lactam antibiotics because a patient has a documented “allergy” to penicillin? Then you actually click on the allergy and it says “GI upset”. I’m literally rolling my eyes as I am writing this right now.
In case you need a refresher on allergy versus intolerance:
Allergy: a true reaction involving the immune system leading to severe symptoms such as hives, itching, swelling, and difficulty breathing
Intolerance: A less severe adverse reaction to a drug that doesn’t involve the immune system and may be manageable with adjustments to dosage or timing
So, what do you do if your patient has a true allergy? Keep reading :)
Classification of Hypersensitivity Reactions
In 1963, two British immunologists, Robert Coombs and Philip Gell, published a book that introduced the different types of hypersensitivity reactions. No disrespect to them, but they were not the most creative because they named their findings: “Gell-Coombs Classification of Hypersensitivity Reactions”. Surely they could have come up with a more clever name.
Anyway, this is tl;dr pharmacy. If you want a deep review then feel free to purchase their book lol. But for those of us who just want to scrape the surface, here is a table I made that summarizes the most important parts:
As you can see, anaphylaxis belongs to the Type 1 IgE-mediated hypersensitivity reaction. Let’s dive just a little deeper into pathophysiology.
Anaphylaxis Pathophysiology
The pathophysiology of anaphylaxis is extremely complex and would likely require some fancy person who has their PhD in immunology to give you a detailed review. Unfortunately, I am not that fancy guy and I do not have a PhD in immunology. So forgive me if this isn’t detailed enough. But again, my goal is to simplify complex topics.
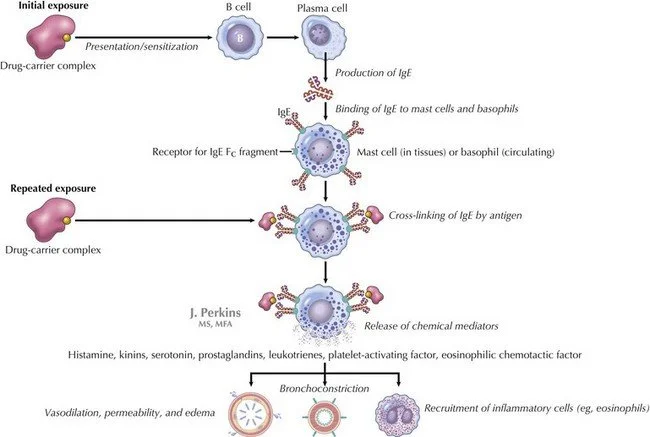
So let’s run it from the top. It all starts with mast cells and basophils.
As a quick refresher, mast cells and basophils are crucial immune cells that play key roles in both allergic reactions and host defense against pathogens. They both release inflammatory mediators like histamine and cytokines. Basophils primarily circulate in the blood while mast cells reside in tissues.
Anaphylaxis is a Type 1 IgE-mediated hypersensitivity reaction that involves the release of numerous chemical mediators from the degranulation of basophils and mast cells after re-exposure to a specific antigen. IgE crosslinking and resultant aggregation of high-affinity receptors induce histamine, tryptase, carboxypeptidase A, and proteoglycans. This isn’t the final step though. These chemical mediators then form arachidonic acid metabolites (thanks to the activation of phospholipase A, cyclooxygenases, and lipoxygenases) including leukotrienes, prostaglandins, and platelet-activating factors. These three final chemical mediators are primarily responsible for the symptomatology associated with anaphylaxis. Specifically:
Histamine: increases vascular permeability and vasodilation leading to tissue hypoperfusion. The body then compensates by increasing heart rate and cardiac contraction (chronotropy and inotropy)
Prostaglandin D: functions as a bronchoconstrictor, simultaneously constricting cardiac and pulmonary arteries. It also potentiates peripheral vasodilation leading to hypoperfusion
Leukotrienes: add to bronchoconstriction and vascular permeability and induce airway remodeling
Platelet-activating factors: act as a bronchoconstrictor and increases vascular permeability
In case you’re a visual learner like myself, here is a picture that summarizes everything we just went over. (Image)
Signs & Symptoms of Anaphylaxis
In most cases, anaphylaxis has a very rapid onset with symptoms presenting within a few minutes of allergen exposure. Most people recognize anaphylaxis by the infamous swelling of the throat, tongue, and lips. While facial swelling is a key symptom, it’s important that we recognize that anaphylaxis involves multiple body systems and symptoms may appear in different combinations. Symptomology of anaphylaxis can include:
Dermal: hives (itchy, raised patches of skin), flushing, itching, or swelling (especially of the face, lips, tongue, or throat)
Respiratory: trouble breathing, wheezing, throat tightness, shortness of breath
Cardiovascular: hypotension, tachycardia
Gastrointestinal: nausea, vomiting, diarrhea, and abdominal pain
Other: dizziness, fainting, confusion, loss of consciousness
Epinephrine: The First-Line Treatment for Anaphylaxis
Epinephrine, epinephrine, and epinephrine. One more time for good measure: epinephrine. I don’t mean to be dramatic, but I really want to stress the importance of epinephrine in the acute management of anaphylaxis. Why? Because epinephrine is the ONLY medication proven to help reverse anaphylaxis and minimize morbidity and mortality. All the other adjunct medications that we will talk about have controversial efficacy. But epinephrine does not. 🙂
Okay, so how does epinephrine work? As most of us know, epinephrine is a vasopressor that is generally used for its inotropic, chronotropic, and vasoconstrictive properties. BTW, if you need a refresher on vasopressors, take a look here. Anyway, back to what we were talking about. Epinephrine primarily works on alpha-1, beta-1, and beta-2 receptors leading to the following effects:
Alpha-1 agonism: vasoconstriction leading to increased blood pressure
Beta-1 agonism: increase in heart rate and contractility force (chronotropy & inotropy)
Beta-2 agonism: bronchodilation leading to better oxygen exchange
In addition to the above mechanisms, epinephrine stabilizes mast cells/basophils by preventing degranulation and release of inflammatory mediators from these cells. This step is key in reversing anaphylaxis. Remember those inflammatory mediators that are released by basophils and mast cells, leading to anaphylaxis? Well, epinephrine inhibits their release.
Based on the pathophysiology that we reviewed above, we can see that epinephrine reduces the release of inflammatory mediators and helps combat the systemic effects caused by these inflammatory mediators.
Pretty cool, right? Okay well, there’s like a million different formulations of epinephrine, right? Kind of. The most common concentrations include:
Anaphylaxis Epinephrine: 1 mg/1 mL (1:1,000)
Cardiac Arrest Epinephrine: 1 mg/10 mL (1:10,000)
Hypotension Push-Dose Epinephrine: 1 mg/100 mL (1:100,000)
Let’s review this really quickly because there have been incidents of people incorrectly pushing the wrong concentration of epinephrine into the wrong route. For anaphylaxis, most of us are comfortable with the premade epinephrine pens. These little guys:
(Image)
These epi-pens make it very simple because we know to inject the entire contents of the pen into the thigh. However, premade epi-pens can be quite expensive and most hospitals do NOT carry them for regular use. Therefore, from the inpatient perspective, we’re generally stuck having to use the 1 mg/1 mL epinephrine vials. These guys:
(Image)
Dosing and administration are fairly straightforward. In regard to dosing, it’s going to be dependent on the patient’s weight:
For Small Children (approx. 7.5 kg to 25 kg / 16 to 55 lbs):
The standard dose is 0.15 mg. This is the dose delivered by an equivalent pediatric auto-injector.
For Larger Children and Most Adults (approx. >25 kg / 55 lbs):
The standard dose is 0.3 mg. This is the dose delivered by a standard adult auto-injector.
For Larger Adults:
For patients where a higher dose is needed (often those >50 kg), a dose of 0.5 mg can be used. This dose must be drawn up manually from a 1 mg/mL vial, as it is not available in a common auto-injector.
The underlying pediatric dose is 0.01 mg/kg. In a hospital setting where you are drawing from a vial, you should use precise weight-based calculations, capped at the standard maximums (e.g., max 0.3 mg or 0.5 mg per dose, depending on the patient and protocol).
(Image)
In terms of administration, epinephrine should always be administered intramuscularly in the anterolateral aspect of the middle third of the thigh.
Now the majority of patients will experience symptom relief fairly quickly after just one dose of IM epinephrine. Rarely does a dose need to be repeated. However, the keyword here is “rarely”. That doesn’t mean never. Depending on the individual and the allergen, some patients may experience a biphasic reaction in which anaphylactic symptoms recur (more on that later). If needed, IM epinephrine may be repeated every ~5-15 minutes if the patient does not adequately respond. There is no true maximum number of IM epinephrine doses that we can give. And if your patient becomes profoundly hypotensive despite several epinephrine IM injections, then a continuous intravenous epinephrine infusion may be started. Again, this rarely is ever needed. But in case it does, now you know what to do.
The Role of Adjunctive Therapy
So we now know that epinephrine is the most important drug. But is there anything else we should give in addition to epinephrine? What about our antihistamines? How about steroids?
Boy do I love controversial topics. There are three controversial drug classes that are commonly used as adjunct therapy in the treatment of anaphylaxis. These include H1 antihistamines, H2 antihistamines, and glucocorticoids. Let’s review what the literature says for each drug class.
H1 & H2 Antihistamines
Let’s get straight to it. There is NO direct evidence supporting the benefit of antihistamines in anaphylaxis and they should NOT be considered part of first-line therapy. As we’ve already discussed a million times, epinephrine is the first-line treatment for anaphylaxis and there is no known equivalent substitute. Therefore, anaphylactic patients who are treated appropriately with epinephrine generally do not need any additional adjunctive agents. If symptoms or signs persist, then more epinephrine should be administered because antihistamines do NOT relieve upper or lower airway obstruction or shock.
(Image)
So, should we never give antihistamines in anaphylaxis? Unfortunately, medicine is not black and white. It’s more gray. Antihistamines should NEVER be given as FIRST-LINE treatment for anaphylaxis. Studies have shown that trying to give antihistamines for the initial treatment of anaphylaxis only led to a delay in the administration of epinephrine, which could be detrimental. Therefore, we should never recommend antihistamines as a first-line treatment option.
That being said, there’s always that 1% where an antihistamine may be considered in anaphylaxis.
Let’s say you have an anaphylactic patient who was appropriately treated with epinephrine. All their life-threatening symptoms, including facial swelling, hypotension, etc, resolved. However, this patient continues to complain of itching and/or urticaria. In this situation, an antihistamine may be considered to help relieve these specific symptoms. So as you can see, an antihistamine is NOT used to treat anaphylaxis. But rather, it is used as an adjunct to epinephrine to help resolve ongoing itching or urticaria. So long story short, antihistamines should only be recommended when a patient's anaphylaxis manifestation has cleared after epinephrine, but the patient continues to report itching or urticaria.
Also, in case you had to Google what urticaria is. Yes, it is just a fancy way to say hives.
One last note. If you are giving antihistamines in anaphylaxis as an adjunct to epinephrine, the intravenous route is generally recommended. Also, remember H1 and H2 antihistamines are NOT first-generation and second-generation antihistamines. First/second-generation antihistamines are both H1 antihistamines. Common H1 antihistamines are diphenhydramine, cetirizine, etc. Whereas common H2 antihistamines are famotidine, ranitidine, etc. Got it? Cool, moving on.
Glucocorticoids
Are you ready for this? This is going to sound very similar to the antihistamine recommendation. There is NO direct evidence supporting the benefit of glucocorticoids in anaphylaxis and they should NOT be considered part of first-line therapy. Literally copy and paste from the antihistamine section. Just changed “antihistamine” to “glucocorticoid”.
I really don’t want to beat a dead horse, but again, nothing is equivalent to epinephrine. It’s really all you need to treat anaphylaxis in 99% of cases. Why complicate it and give more drugs that aren’t necessary? Remember, less is always more.
A little while ago, glucocorticoids were actually recommended in the initial treatment of anaphylaxis. Why? Let me tell you.
There’s this thing called “biphasic anaphylaxis”. Simply put, a biphasic reaction in anaphylaxis is a recurrence of anaphylactic symptoms after an initial anaphylactic episode has seemingly resolved, without any further exposure to the allergen. I am not exactly sure why this occurs, but it can happen. So the initial thought process was to give glucocorticoids to address the late-phase inflammatory response and potentially prevent biphasic reactions.
That sounds super dandy and all. However, a 2020 systematic review failed to find evidence for this effect. Therefore, there likely isn’t much benefit in empirically giving glucocorticoids to prevent the biphasic anaphylaxis.
Much like antihistamines, there’s always that 1% where glucocorticoids may be considered in anaphylaxis.
There are two scenarios in which adjunct glucocorticoids may be considered:
Patients with persistent bronchospasm (especially with known asthma) despite an otherwise adequate response to epinephrine
Patients with severe symptoms requiring more than two doses of IM epinephrine
Much like antihistamines, the intravenous route is recommended, with methylprednisolone being the recommended agent.
The tl;dr on Anaphylaxis
So that’s it, folks. The moral of the story is “anaphylaxis = intramuscular epinephrine”. In case you didn’t have time to read through this entire post (which I recommend you do), here is a quick breakdown that summarizes everything we talked about.
Allergy: a true reaction involving the immune system, leading to severe symptoms such as hives, itching, swelling, and difficulty breathing
Intolerance: A less severe adverse reaction to a drug that doesn’t involve the immune system and may be manageable with adjustments to dosage or timing
There are four different classifications of hypersensitivity reactions. Anaphylaxis belongs to the Type 1 IgE-mediated hypersensitivity reaction and occurs secondary to mast cell/basophil degranulation
Anaphylaxis involves multiple body systems, and symptoms may appear as dermal, respiratory, cardiovascular, gastrointestinal, and neurological
Epinephrine is the ONLY medication proven to help reverse anaphylaxis and minimize morbidity and mortality
Epinephrine 1 mg/1 mL (1:1,000) concentration should be used when treating anaphylaxis
Epinephrine dosing for anaphylaxis is dependent on the patient’s actual body weight:
0.15 mg for small children (7.5-25 kg)
0.3 mg for larger children/adults (>25 kg)
Up to 0.5 mg for large adults (manual draw from a vial)
When used for anaphylaxis, epinephrine should always be administered intramuscularly in the anterolateral aspect of the middle third of the thigh
There is NO direct evidence supporting the benefit of antihistamines or glucocorticoids in anaphylaxis, and they should NOT be considered part of first-line therapy
Antihistamines should only be recommended when a patient's anaphylaxis manifestations have cleared after epinephrine, but the patient continues to report itching or urticaria.
There are two scenarios in which adjunct glucocorticoids may be considered:
Patients with persistent bronchospasm (especially with known asthma) despite an otherwise adequate response to epinephrine
Patients with severe symptoms requiring more than two doses of IM epinephrine