The Pharmacist's Guide to GLP-1 Compounding and Virtual Prescribing
Carley’s Note: Hi, my phavorite pharmacy phriends! It’s been a little while, and I’ve missed you guys so, so much! With that said, a while back we got together and talked about GLP-1 receptor agonists (GLP-1s)…do you remember? It feels like since then, the entire pharmacy world has gotten whiplash. One minute they were the darlings of weight loss, and the next we were all drowning in calls about sketchy telehealth scripts, compounded versions from who-knows-where, and shortages that made the Adderall situation look like a walk in the park. It’s been a lot to process, and it feels like the best way to tackle the whole GLP-1 saga is to treat it like what it has become: a celebrity documentary, one that starts with glamour and ends in a bit of a crisis.
You see, sometimes when people really like their favorite celebrities, they can lose touch of reality a little bit (no judgment, I’m a Swiftie myself). I’m afraid that’s the track we may be on with our friends, the GLP-1s. From the telehealth and overprescribing boom, to the rise in questionable compounding and advertising practices, it’s safe to say that we may need to take a more serious approach to our production this time (don’t worry, the production team will still make it fun). Not to fret, though! This story isn’t all conspiracy and fear-mongering! It’s also a redemption story about exercising good clinical judgment, and advocating for patient safety and access (our favorites!!).
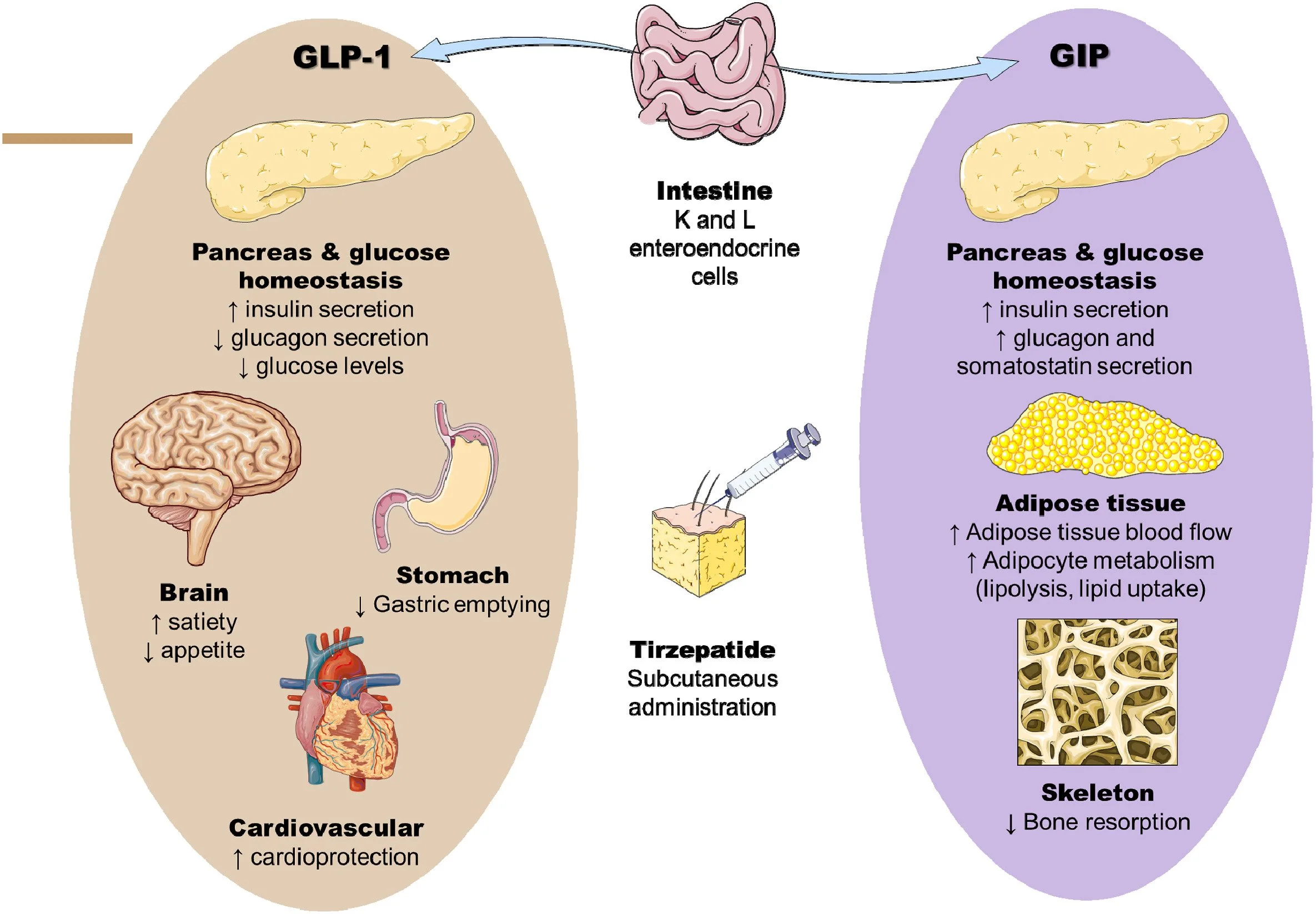
What are GLP-1 Receptor Agonists? A Quick Review
Your brain remembering our first GLP-1 article. (image)
Before we get started, let’s do a quick review of what happened in our first GLP-1 article so everyone’s on the same page. It’s kind of like when you’re getting ready to go see the next Marvel movie!
So, really quick:
Obesity: Obesity has gotten bad, like really bad. WHO reported that obesity had nearly tripled since 1975. With obesity comes risks such as type 2 diabetes, heart disease, stroke, cancer, sleep apnea, etc. etc. etc. NO bueno.
GLP-1 Receptor Agonists: Increased insulin secretion, decreased glucagon and glucose production, slowed gastric-emptying, appetite suppression all packaged together in a beautiful weight loss and blood sugar lowering solution. BOOM - let’s keep it moving.
Semaglutide: We talked about the SUSTAIN-6 trial which showed semaglutide’s potential for an average of 5% weight loss on the smallest dose, kicking the hysteria off. After that was learning the semaglutide dosing dance - remember to titrate that tempo (dose) up!
Other GLP-1s: We discussed another GLP-1, Saxenda, as well as a very important GLP-1/GIP receptor agonist, tirzepatide. These newer drugs were really just breaking onto the scene, but boy did we not know how they would shake the game up.
Bad Stuff: These drugs didn’t come without their problems, even before our shenanigans kicked off. They come with nasty side effects like nausea, vomiting, diarrhea, and constipation. They also have a black box warning for the risk of thyroid C-cell tumors and should not be used in patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2). A history of pancreatitis or gastroparesis also requires extreme caution. I know, drama queens. Don’t worry, we’re going to gossip about this a lot more. Oh, and don’t forget the cost of the brand-name medications! Back then, the average price of GLP-1s was around $1,000 per month. If only we knew then…
Lifestyle: As with all guilty pleasures, these drugs should not be our sole form of therapy. They go best with diet and exercise changes, and when used in moderation.
(Image)
So with that out of the way, let’s pick back up where we left off!
The SURMOUNT Trials: Clinical Evidence for Tirzepatide
Now, when we last talked, these GLP-1s had already generated significant buzz for their waist-trimming benefits, but it was difficult to anticipate JUST how popular they would get. Tirzepatide specifically was the one to watch this time, as the SURMOUNT clinical trials were steadily unveiling its capabilities. Now, you know we love a good clinical trial breakdown…
(Image)
SURMOUNT-1: We had already seen this film before! This trial let us know that tirzepatide had the capacity to help patients without diabetes lose an average of about 20% of their body weight when taking the 15 mg dose.
SURMOUNT-2: This trial was particularly relevant for our friends with diabetes. The results showed that over 72 weeks, patients on the 10 mg dose lost an average of about 12.8% of their body weight, and those on the 15 mg dose lost an average of 14.7% of their body weight! The placebo group? They only saw a dip of 3.2% in body weight. A clear winner for our rising star.
SURMOUNT-3: That’s right, the sequels didn’t stop there. In this trial participants were started on a 12-week intensive regimen of diet and exercise before being randomized to tirzepatide or placebo. By that 12 weeks, the participants had already lost an average of 6.9% of their body weight on their own! Like any predictable sequel though, you can guess the outcome…more weight loss with tirzepatide! That’s right, the group randomized to tirzepatide went on to lose an additional average of about 18.4% of their body weight over the next 72 weeks. Placebo? They actually saw a regain of about 2.5% body weight! Our friends in the tirzepatide group ended up losing about 24.3% of their body weight from the start of the entire study, proving that tirzepatide is most effective when paired with diet and exercise.
SURMOUNT-4: Finally, the trial that helped us understand the long-term sustainability of tirzepatide’s effects. This study placed patients in a 35-week “season” of tirzepatide, achieving an average weight loss of 21.1%. Then, for the next 52-weeks, some patients were randomized to continue the “season” (AKA continue tirzepatide), or to turn the TV off (placebo). Those who kept the tirzepatide around lost an additional 5.5% body weight on average. Those in the placebo group? They actually experienced an average weight regain of 14%. Altogether our friends who continued their tirzepatide led them to a total average weight loss of about 25.3% across 88 weeks. Moral of the story? Tirzepatide provides long-term benefit when continued in these patients!
Now, you know just as well as I do that the industry caught on to these results QUICK. By November 2023 the FDA had given its official approval to tirzepatide for weight loss alone, under the brand name Zepbound. This new approval, combined with the frenzy for Wegovy, off-label Ozempic, and off-label Mounjaro, turned what was a shining viral moment into a global phenomenon by the time it made its red carpet debut in pharmacies in December 2023.
The Rise of Telehealth and Its Impact on GLP-1 Prescribing
Simultaneous to this new drug going viral, we saw a boom in prescribing methods that were a little less traditional. That’s right, we’re talking about the telehealth prescribing boom. What once started as a brilliant idea to increase access during a global pandemic may or may not have quickly spiraled out of control. Before we knew it, every other commercial on our TVs was a telehealth commercial promoting their new, shiny platform to help with mental health, hair loss, erectile dysfunction, and you guessed it…weight loss!
Now, don’t get me wrong - this is revolutionary technology. Patients who may have transportation difficulties, live in rural areas, or simply need a more convenient option to be seen were happy to see a new, reliable way to receive care. On the other hand, this rapid increase in visits, and ultimately rapid increase in prescribing of our GLP-1s led us to a sticky situation.
You see, because of the already mass hysteria surrounding semaglutide, Wegovy and Ozempic had already been on the FDA’s Drug Shortage list since early to mid 2022. When our friend tirzepatide received its FDA approval for weight loss, and simultaneously telehealth platforms increased prescribing of GLP-1s for patients, we saw this shortage situation explode. Imagine if we still had Blockbuster stores, but every single store in your town was out-of-stock of a movie because the demand was THAT high. Yeah, pretty much what happened in pharmacies.
So, with a growing demand for these new medications, and manufacturers scrambling to try and put enough doses out, we were left with a significant deficit in our GLP-1 supplies. That’s when the compounding pharmacies walk in…
GLP-1 Compounding During Drug Shortages
Compounding pharmacies after seeing GLP-1s on the FDA shortage list for the 18th straight month. (Image)
Now, how were the compounding pharmacies able to get in on the situation anyways? You see, per the FDA regulations, when a drug is on the official FDA Drug Shortage list (which our GLP-1 friends all were), compounding pharmacies are legally allowed to prepare “essentially a copy” of that drug in order to meet the patient’s needs. This rule was put in place to make sure patients are able to access their medications, even if there is a supply crisis.
And just like that, the door flew open. Practically overnight we had an entirely new industry of “compounded semaglutide” or “compounded tirzepatide”. It didn’t stop there though - similar to our telehealth boom, these compounding pharmacies started advertising their “copy cat” versions directly to our patients online, on TV, and through those same telehealth platforms we talked about! These ads often used language that mimicked the brand names or made bold, unproven claims, creating further confusion for patients and blurring the line between FDA-approved drugs and their unregulated counterparts. Not only did they glamorize their readily available supply, but they were also sure to remind patients that their drugs came at a cheaper price than those brand-name drugs.
So what’s the problem? More people get GLP-1s, more people lose weight, obesity rates go down, compounding pharmacies fill the supply gap, and everyone’s happy, right?
Not so fast. As always in Hollywood, nothing is ever as it seems on the TV screen. Time for this documentary to take a peek behind the curtain at this production to discuss the safety and sustainability of this cinematic universe.
Compounded GLP-1s: Safety Risks and Regulatory Concerns
Now, when you’re getting your prescriptions from a traditional pharmacy from the manufacturer, you can be positive that you’re getting exactly what was prescribed to you - FDA-approved and all.
Compounded meds? Well, not so much. These could be a high quality copy of our blockbuster film, or a faulty bootleg. While compounding pharmacies are held to rigorous standards for cleanliness, quality control, and training, that does not guarantee their prescriptions’ safety, purity, or even potency. A large reason for the uncertainty around just how quality they are has to do with the difference between 503A traditional compounding pharmacies versus 503B outsourcing facilities.
(Image)
Think of your 503A compounding pharmacy as your local individualized compounding pharmacy. Their whole job in this industry is to create a unique compound for individual patients based on patient-specific prescriptions. This is the traditional compounding we know and love - the doctor sends the pharmacy a prescription, they refer to the most appropriate Master Formulation Record, and then go on to compound an individual prescription for that specific patient. These pharmacies are typically overseen by their state’s Board of Pharmacy and often follow USP guidelines surrounding both non-sterile and sterile compounding. Great oversight, sure, but nowhere near the same strict federal manufacturing rules as big pharma.
Now, 503B outsourcing facilities? They’re a whole production set. They don’t care as much about individualized patient prescriptions, rather they’re focused on mass-producing needed drugs. Because of these large volumes, they have to register with the FDA and follow the same Current Good Manufacturing Practices (CGMP) as major drug manufacturers.
What does this have to do with the boom of our GLP-1 drugs? Well, many of the prescriptions we saw flood the market, whether from traditional or telehealth means, were coming directly from 503A compounding pharmacies who were not built for this scale of production. This is where the lines started to get legally blurry. Remember, we said all of those prescriptions being sent to 503A pharmacies needed to be patient specific. Well, what happens when the compounding pharmacy partners with a telehealth parent company and starts to get thousands of prescriptions? Is each individual prescription still patient-specific, or at that point have you crossed over into drug manufacturing and outsourcing, which would need to be a 503B facility? Not to mention, the differences in oversight between 503A compounding pharmacies and 503B outsourcing facilities led to questions regarding the safety and efficacy of the prescriptions that were being produced…yikes.
It doesn’t stop there, we saw compounding pharmacies also take liberties with the dosages and even formulations they offered of GLP-1s:
Salt forms: The FDA had to step in and warn compounding pharmacies about using different salt forms, such as semaglutide sodium or tirzepatide acetate, instead of the actual base active ingredient found in the FDA-approved molecules. Those salt forms haven’t been FDA-approved, and while they may keep their efficacy, we don’t have data about their safety profiles or adverse effects.
Dosages: We also began to see products pop up on the market in dosages that weren’t specified by the manufacturer, and have never been tested for safety or efficacy.
Multi-Dose Vials: Some compounding pharmacies offered their prescriptions in multi-dose vials, requiring patients to draw their dose up themselves. This escalated so quickly that poison centers reported a more than 15-fold increase in phone calls relating to semaglutide, the majority of which were due to dosing errors, with patients taking incorrect amounts or even double their prescribed dose. There is such a thing as too much of a good thing, after all.
Combination Formulas: Other compounding pharmacies tried to hop on the healthy bandwagon by creating formulations of GLP-1s with other ingredients such as Vitamin B-12, promising decreased side effects or increased benefit, although these combinations have also never been studied and, you guessed it, have no proof to be safe or effective.
To emphasize just how serious all of this is, Eli Lilly, the manufacturer of Zepbound and Mounjaro, issued a direct warning to patients on their website about the dangers of compounded GLP-1s. It doesn’t stop there though! Novo Nordisk, the manufacturer of Ozempic and Wegovy, echoed these sentiments on its global position page, detailing the dangers their own testing uncovered…scary stuff, huh?
Dangers of Inadequate Screening in Virtual GLP-1 Prescribing
If you thought the drama stopped there, you thought wrong! Unfortunately, the problem didn’t just stop with what was in the vial…but also who got them. Traditionally, patients are seen by a provider, have an accurate health history taken, any necessary exams or labs are performed, then, only if it’s the best fit, that provider will prescribe needed medications.
(Image)
That wasn’t exactly the case with our situation. With the boom of telehealth we saw more of an “auditionless” process for getting access to the GLP-1s. Screening processes for the GLP-1s were drastically reduced, and in some cases were as simple as a short online questionnaire. These questionnaires sometimes only evaluated your BMI and health history (which let’s be real, not everyone is a great historian), with complete disregard for family history, thorough exams, or even basic medical history taking practices. This process was clearly optimized for speed and volume, not necessarily patient safety.
The abbreviated processes used by some telehealth companies were simply not designed to catch the different levels of risk. First, they could easily miss the absolute contraindications we talked about earlier, like a personal or family history of MTC or MEN 2. But the danger didn't stop there. These processes also weren’t equipped to handle the grey areas that require real clinical judgment. We're talking about the tough calls - the ones a questionnaire can't handle. Things like knowing to proceed with caution for a patient with a history of pancreatitis, or remembering that the fine print for Zepbound recommends against its use in patients with severe gastroparesis. These are the critical details our provider BFFs are trained to navigate in order to prevent future complications.
There’s one final population that this situation fails to protect - the socially vulnerable. With the immense amount of marketing that was being done for our GLP-1s, we saw an almost equal boom of pressure from the monster that is social media. We saw hashtags like #OzempicJourney and #SkinnyTok, discussions of “Ozempic face”, a flood of transformation photos and videos, and a bombardment of personal experiences that were usually framing these drugs as “one size fits all”. This constant pressure as fans scrolled, including the telehealth and compounding ads within the feed, drove countless people to seek our GLP-1 friends in hopes to achieve a certain “look”, regardless of whether they were clinically obese or appropriate candidates.
This is a common marketing tactic we’ve seen before - find people who are already desperate for change and provide them with a “miracle fix” that is also easy to obtain. This combination of immense pressure, lack of patient education, and minimal screening created a perfect storm. It led to decreased screening for disordered eating histories while completely ignoring the physical consequences of unmonitored rapid weight loss, such as the loss of healthy muscle mass. Ultimately, it allowed what should be a beneficial medication to be used in a way that could be particularly harmful, both mentally and physically. This isn’t just a regression in our screening and prescribing practices, but also a societal regression in which it’s up to us and our provider BFFs to keep those most vulnerable safe.
The Crackdown: FDA Ends Shortages and Halts Compounding
For a while, it seemed like this chaotic, unregulated “production” of GLP-1s would go on forever; however, in late 2024 and early 2025 the drug manufacturers and federal regulators finally decided it was time to start fighting back and end this Wild West era (this was never supposed to be a Wild West film anyways).
The most important domino to fall was the resolution of the official drug shortages. In October 2024, the FDA declared that tirzepatide was no longer in shortage, and shortly after in February 2025 announced the same for semaglutide. Just like that, the legal justification that had allowed thousands of compounding pharmacies to produce these drugs slammed shut. The compounding pharmacies were given clear grace periods to wind down these operations. For tirzepatide, 503A (traditional) pharmacies had until February 18, 2025, and 503B (outsourcing) facilities had until March 19, 2025 to stop their GLP-1 production. For semaglutide, the deadlines were set for April 22, 2025 (503A) and May 22, 2025 (503B). Their message was clear - the show was over, and the loophole that had allowed this industry to flourish was now officially closed.
Simultaneously, the original creators of our GLP-1s, Novo Nordisk and Eli Lilly, took an offensive strategy against the compounding industry. They weren’t just going to let “bootleg” versions of their multi-billion dollar drugs go around without a fight. We saw a flood of high-profile lawsuits against compounding pharmacies, medical spas, and telehealth clinics. These lawsuits weren’t just about money; they were about patient safety and trademark infringement. The manufacturers argued that these compounded versions were unapproved, potentially dangerous, and were confusing patients into thinking they were getting the real, FDA-approved drug. Federal courts and the FDA quickly began to side with the manufacturers, issuing warnings and injunctions that forced many of these back-alley productions to stop.
After the Crackdown: The New GLP-1 Landscape
So what does this new landscape look like? Many of the compounding pharmacies that had built a business model on GLP-1s have had to pivot or shut down their “bootleg” operations. And their telehealth partners who were driving so many of the prescriptions?
Many of them quickly changed their tune. Instead of advertising easy access to cheap, compounded versions of the GLP-1s, some of these telehealth companies have now pivoted to prescribing the manufacturers’ drugs like Wegovy and Zepbound. Their new business model often focuses on a different value now, helping patients navigate insurance prior authorizations for the real-deal GLP-1s.
This still didn’t solve our problem, though. The underlying issues that drove patients to the cheaper alternatives in the first place, like the high cost of these medications and restrictive insurance plans, haven’t disappeared. So, who does that leave waiting in the wing to help clean up this mess, while also improving access and safety for patients? That’s right…us!!! Now we can get to the good part.
The Pharmacist’s Role in the New GLP-1 Landscape
We’ve finally reached the part of the documentary where we stop talking about all of the chaos that ensued and begin talking about the clean-up. While things may have calmed some, the real work of managing the GLP-1s and helping patients navigate the new landscape falls partially on our shoulders as pharmacists.
Me attempting to explain to the patient the difference between their old compounded Tirzepatide and their new FDA-approved Zepbound. (Image)
First up is being vigilant about the switch from compounded to FDA-approved GLP-1s. As patients are switching back to the name-brand medications, it’s important that we reconcile their medications and counsel them to stop usage of the compounded version. This also includes ensuring their transition is safe. Since the potency of the compounded product is unknown, the safest approach is often to start the new, FDA-approved product at its initial starting dose and titrate up according to the manufacturer's instructions to minimize side effects. Also, since these patients may have been using multi-dose vials, it’s important that they’re counseled on using the pen injectors that most GLP-1s are dispensed in.
It’s also important that we emphasize to patients that these drugs are to be used in combination with healthy lifestyle choices, not alone. We should also be screening for both side effects and interactions, and educating our patients on how to handle these things as they arise safely. Remember, screening doesn’t stop there. It’s important to remain vigilant to ensure that overprescribing remains controlled and these medications don’t end up in the hands of patients they may not be safe for over time.
Finally, the elephant in the room, cost. This is still one of our largest remaining hurdles. As patients are transitioning from their often cheaper compounded versions to FDA-approved versions of the GLP-1s, we should take extra care to help patients navigate cost and insurance hurdles such as prior authorizations. Many manufacturers also offer patient assistance programs that may be useful in lowering the cost of these drugs for our patients.
The TL;DR On The Virtual Prescribing and Compounding of GLP-1s
As you can see, our GLP-1 story was a true Hollywood blockbuster. While our GLP-1s are amazing at their weight loss capabilities, they aren’t without their own struggles. The immense telehealth and compounding boom of these medications due to shortage led to an unpredictable, and at times less than safe, environment for providers and patients alike. As this era ends and we look to calm the chaos, it’s important that we remember that as pharmacists, we are perfectly poised to navigate these challenges with our patients. May the next documentary be filled with good screening practices, proper education, and most importantly, patient safety as the priority.