The Pharmacist's Guide to Gestational Diabetes
Steph’s Note: As I sit here 28 weeks pregnant at the doctors’ office waiting to drink my oh-so-yummy glucose drink (no, it doesn’t taste like Gatorade, no matter what they say), I figured maybe now is a good time to fill in another content gap on our site. Much like our recent gap-filling HIV PEP and PrEP posts, we thought we had covered pretty much all the info that most pharmacists might need to know about the big diabetes topics. We have a cheat sheet for the medications. We have posts on insulin therapies (even one specifically on U-500!), oral medications, continuous glucose monitors and insulin pumps, GLP-1 agonists, how to build treatment regimens, and even a fun journal club on SGLT-2 inhibitors. When I say I’ve edited a lot of diabetes posts over the years…I mean for a while, it seemed like this was the only topic I was reviewing!
And yet, there’s another increasingly common topic we’ve missed…gestational diabetes. Sure, this may be a little more niche than your usual type 1 and type 2 diabetes mellitus patients, but it’s not so niche that you have to be a diabetes specialist to encounter these patients. From the community pharmacists who dispense to our inpatient colleagues managing women when they come to the hospital for complications or delivery, it’s a topic with wide-reaching scope in our profession. So let’s get started on filling this knowledge gap!
What is Gestational Diabetes?
Gestation diabetes mellitus (GDM) is diabetes that develops for the first time during a women’s pregnancy, usually the 2nd or 3rd trimester. While it is yet unclear whether pregnancy unveils a chronic, previously undetected issue versus outright causing the issue, we do know that physiologic changes during pregnancy impact glucose metabolism (more in a few). But first, let’s talk scope of the issue.
(Image)
According to the CDC, about 8.3% of pregnant women in the US were diagnosed with GDM in 2021. Increasing maternal age was associated with a pretty linearly increased risk for GDM, and by the time women were over 40 years old and pregnant, their rates of GDM were almost 6 times more than moms younger than 20.
Yay - just one more thing for older moms to have to think about… (And don’t even get me started about the term geriatric pregnancy!)
What are the Risk Factors for Gestational Diabetes?
This is tricky… because GDM can develop in women who have no known risk factors at all. But there are several recognized associations, including the following:
Overweight or obese
Being physically sedentary
History of GDM during a previous pregnancy
History of having a large baby (over 9 pounds) during a previous pregnancy
Hypertension
Polycystic Ovarian Syndrome (PCOS)
History of cardiac disease
A first degree relative with diabetes mellitus
Low HDL <35 mg/dL or high triglycerides >250 mg/dL
So what’s the big deal about having high blood sugars during pregnancy? Aren’t pregnant moms supposed to eat for two and smash pizzas and weird ice cream flavors as much as they want?
Complications Associated with Gestational Diabetes
(Image)
Unfortunately, despite what your body might say about wanting to crush an entire Domino’s large followed by a half gallon of ice cream, pregnancy isn’t actually a free pass. (I say this reflecting on how much pizza I’ve eaten in the last 28 weeks…)
Complications of GDM can affect both mom and baby. For mom, potential issues associated with GDM include a 30% increased risk of delivery by C-section and a 50% higher risk of gestational hypertension (including an increased risk for preeclampsia). Additionally, moms with GDM are more prone to developing type 2 diabetes mellitus (T2DM) later in life.
And we’re not talking just a little increased risk… one 2020 meta-analysis of over 1 million women demonstrated an almost TEN times higher risk of T2DM! Another 2022 study of about 51,000 women put more time context on this increased risk, demonstrating a (lower, but still significant) almost 4-fold increase in T2DM 6-15 years after the affected pregnancy. This risk did decrease as time passed, but it still persisted for more than 35 years.
For baby, potential issues of maternal GDM include premature birth, macrosomia (or large for gestational age, or LGA) and associated shoulder dystocia (injury) upon delivery, neonatal hypoglycemia (along with neonatal hypocalcemia, hypomagnesemia, polycythemia, and hyperbilirubinemia), respiratory distress at birth, childhood adiposity, and increased risk of insulin resistance and diabetes. Generally speaking, GDM (as opposed to maternal pre-existing diabetes) does not confer an increased risk of fetal malformations, although if diagnosed earlier in pregnancy, can not be ruled out as a cause.
Wow. That’s a plethora of hard-hitting, why-we-should-care issues. Hopefully we can all now agree that GDM is a sector of diabetes management we should know!
Pathophysiology of Gestational Diabetes
Maternal glucose metabolism is really just one more example of mom already starting to do everything for her baby (as she will continue to do for the next few decades of life lol). In an effort to reserve precious glucose for her growing baby, mom’s insulin sensitivity decreases in the 2nd and 3rd trimesters. So rather than mom’s muscle and fat cells responding to insulin and gobbling up glucose from the blood, she becomes more insulin resistant, leaving the glucose to pass to her baby for growth. This insulin resistance in mom also leads to more maternal lipolysis and fat oxidation so that fatty acids can be used as an energy source.
What’s driving this insulin resistance in mom? Hormones. Oh, the pregnancy hormones! Sure you’ve heard about how these can make you cry basically every 5 minutes (for no apparent reason), but now you can add messing with your insulin to the list of things these lovely chemicals do to you! Specifically, increases in progesterone, estrogen, cortisol, human placental lactogen, and human placental growth hormone all contribute to maternal insulin resistance.
Now the body typically knows this pregnancy-related insulin resistance is coming, and it will actually ramp up insulin production early in pregnancy before the resistance even starts to occur to try to maintain normoglycemia. But (because of course, there’s a but) not everyone ramps up adequately. It is this insulin resistance and relative insulin deficiency that leads to the hyperglycemia associated with GDM.
Speaking of, what constitutes hyperglycemia in GDM?
Diagnosis of Gestational Diabetes
As with many disease states, there’s been difficulty amongst the experts for coming to a consensus about what exactly constitutes GDM. So there are a couple different strategies, all based on some form of an oral glucose tolerance test (OGTT). An OGTT consists of a patient rapidly consuming a glucose drink (like a bad fruity pedialyte that gives you heartburn) and then having their blood glucose checked at specific intervals to see if their bodies are processing the glucose appropriately.
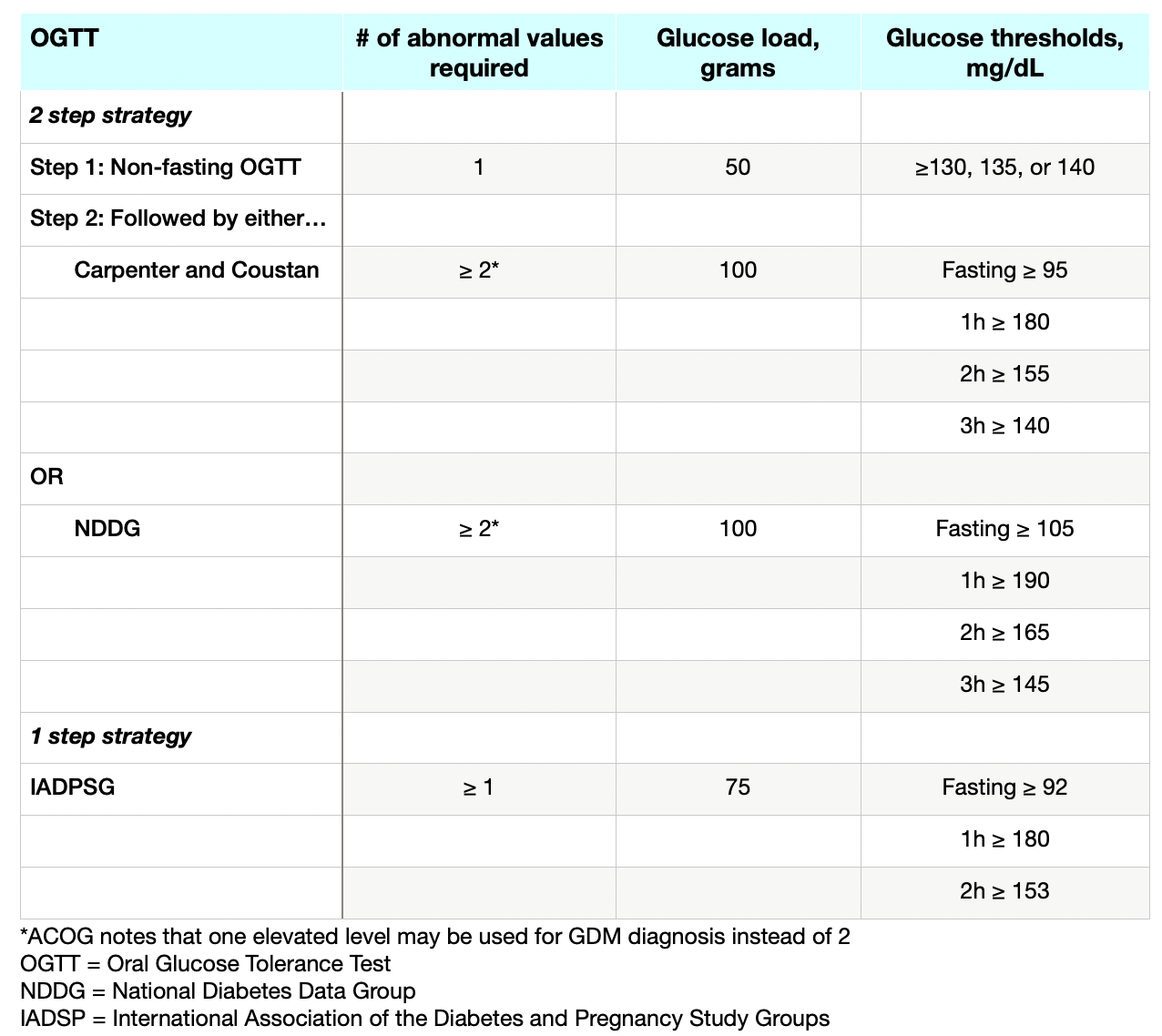
For GDM, most clinicians in the US usually start with the easier 50g glucose, non-fasting, 1 hour venous (not fingerstick) glucose test as an initial screen between 24 and 28 weeks pregnant. If a patient fails this, then they progress to the longer, 100g glucose, fasting, 3 hour test. If a patient has at least 2 of 3 abnormal glucose values, then this is considered GDM. However, the thresholds for abnormal aren’t even completely agreed upon!
Somewhat more recently, the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) has endorsed a one step, 75g glucose, 2 hour OGTT. While the diagnostic thresholds for this test are sourced from the Hyperglycemia and Adverse Pregnancy Outcomes Study and reflect real-world neonatal risks of outcomes, this strategy has not gained as much traction. There’s a concern for increased GDM diagnoses without the necessary support resources, as well as questions about the true benefits.
So speaking of inconsistencies in diagnostic criteria and various strategies, check out this table with the tests and thresholds for GDM:
Just for funsies, let’s take a minute to compare how these values line up with diagnosis of T2DM in non-pregnant patients based on an OGTT. According to the 2024 ADA guidelines, T2DM diagnosis should be considered (and an additional test used for corroboration) if a 2 hour glucose level is ≥200 mg/dL following a 2 hour, 75g glucose OGTT. So the 2 hour thresholds in pregnant women are actually more conservative (allowing for increased diagnosis), even when assessing the same 75g glucose load of the IADPSG strategy.
Assuming a patient meets one of the above criteria for GDM, the next question is this - how do we manage this disease state, and how effective will that management be at preventing associated complications?
Management of Gestational Diabetes
Target blood glucose values for a patient with GDM.
First, since we’ve talked about the elevated blood glucose values that land a woman in GDM land, now let’s talk about where her values are ideally supposed to be. Target blood glucoses are (again) more conservative for a GDM patient than for a non-pregnant woman. Check them out to the right here:
Now, how do we achieve these goals?
As for any patient with hyperglycemia and diabetes, the first step is making changes to diet and lifestyle. There’s even evidence that up to 85% of women diagnosed with GDM can be managed with these changes alone, meaning they don’t require pharmacotherapy at all!
How refreshing to find a disease state that may not actually require medications to meet treatment goals, right? We’re pharmacists, but less is often more.
In terms of what these diet and lifestyle changes are, they’re pretty much what you would expect. Limit simple carbohydrates (candies, etc), and incorporate complex, nutrient-dense carbohydrates instead (e.g., whole grains, legumes, fruits, etc). Reach for monounsaturated and polyunsaturated fats rather than saturated (or GASP, trans) fats. Don’t try to cut out carbohydrates entirely because then the body shunts to lipolysis, which increases free fatty acids and can actually make maternal insulin resistance worse.
Of course, these changes are sometimes easier said than done, especially if mom is busy with a demanding job, chasing other kids, and just plain stressed out. Then, that pack of Pop Tarts looks like a fast, easy win. But not for her or her developing baby (*she keeps telling herself*)
So moms-to-be with GDM are asked to make these changes (often in concert with a nutrition consult), and they monitor their fasting and post-prandial blood glucoses for 1-2 weeks. If they are still not meeting their goals (usually >15-20% of readings above goal), then it’s time to add in the pharmacotherapy - which is refreshingly simple for GDM: insulin, insulin, or insulin!
While you may have heard about metformin or glyburide historically being used for GDM, these have fallen out of favor due to their ability to cross the placenta. Metformin can result in umbilical cord levels just as high - if not higher - than concomitant maternal levels. Glyburide reaches levels up to 70% of mom’s. Both medications have been linked to negative childhood effects in studies, so it’s best to just avoid them.
In contrast, none of the commercially available preparations of insulin have been shown to cross the placenta. Woohoo! While some practitioners may prefer insulins studied in randomized controlled trials (e.g., NPH, regular, and detemir) over those only investigated in cohort studies (e.g., glargine), the patient’s individual needs also help to drive the ship in practice. Some patients may not be able to adhere to the multiple daily injections associated with the older formulations.
(For a review of all the different insulins and their kinetics, check out this post.)
Locations where a pregnant woman may inject insulin. The belly is still preferred! (Image)
Now, you may be wondering… where do women with GDM inject the insulin considering their bellies are ever growing? Although it may seem uncomfortable, the abdomen is still the recommended site for insulin injection during pregnancy since this is where insulin absorbs in the most consistent manner. The standard rule of at least 2 inches away from the belly button applies.
As her belly gets bigger and the skin becomes more taut, it may be necessary to move sideways further away from the belly button and try to fold up some skin between the fingers in order to get the injection into fatty tissue. Other options like the upper thighs and the backs of the arms are also fair game, although absorption isn’t quite as consistent - making monitoring crucial.
How Does GDM Affect Labor and Delivery?
The degree to which labor and delivery is affected by GDM is really determined by how well controlled the mom’s hyperglycemia is. If mom has managed to achieve her glycemic goals with lifestyle and diet management alone, she may progress through a normal pregnancy course with no need to plan an induction or timed delivery. If mom requires pharmacotherapy to achieve her glycemic goals, it’s recommended to deliver during the 39th week. In women who have not been able to meet their glycemic goals, delivery should be planned between 37-38 weeks (to try to avoid delivery of a too-large infant!).
Women with GDM, even those who have managed with diet and lifestyle changes alone, may require initiation of an insulin infusion while laboring if their glucose levels rise higher than 100-126 mg/dL. Again, this is to try to prevent the dreaded occurrence of neonatal hypoglycemia upon delivery (from the baby’s overproduction of insulin in response to maternal hyperglycemia). Both mom and baby will require glucose monitoring after delivery, although the cool part is that women with GDM can usually discontinue all treatments after delivery!
How are Moms with GDM Monitored after Delivery?
Between 4-12 weeks after delivery, mom should do another OGTT to test for the persistence of diabetes, and it’s recommended moms continue to be screened every 1-3 years for diabetes given the increased risk after GDM. Those continued screenings, whether hemoglobin A1c, fasting glucose, or OGTT, should follow the normal thresholds for diabetes diagnosis rather than the GDM thresholds.
So there you have it - GDM in a nutshell! Hopefully this post will help you to be able to compare and contrast this special population with our other diabetes folks and understand how management affects outcomes for both mom and baby.