Continuous Glucose Monitors and Insulin Pumps: A Guide for Pharmacists
Brandon’s Note: If you pay attention when you’re out and about, there’s a good chance you’ve seen these little pods on the backs of peoples arms…and it was most likely a Continuous Glucose Monitor. Here to educate us on CGMs and Insulin Pumps is tl;dr team member, Carley Moses, PharmD. Take a peek at her previous posts on Pediatric Vaccines, Adult Vaccines, GLP1-agonists, and Chronic Care Management. Take it away, Carley!
Hi again, my beautiful pharmily! Today, we will talk about some of the coolest diabetes management technologies. I'm talking about continuous glucose monitors (CGMs) and insulin pumps. We're also going to talk about some of the important things for patients and healthcare pros to consider when using these devices to ensure we maximize benefit while minimizing some of the scarier sides of diabetes. First, let’s review some blood sugar basics.
Blood Glucose Basics
The best defense against hypoglycemia is a strong offense.
Hypoglycemia: We may also call him low blood sugar; hypoglycemia occurs when blood glucose levels drop below a specific number, usually around 70 mg/dL.
Patients might experience dizziness, confusion, sweating, or even unconsciousness. It's essential to act fast and treat hypoglycemia with a quick source of glucose, like fruit juice or glucose gel.
Heck, I’ve even heard of people using tubes of icing - just something with a quick glucose burst.
Hyperglycemia: On the flip side, we have hyperglycemia, which is high blood sugar. This happens when blood glucose levels rise above 180 mg/dL after meals or over 130 mg/dL when fasting. Symptoms include the poly-triplets: frequent urination (polyuria), excessive thirst (polydipsia), and excessive hunger (polyphagia). Continued hyperglycemia may lead to long-term complications like neuropathy, retinopathy, or kidney disease.
Treating hyperglycemia involves adjusting insulin doses, modifying diet, or increasing physical activity.
Given that, it’s no wonder there’s an increased need for technology to provide us with quick, accurate information relating to blood sugar. The more our patients know what their blood sugar is, the more they can make good decisions to prevent complications related to both low AND high blood sugar - alright, I’ll stop my elevator pitch for CGMs and pumps and get to the real meat now.
Overview of Continuous Glucose Monitors
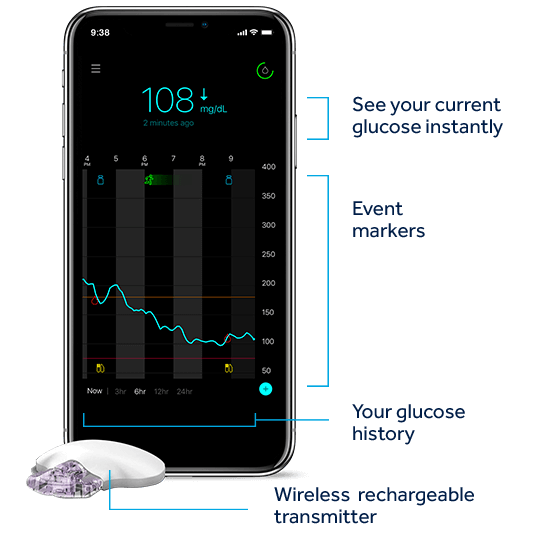
Continuous Glucose Monitors (CGMs) are amazing little tools that monitor glucose levels in the fluid under the skin. They give you real-time info on your blood sugar levels. There are two main types: Real-time CGMs (rtCGMs) and intermittently scanned CGMs (iscCGMs). RtCGMs constantly send you updates, while iscCGMs need you to scan the sensor for the info (Remember those scanners in stores that would tell you the price of things? Kind of like that…except you scan and get your blood sugar). CGMs provide patients with real-time information about their blood sugar levels and can help them make more informed decisions about diet, exercise, and insulin dosing. It’s kind of like they have their own diabetes personal assistant always handy.
Some of the CGM devices currently available on the market include:
Dexcom G6/G7: rtCGMs that provide real-time glucose readings and can be used with a compatible smart device or receiver. Dexcom CGMs are also commonly compatible with various insulin pumps making blood sugar reading and control more convenient. The G6 and G7 devices can be worn for up to 10 days.
Freestyle Libre 2: an iscCGM that requires the patient to scan the sensor with a receiver device or smart device to obtain glucose readings. The Freestyle Libre 2 also includes optional alarms for high and low glucose levels. The sensors for the Freestyle Libre 2 can be worn for up to 14 days.
Freestyle Libre 3: a rtCGM that provides real-time glucose readings and can be used with a compatible smart device. The Freestyle Libre 3 includes optional alarms for high and low glucose levels and can also be worn for 14 days, similar to its sibling the Freestyle Libre 2.
Eversense: a rtCGM that uses a sensor implanted in the patient's upper arm. It’s important to note that due to the longevity of this sensor, a small procedure is required in order to place the sensor. The sensor can be worn for up to 180 days and provides real-time glucose readings through a compatible smart device or receiver.
Medtronic Guardian Connect: a rtCGM that provides real-time glucose readings and can be used with a compatible smart device or receiver. The Guardian Connect also includes optional predictive alerts for high and low glucose levels. The sensor for the Guardian Connect can be worn for up to 7 days.
When counseling patients on CGMs, we should emphasize the importance of proper application and maintenance of the device. CGMs are typically applied to the upper arm or abdomen and require regular calibration to ensure accurate blood sugar readings. Patients should be advised to follow the manufacturer's calibration instructions and keep the sensor site clean and dry. If patients face issues with the sensor staying attached, advise them that many retailers sell patches that can be placed over the sensor to help them last their full duration (and they come in cute designs)!
Overview of Insulin Pumps
Insulin pumps are another tool in the diabetes management toolkit. These devices deliver insulin continuously throughout the day and can be programmed to deliver bolus insulin doses to cover meals and those pesky late-night snacks. We’ve talked about insulin pumps before, and busted quite a few myths related to them, so be sure to check out that article to get up to speed.
Insulin pumps come in a variety of types, including:
Traditional Pumps — These pumps are connected to the patient's body through a tube that delivers insulin from a reservoir to the infusion site.
Patch Pumps — Also known as tubeless pumps, these devices use a small adhesive patch to deliver insulin directly to the infusion site. Patch pumps are ideal for patients who may be uncomfortable with the tubing used in traditional pumps.
Partially Closed Loop Pumps — These pumps use CGM readings to adjust insulin delivery automatically but require the patient to input bolus doses manually.
Closed Loop Pumps — Also known as artificial pancreas systems, these pumps use CGM readings to adjust insulin delivery automatically, including bolus doses.
Some of the insulin pump devices currently available on the market include:
Medtronic MiniMed 780G: a partially closed loop pump that uses CGM readings to adjust basal insulin delivery and requires the patient to input bolus doses manually.
Tandem t:slim X2: a partially closed loop pump that uses CGM readings to adjust basal insulin delivery and allows patients to enter bolus doses directly into the pump or through a compatible smartphone app.
Omnipod: a patch pump that delivers insulin directly to the infusion site without the need for tubing. The Omnipod also has a touchscreen controller for easy programming and dosing.
Note that these are not all of the insulin pumps currently available on the market but rather an example of the different devices and technologies available for our diabetic friends. Watch for new device approvals from the FDA as this technology develops daily.
When counseling patients on insulin pumps, we should stress the importance of proper insulin dosing and monitoring - we can’t be having our patients out here overdosing on their insulin and having hypoglycemic events, now can we? Patients should be advised to work closely with their healthcare provider to determine appropriate basal and bolus insulin doses and to regularly monitor their glucose levels with a CGM or blood glucose meter.
Patients also need to understand the maintenance and upkeep required for insulin pumps. Patients should follow the manufacturer's instructions for changing infusion sets and reservoirs. Usually, infusion sets need to be changed every 2-3 days, while reservoirs typically need to be changed every 3-7 days, depending on the individual's insulin needs and the reservoir's capacity. Some patients may be able to extend the lifespan of their infusion sets and reservoirs by carefully following good maintenance and hygiene practices, such as keeping the infusion site clean and dry, rotating infusion sites, and properly storing and handling their insulin and pump supplies.
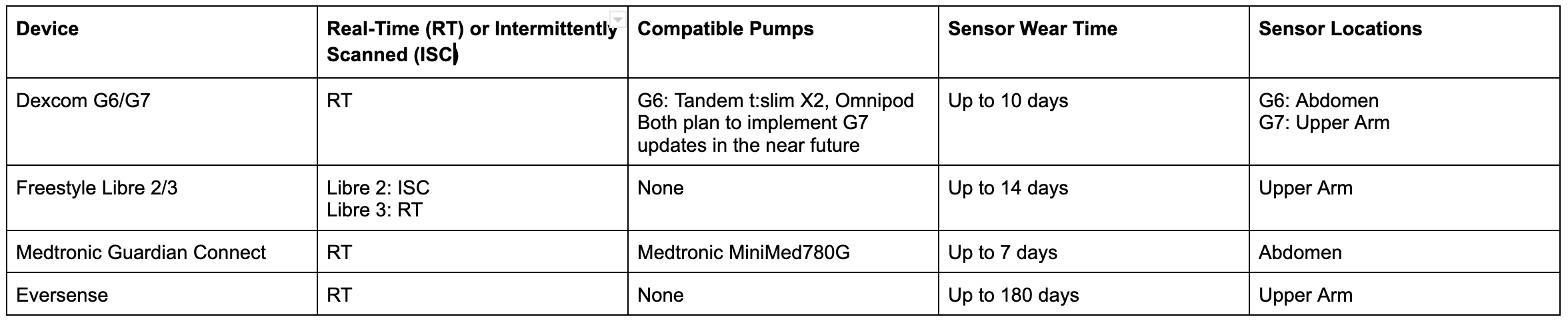
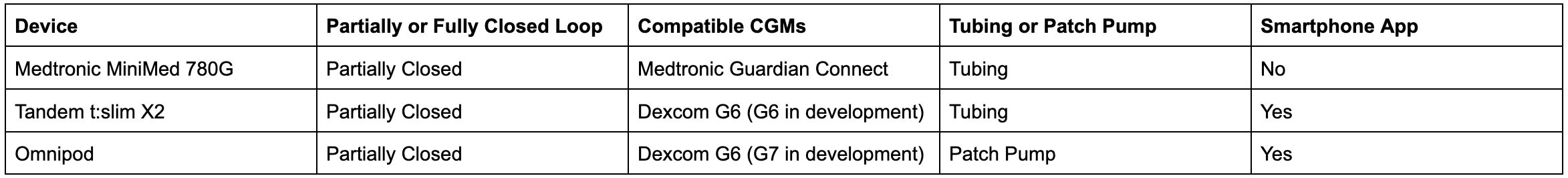
Now, that was a lot of info - so let’s break this down into a table format.
Comparison of Continuous Glucose Monitors
Comparison of Insulin Pumps
How to Use a Continuous Glucose Monitor or Insulin Pump
Now that we have an idea about some of our devices let’s walk through the journey of both so you get the inside scoop on what it's like to have these little game-changers by your side.
Step 1: Getting Everything in Place
Clean that skin, load the applicator, and press the button to apply the CGM to the abdomen. Feel a pinch? No worries, it's over in a flash! Now, set up the insulin pump, following the device-specific instructions for filling the reservoir and attaching the infusion set.
Step 2: Attach and Activate
Snap-on the CGM transmitter, activate it with your smartphone, and boom! You're in business. Attach the infusion set for the pump, prime it, and you're rockin' and rollin' with your new devices.
Step 3: Wearing and Using Your Devices
Shower time? Most CGMs and pumps can handle a splash, but always check those instructions (no one wants a technology meltdown, think of it like a brand-new iPhone or something). Trouble with sticking? Grab those adhesive sprays or covers and slap 'em on. If the readings seem funky, have that traditional fingerstick glucometer on standby (better safe than sorry!).
Step 4: Understanding Readings and Dosages
Regular scans or real-time data? Dive into the data on your devices, and you'll start to see trends, understand your body's reactions, and get a grip on managing those glucose levels. Insulin pumps? They'll help you nail those doses. Learn to love the bolus button and the convenience it offers; just make sure you're in sync with your healthcare squad for the best results.
Step 5: Sensor and Pump Maintenance
CGM sensors usually last around 7-14 days, depending on the model. Insulin pump reservoirs and infusion sets? Usually, 2-3 days, depending on maintenance and upkeep. Keep up with replacements, and you'll be a pro in no time.
Tired of reading about it? Well, this one’s for you visual learners. Let’s have a mini movie night and watch a couple of videos showing how our CGMs and pumps are applied and connected. This is just one example of a common pairing - the G6 monitor with an Omnipod pump. As we all know, you can find anything on YouTube, so feel free to peruse to find information about your patient’s specific CGM or insulin pump.
Dexcom G6 — How To Insert the Sensor and Attach the Transmitter
Omnipod® 5 Automated Insulin Delivery System Product Training - Pod Activation
Omnipod® 5 Automated Insulin Delivery System Product Training - Connect to Sensor
Insulin Calculations for Insulin Pumps
One of the benefits of insulin pumps is the ability to make super-duper-precise insulin dosing calculations based on the patient's individual needs. Insulin pumps can deliver both basal insulin (a continuous, low dose of insulin throughout the day to help keep patients’ baseline blood sugar in check) and bolus insulin (a larger dose of insulin to tackle meals and snacks).
Most insulin pumps use rapid-acting insulin analogs, such as insulin lispro or insulin aspart, for bolus doses. For basal insulin, pumps may use either rapid-acting or long-acting insulin analogs, depending on the patient's needs. As a pharmacist, your patient or one of your practitioner-homies may look to you for help in some of the calculations related to these devices…fear not! We know you can handle them.
Bolus Insulin
This rapid-acting insulin covers the carbs in meals. To calculate bolus insulin, you'll need the insulin-to-carb ratio (ICR), which is the number of grams of carbohydrates covered by 1 unit of insulin. For example, an ICR of 1:15 means 1 unit of insulin covers 15 grams of carbs.
Let's say a patient has an ICR of 1:10 and plans to eat 50 grams of carbs. The bolus insulin dose would be:
Bolus insulin = Carbs ÷ ICR = 50 grams ÷ 10 = 5 units
Basal Insulin
This long-acting insulin keeps blood sugar stable between meals. To calculate basal insulin, first determine the patient's Total Daily Dose (TDD) of insulin. TDD is typically calculated based on the patient's weight in kg. A common starting point is 0.5 units/kg/day.
For example, if a patient weighs 70 kg:
TDD = 0.5 units/kg × 70 kg = 35 units
Now, to determine the basal insulin dose, take 40-50% of the TDD. For our 70 kg patient:
Basal insulin = 0.5 × 35 units = 17.5 units (rounded to 18 units)
Correction Factor (CF)
CF, or insulin sensitivity factor (ISF), corrects high blood sugar levels. It's the number of mg/dL (or mmol/L) that 1 unit of insulin is expected to lower. For instance, a CF of 1:50 means 1 unit of insulin will lower blood sugar by 50 mg/dL.
To calculate the correction insulin dose, use the following formula:
Correction insulin = (Current blood sugar - Target blood sugar) ÷ CF
Suppose a patient has a current blood sugar of 250 mg/dL, a target of 100 mg/dL, and a CF of 1:50:
Correction insulin = (250 - 100) ÷ 50 = 3 units
We should emphasize the importance of proper insulin dosing and calculation to patients using insulin pumps. Remember - low blood sugar is more acutely dangerous than high blood sugar! Make sure as you’re covering these numbers with your patient that you are also covering their plan, should they experience a hypoglycemic event.
Cost and Insurance Considerations for CGMs and Insulin Pumps
The cost of CGMs and insulin pumps can vary widely depending on the device and the patient's insurance coverage - but they’re definitely not cheap. We have to work with the patient’s insurance provider to figure out their coverage for CGMs and insulin pumps, including any copays or out-of-pocket expenses.
It's also worth noting that some insurance providers may require prior authorization or other documentation before covering the cost of these devices. This documentation may include the frequency with which the patient is currently checking their blood sugar, injecting insulin daily, adherence to their blood sugar checking regimen, and data related to their diabetes diagnosis. Helping to gather or verify this information can help to speed up the prior authorization process to ensure that the patient gets their device in a timely fashion. We’re shooting for Prime level delivery speeds here.
Insurance Considerations for Travel, Vacation, and Unfortunate Events
Patients who use CGMs and insulin pumps may need extra precautions when traveling, going on vacation, or just navigating the unfortunate events of daily life. Here are some of my favorite tips to guide them through their adventures, whether it’s a flight to a tropical paradise or a road trip to Grandma's house.
Carry-On Essentials: Remind patients to carry devices, infusion sets, reservoirs, and adhesives in their carry-on luggage for easy access. TSA agents may ask about these, so no shame – we've all been there.
Extra Supplies for Extra Fun: Pack more infusion sets, reservoirs, and other supplies than they think they'll need. Better safe than stranded without the necessities!
Local Options: Research local pharmacies or medical supply stores at the destination. Transferring prescriptions can be part of the adventure.
Adhesives for Adventures: Stock up on special adhesives or covers that keep the CGM or pump in place during active or water-filled vacations. Bonus points if they pick a fun pattern for their cover that matches their vacation destination.
Keep It Cool: Watch out for those devices and insulin in hot weather. Tropical vacations are fun; unstable insulin is NOT!
Know Your Zone: An 8 a.m. insulin administration time on the East Coast is not the same as an 8 a.m. insulin administration time on the West Coast! Ensure the patient’s devices (and brain) are prepared for any time changes - unfortunately, diabetes does not experience jet lag.
Backup Insulin Plan: Discuss a backup insulin plan, including types of insulin and dosing strategies. It's all about being ready for whatever comes their way.
Manual Checks: If the CGM or pump falters, finger-sticks for blood glucose monitoring and manual insulin administration become their trusty sidekicks. Make sure they know how to do it and that they have those supplies handy with them!
ADA Guidelines on CGMs and Insulin Pumps
The ADA has published guidelines related to the use of CGMs and insulin pumps as part of the overall management of diabetes. These guidelines are updated regularly to reflect new research and technological advances.
For CGMs, as of Summer 2023, the ADA recommends that they be considered for patients with type 1 diabetes who have not achieved their blood sugar goals with traditional glucose monitoring methods or for patients with frequent hypoglycemia. CGMs may also be considered for patients with type 2 diabetes who require insulin therapy.
Regarding insulin pumps, the ADA recommends that they be considered for patients with type 1 diabetes who have not achieved their blood sugar goals with multiple daily injections or for patients with frequent hypoglycemia or hypoglycemia unawareness. Like their sibling, insulin pumps may also be considered for patients with type 2 diabetes who require insulin therapy.
The ADA guidelines also emphasize the importance of individualizing therapy based on the patient's needs and preferences and considering factors such as age, how long they’ve had diabetes, and any comorbidities they may have. The guidelines note that using CGMs and insulin pumps requires ongoing education and support and that patients should be trained on their proper use and maintenance (*cough cough* that’s your job *cough cough*).
Additionally, the ADA recommends that healthcare providers work closely with patients to develop individualized blood sugar targets and treatment plans and that patients should be monitored regularly for blood sugar control and any potential issues.
Future Developments for CGMs and Insulin Pumps
As diabetes management technology continues to evolve, exciting developments are on the horizon. One of the most promising research areas is the development of closed-loop systems, which use CGM readings to automatically adjust insulin delivery and dosing (no more manual inputting of bolus doses!). These systems have the potential to improve diabetes management and reduce the burden on patients greatly.
Another area of research is the development of non-invasive CGMs, which would eliminate the need for frequent fingerstick testing or even the application of a transmitter. Some non-invasive CGMs in development use sensors that can be worn on the skin (what can’t smartwatches do nowadays?), while others are exploring the use of optical or other non-invasive methods to measure glucose levels.
As technology rapidly develops, we should stay up-to-date on the latest developments in diabetes management technology and be prepared to counsel patients on the benefits and risks of new devices as they become available.
The tl;dr of CGMs and Insulin Pumps
So, there you have it, guys! CGMs and insulin pumps are complete game-changers when it comes to handling diabetes. Picking the right device, nailing those doses, and staying on top of monitoring will seriously help your patients take control of their glucose levels and live their best life. Stay informed as technology evolves and collaborate with your healthcare squad to maximize the benefits of these fantastic gadgets!