Acute Stabilization of Severe Bleeds Part 2: Initial Management of Traumatic Brain Injuries & Intracranial Hemorrhages
Steph’s Note: Ladies and gentleman, after taking a couple of months off since Part 1 of this acute bleed series, we’re so back. And by we, I really mean Dr. Josef Nissan, who is our critical care expert extraordinaire of vasopressors, heparin-induced thrombocytopenia, acetaminophen toxicity, and methemoglobinemia fame (not to mention various other work with us, like our critical care pocket guide). We’re back hungrier than ever to teach about acute stabilization of severe bleeds!
If your break happens to include chocolate, ain’t nobody gonna judge you here. (Image)
In Part 1, we talked about anticoagulation reversal in patients with acute severe/life-threatening bleeds. In Part 2 (aka this post), we’ll shift our focus to the acute management of traumatic brain injuries/intracranial hemorrhages. Lastly, we’ll finish off the series with Part 3, in which we will talk about the management of gastrointestinal and variceal bleeds.
Alright, let’s start. But I am going to warn you. This is a pretty hefty topic. Both clinically and emotionally. There is A LOT information that goes into this. So unless you’re a super go-getter, I recommend you take breaks when reading this article to help your brain digest all the information.
The Basics of Traumatic Brain Injury
This is tl;dr pharmacy. So if you think I’m going to give you some super duper in depth medical explanation of what a traumatic brain injury is, then think again.
So what’s a traumatic brain injury according to tl;dr rules? Pretty self-explanatory. Traumatic brain injury (TBI) is when there is an impact, penetration, or rapid movement of the brain within the skull that results in an altered mental state.
Classifications of TBIs
There are two main types of TBI:
How many closed TBIs do you think Wile E. Coyote had over the years? (Image)
Open (aka penetrating): the scalp/skull is broken, fractured, or penetrated
Examples: a gunshot wound to the head, arrow to the head, hammer to the head, etc.
Closed (aka blunt): outside force impacts the head, but the skull is NOT broken, fractured, or penetrated
Examples: Have you ever seen a boxer (the athlete, not the dog) get knocked out mid fight? Do you usually see an external skull fracture? Generally speaking, no. This is classified as a CLOSED TBI. Reason is, all the damage/swelling/bleeding is within the skull. No evidence of skull fracture or penetration is apparent from the outside.
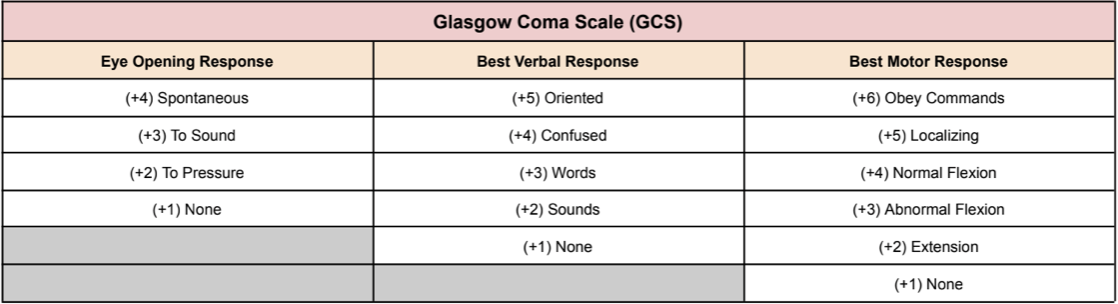
How can we classify severity of a TBI? We use the Glasgow Coma Scale (GCS) Score. How do we calculate that score? Simple, we use the table below:
Using the GCS score, we can classify a TBI as…
Mild: GCS Score of 13-15
Moderate: GCS Score of 9-12
Severe: GSC Score of ≤ 8
Signs & Symptoms of a TBI
Just like everything else with medicine, it’s complicated. Signs and symptoms of TBIs are dependent on so many factors, including severity of TBI, time since injury, baseline, age, and so on. So take this with a grain of salt. But in general, a TBI may present like this:
Within 30 minutes of injury: headache, blurry vision, nausea/vomiting, vertigo
Within 24 hours of injury: confusion, disorientation, difficulty speaking, memory loss
After the first 24 hours: loss of consciousness/comatose state (if a severe TBI)
Pathophysiology of TBI
The pathophysiology of TBIs can be separated into two main categories: primary brain injury pathophysiology and secondary brain injury pathophysiology. Here’s a quick overview of the two:
Primary brain injury
Occurs at the time of trauma and is caused by a penetrating or blunt force
Leads to tissue deformation, axonal shearing, contusion, necrosis, and blood-brain barrier disruption
Secondary brain injury
Occurs at the time of trauma and continues for hours to days
Caused by a cascade of molecular injury mechanisms
Leads to cerebral edema, neuro-inflammation, mitochondrial damage, excitotoxicity, and ischemia
The Basics of Intracranial Hypertension
If you listen closely, you’ll hear them whispering about the scariest Condition-That-Must-Not-Be-Named… ICH! (Image)
By the time this post is published, it’ll probably be October. (Oops, turns out it’s December!) Which means there’s only one thing spookier than Halloween…
Intracranial hypertension.
Let’s be real, would you rather walk through a haunted house or be the sole pharmacist in the hospital when a physician calls asking for help with the management of intracranial hypertension?
I suppose we should define what that is so you can make an informed decision. If not obvious enough by the name, intracranial hypertension is a clinical condition associated with an increased pressure in the cranium. Normal intracranial pressure (ICP) in adults like you and me is <20 mmHg. Anything higher than that is classified as intracranial hypertension (ICH).
To be specific:
Normal: <20 mmHg
Mild Intracranial Hypertension: 20-30 mmHg
Moderate Intracranial Hypertension: 30-40 mmHg
Severe Intracranial Hypertension: >40 mmHg
Why is intracranial hypertension so deadly? Simple, because our skulls are hard and rigid.
For illustrative purposes, think of a balloon. If you fill a balloon with water, that balloon will expand. The more water you put in, the more the balloon expands (until it eventually pops). Well, our skull is nothing like that. When someone has an intracranial bleed, does our skull expand like a balloon would? No.
(Image)
So where does all that building pressure and edema go? The only place it can go, which is back down towards the brain stem.
And why is that a death sentence? Because our brain stem houses the medulla oblongata. The medulla oblongata is the control center for our heart and lungs. If damaged, our heart and lungs stop…which means death.
This super simplified explanation right there is what we call brain herniation. Here is a picture to help illustrate what I just explained:
(Image)
Management of Intracranial Hypertension
Now that we’re intracranial hypertension experts, let’s talk about how we can manage this disease state. While I do love drugs (the legal ones, geez people), non-pharmacological interventions are just, if not more, important than pharmacological interventions here. That being said, below is a quick overview of all the intracranial hypertension treatment options that we are going to review in this post:
Non-pharmacological treatments
Surgical interventions
Head elevation
Hyperventilation
Pharmacological treatments
Sedation/analgesia
Hyperosmotic therapy
Chemical paralysis
Barbiturate coma
Non-Pharmacological Management - Surgical Interventions
I am a critical care pharmacist. So think again if you think I am going to dig deep into all the different kinds of surgical procedures that can be done to help reduce intracranial pressure. Plus, this is tl;dr. So here’s the name of the possible procedures along with pictures that will help better explain them. And FYI, don’t worry, these pictures aren’t that grotesque.
Non-Pharmacological Management - Head Elevation, Hyperventilation, Therapeutic Hypothermia
Yes, these are fairly important acute interventions that can be made to help reduce intracranial pressure. However, we’re not going to spend a lot of time discussing them because this is a pharmacy website and we love drugs (again, legal ones). But for completeness sake, here is a summary of the other non-pharmacological interventions that can be recommended in patients with intracranial hypertension:
So, are you a non-pharmacologic wizard now? I hope so. Now, on to the fun part. Pharmacological interventions.
Pharmacological Management - Sedation/Analgesia
As you probably already know, patients with moderate to severe intracranial hypertension will need to be intubated since they generally can’t protect their airway. Initiating sedation and analgesic drips will hit two birds with one stone! First, they allow the patient to be comfortable while there’s a tube stuck down their throats (aka post-intubation sedation & analgesia). Second, sedatives/analgesics also lower ICP.
How, you ask?
By sedating the patient, we decrease their cerebral metabolic rate of oxygen. As a result, this decreases energy demands, leading to decreased cerebral blood flow and ICP.
Which agents should we use? Check out this little table I made for you :)
Pharmacological Management - Hyperosmotic Therapy
Let’s be honest, there is a very strong chance you skimmed through this entire post just to get to this part. I don’t know why, but I swear us pharmacists make hyperosmotic therapy scarier than it needs to be. We’re all so scared of it and will do anything to avoid it.
But eventually, it’ll sneak up on ya. So here at tl;dr, we want you to be prepared for when you have to administer hyperosmotic therapy.
To make this as simple as possible, let’s use an example.
Patient GG is a 67 yo female who presents to your ED after being found down and altered by EMS. She was intubated en route given her inability to protect her airway (GCS of 7). A CT of the head was completed and shows a severe intracranial hemorrhage with a midline shift.
Now, let’s walk through it. Does this patient have intracranial hypertension? Yes, given the severe head bleed with a midline shift.
How can we treat her intracranial hypertension? First, we should implement the non-pharmacological interventions including possible surgical interventions (if indicated), head of the bed elevation, acute hyperventilation, and therapeutic hypothermia (if indicated).
Second, we should start post-intubation sedation and analgesia to help decrease cerebral oxygen demands leading to decreased cerebral blood flow and therefore decreased ICP.
Now what? This is when we’d start hyperosmotic therapy. How do these agents work? Simple, let’s go back to our Gen Chem class from freshman year of college.
(Image)
Fluid (water) always follows areas with high chemical concentrations (high osmolarity). Same thing happens in our brain. Giving hyperosmolar therapy increases our intravascular osmolarity, causing the edema in the brain to be sucked into the peripheral vasculature. By decreasing the cerebral edema in the brain, we are decreasing the intracranial pressure. Make sense?
Ok, so what are our hyperosmolar drug options? Hypertonic saline and mannitol. Which is better? Literature is very conflicting, and the general consensus is that they’re pretty equivalent in terms of morbidity and mortality. Personally, I like hypertonic saline a lot more, and I’ll tell you why later on. But for now, here’s a small overview comparing the two agents:
So, why do I like hypertonic saline more than mannitol? Two reasons. First, mannitol is a pain in the butt to administer. You need to use like a million vials for each dose (unless your institution carries the premix bag). The vials also need to be placed in a little heating chamber because they can crystallize so dang easily. You also need to use a filter needle when administering to the patient.
If mannitol was your girlfriend. (Image)
Second, mannitol is a diuretic meaning it has negative effects on your mean arterial pressure (MAP). Why does this matter? Because higher MAPs are needed to maintain good cerebral perfusion pressure (CPP) in patients with intracranial hypertension. What is CPP? It’s the net pressure gradient that drives oxygen delivery to cerebral tissue. How do we maintain good CPP? By using this formula:
CPP = MAP - ICP
To optimize cerebral perfusion pressure, we need to increase MAP and decrease ICP. Let’s dig deeper.
Hypertonic saline effects: ↑MAP & ↓ICP
Mannitol effects: ↓MAP & ↓ICP
So as you can see, hypertonic saline should theoretically elevate/maintain cerebral perfusion pressure better than mannitol. For that reason and for the fact that mannitol is a pain to administer, I personally like hypertonic saline more.
Alright, now that we know why I love hypertonic saline, let’s talk about the different common hypertonic saline formulations. Here’s a table I made that sums everything up:
Pharmacological Management - Chemical Paralysis
Let’s be clear, chemical paralysis is NOT for every patient with intracranial hypertension. It’s primarily indicated for severe cases in patients with refractory intracranial hypertension despite trialing the above interventions. How does paralysis lower ICP?
Chemical paralysis → limits systemic muscle contraction → ↓ Intrathoracic resistance → ↑ Outflow of blood from the brain → ↓ ICP
While there are some advantages, chemical paralysis does come with a list of disadvantages/risks as well. Let’s review:
If the provider elects to utilize chemical paralysis to lower ICP, here are some of the common agents that may be used:
Pharmacological Management - Barbiturate Coma
I, luckily, have never had to initiate pentobarbital on anyone. Why not? Because it’s the absolute last-line option for refractory intracranial hypertension. This is not something that can/should be initiated in the majority of patients with elevated ICP. Generally, the above non-pharmacological and pharmacological interventions are more than sufficient to lower ICP. However, in case you ever have to use it, here is a brief overview:
The tl;dr of Acute Management of Traumatic Brain Injuries/Intracranial Hemorrhages
Phew. That was a lot of information. Like I said earlier, take breaks when reading through this post. Read it over multiple times. There is a lot of information to digest. But I am very confident that you will be an intracranial pressure wizard in no time. If not, here’s a couple things that I hope you can at least remember:
Non-Pharmacological Management of Intracranial Hypertension
Surgical interventions
Burr hole, craniectomy, craniotomy
Head elevation
Head-elevation of at least 30° is recommended
Hyperventilation
May be utilized for temporary control of elevated ICP to allow implementation of other interventions
Therapeutic hypothermia
Cooling the core temperature to 32-35°C may be an effective intervention for elevated ICP refractory to other medical management
Pharmacological Management
1st-line: sedation/analgesia, hyperosmotic therapy
Refractory intracranial hypertension: chemical paralysis, barbiturate coma
There you have it! Stay tuned for Part 3 of this acute bleed series, in which we’ll discuss gastrointestinal and variceal bleeding.