Acute Stabilization of Severe Bleeds Part 1: Reversal of Anticoagulation
Steph’s Note: This week, we welcome back one of our favorite tl;dr voices of 2023 - Dr. Josef Nissan. In between authoring pharmacotherapy pocket guides and cheat sheets, he spends his free time working as an ICU/ED pharmacist. Or is it vice-versa?? Honestly, with how much content he’s produced this year alone, I’m not actually sure which is his primary job! J/k, he’s a rockin’ ICU/ED pharmacist first - and tl;dr author extraordinaire second. :) Alright, Joe, tell us about this latest project!
A little while ago, I got a message from one of our readers requesting a post about the acute management of bleeds. Here at tl;dr, we never let requests go unanswered (because we’re awesome). So being the courageous writer that I am, I decided to tackle this task.
(Image)
That being said, management of acute bleeds is such a broad topic that can’t be covered in just one post.
Cue the drum roll.
Welcome to my very first topic series. In part I, we will focus on anticoagulation reversal in patients with acute severe/life-threatening bleeds. In part II, we will shift our focus to the acute management of intracranial hemorrhages. Finally, we will finish off the series with part III, in which we will talk about the management of gastrointestinal and variceal bleeds.
Shall we begin?
“Hey, What Should We Use to Reverse...”
Oh come on. Don’t be afraid. If it hasn’t happened yet, it will. The infamous question that every provider will ask you at one point in your career:
“Hey, what should we use to reverse...?”
And in case you still don’t think this topic is that important, just know I got anticoagulation reversal questions on my NAPLEX, BCPS, and BCCCP exams. While you may feel a little underprepared now, I promise that you will be an anticoagulant reversal wizard by the end of this post. Let’s dive right into the deep end.
The Clotting Cascade
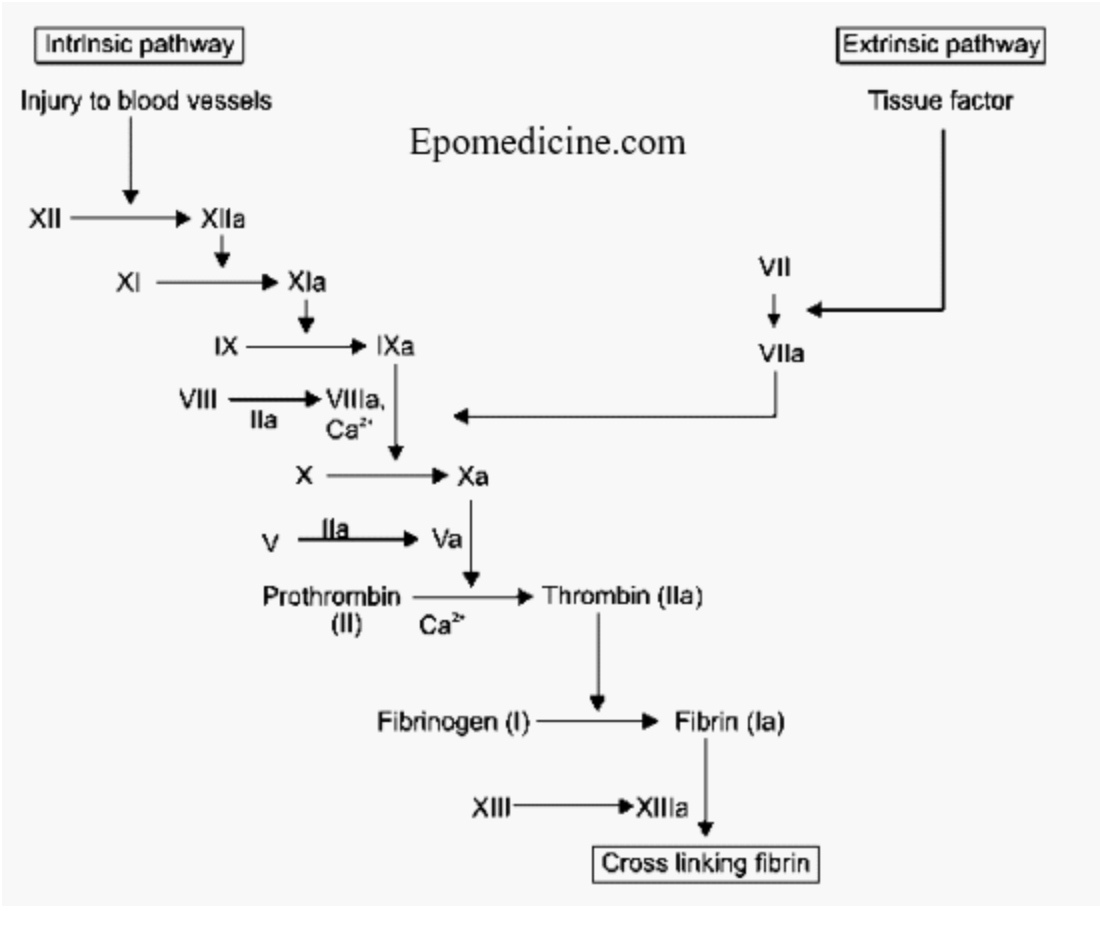
Ah, I see. So you’re like me. Memorized the clotting cascade for the NAPLEX and haven’t reviewed it since? Well unfortunately, to understand anticoagulation reversal, we first need to understand how anticoagulants inhibit the clotting cascade. Once we know that information, reversing them is a piece of cake.
Let’s review the clotting cascade with this beautiful and simple picture that I have placed below:
That dreadful clotting cascade (Image)
How Anticoagulants Work
Alright, so have you committed the clotting cascade to memory? Next step is to review the mechanisms of action of the different anticoagulants. Anticoagulants may inhibit various steps in the clotting cascade; however, the final result is the same…inhibition of fibrin/clot formation.
Simply put, the clotting cascade is like dominos (no, not the pizza). No matter where you inhibit the clotting cascade, everything else comes falling down since the subsequent steps are incapable of occurring. For completeness sake, take a quick look at the table I made below:
Definite hemorrhage… There’s no clot here after that domino effect. (Image)
Do you see the recurring theme? That domino effect I was referring to? As long as you inhibit part of the clotting cascade, everything else comes crashing down with the final outcome being the inability to form fibrin (clot).
Warfarin Reversal
Let’s start with the infamous “rat poison.” Just kidding. (I mean, kinda… Warfarin was used as a rodenticide in the 1950s! Even though that information is clinically irrelevant at this point, patients still love to bring up that fact. Like I was literally negative 46 years old when this was a thing. Why are we still talking about it?)
Anyway, back to what actually matters.
So warfarin reversal is pretty simple. As we discussed earlier, warfarin inhibits Vitamin K Epoxide Reductase (VKOR) leading to a depletion of functional vitamin K. Without vitamin K, our liver cannot synthesize new clotting factors including factors II, VII, IX, and X. (For a full review of warfarin, check out this previous post.)
So, how would we treat an acute bleed secondary to warfarin toxicity? Simple, reverse the mechanism of action of warfarin!
Administer vitamin K to help promote new endogenous clotting factor production in the liver. However, our liver takes a few days to produce these new clotting factors. Considering a significant bleed is an acute medical emergency, we don’t have a few days to wait around while our liver produces clotting factors to stop the bleeding.
So what can we give in addition to vitamin K to reverse warfarin in the acute setting?
Administer clotting factors. Since we said warfarin inhibits factors II, VII, IX, and X, let’s give the patient a product that has all four of those clotting factors to help replenish any deficiency secondary to warfarin use and promote acute clotting to reverse a bleed.
What’s this magical product, you ask? 4F-PCC (4-factor prothrombin complex concentrate).
Easy, right? Now let’s discuss dosing. Take a look at the nice and pretty table that I made below for you. Two important things to always consider when reversing warfarin are evidence of acute bleeding and INR level.
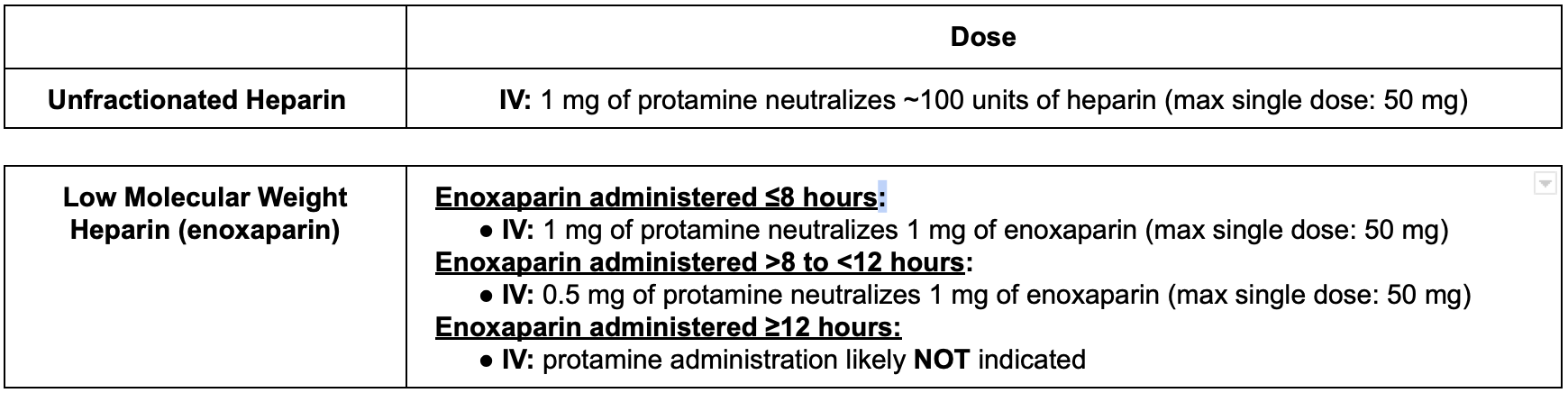
Unfractionated Heparin and Low Molecular Weight Heparin Reversal
On to the next beast. This one is probably my favorite because the reversal agent is so unique. Spoiler alert, the antidote for heparin products is protamine sulfate. Why is it unique you ask? Believe it or not, protamine is a weak anticoagulant when given alone.
(Image)
Wait, to reverse heparin in an acute bleed, you give another anticoagulant (protamine)?
I know this sounds counterintuitive, BUT (big but). Yes, protamine does have weak anticoagulation effects when given alone. However, when it is given in the presence of heparin, it binds to the drug, forming a stable salt and therefore nullifying the anticoagulant activity of both drugs.
While protamine can fully reverse the effects of unfractionated heparin, it is very important to note that protamine incompletely reverses the anti-Xa activity of LMWH (enoxaparin). While you can get 100% reversal of unfractionated heparin with protamine, you can expect about 60-75% reversal of the anti-Xa activity of enoxaparin.
In terms of dosing, see below :)
Example time. Let’s say you’re consulted for patient AD (70 kg) who has evidence of upper GI bleed 2 days after starting an unfractionated heparin drip (1260 units/hr) for DVT treatment. Given the short half-life of unfractionated heparin, add the total units of heparin administered in the preceding 2 to 3 hours. To figure out the protamine dose for our patient, we can estimate 1260 units/hr x 3 hours = 3780 units administered in the last 3 hours.
As we stated above, every 1 mg of protamine neutralizes about ~100 units of heparin. So in this case, 3780 units/100 units = ~37.8 mg of protamine sulfate will be needed to reverse unfractionated heparin.
The same exact workup can be done with enoxaparin to help determine the protamine dose. I don’t want to beat a dead horse, but you get the picture.
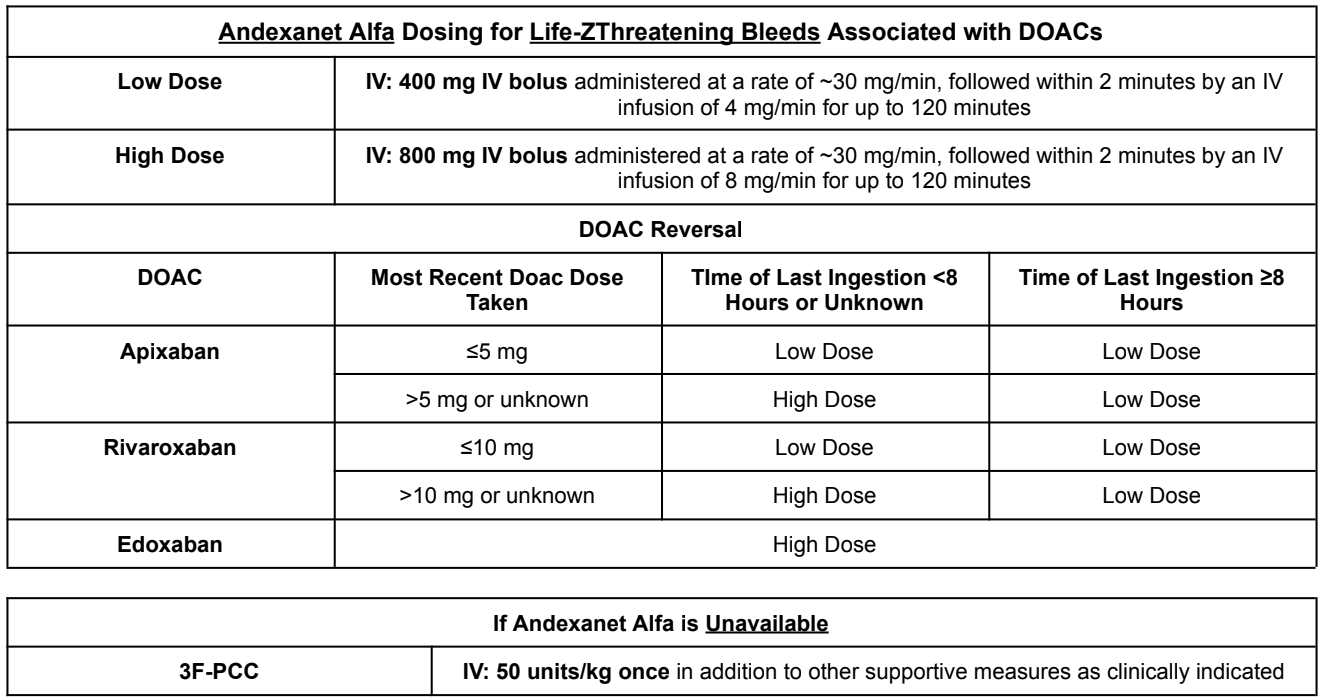
Direct Oral Anticoagulant (DOAC) Reversal
Considering DOACs continue to gain more and more popularity, the incidence of DOAC-associated bleeding has continued to increase over the past several years. Depending on which institution you work for, treatment of choice may differ between facilities.
I’m sure you’ve had drug reps come into your hospital with free dinners portraying the new DOAC reversal agent andexanet alfa as a life-saving drug. But is it really all they make it out to be? I’ll let you decide that for yourself because I may or may not have a very biased opinion. (If you haven’t read it, you should definitely get some pharmacy phriends together to journal club the ANNEXA-4 study.)
Nonetheless, andexanet alfa costs ~$3000 per 200 mg vial. As you can see below, andexanet alfa is generally dosed at 880-1760mg for DOAC reversal. So that means the true cost to treat DOAC-associated bleeding with andexanet alfa is closer to ~$13,200 to $26,400 per patient.
Is the cost justified by the scientific literature? Not really.
If you are at a smaller institution, you likely won't have andexanet alfa at your disposal. So what else can you administer for DOAC-associated bleeding?
Activated or inactivated 3F-PCC. Unlike 4F-PCC which is used for warfarin reversal, 3F-PCC contains only factors II, IX, and X (little to no factor VII). Considering DOACs inhibit factor Xa, we need a product that will replenish our diminished factor X, which will in turn help promote clotting thus reversing the acute bleed. For dosing of both agents, see below.
Dabigatran Reversal
What it’s like when idarucizumab sees dabigatran. Level of crush affinity = creeeeeeepy. (Image)
On to the last beast, which is also probably the least popular of the anticoagulants. I have yet to come across a dabigatran-associated bleed in my career, but I’m sure the time will come. The reversal agent for dabigatran is a fancy humanized monoclonal antibody fragment called idarucizumab.
Much like our other reversal agents, idarucizumab has an affinity for dabigatran that is ~350 times greater than that of thrombin. As a result, idarucizumab binds systemic dabigatran, neutralizing the anticoagulant effect within minutes of administration.
In terms of dosing…
Idarucizumab: 5 g IV (administered as 2 separate 2.5 g doses given no more than 15 minutes apart)
The tl;dr of Anticoagulation Reversal
In conclusion, one of the crucial steps in stabilizing an acute severe/life-threatening hemorrhage is reversing any possible lingering anticoagulant effects. Familiarizing yourself with the clotting cascade and knowing where anticoagulants work will help you understand how to reverse their effects.
If you skipped this entire post and went straight to the tl;dr version, here is a quick anticoagulant antidote/reversal agent summary you can use:
Warfarin
Antidote/Reversal Agent(s): Vitamin K +/- 4F-PCC
Clinical Considerations: always assess the severity of bleed and INR level before determining the dose and place in therapy of vitamin K and 4F-PCC
Unfractionated Heparin
Antidote/Reversal Agent: Protamine sulfate
Clinical Considerations: 1 mg of protamine neutralizes ~100 units of heparin
Low Molecular Weight Heparin
Antidote/Reversal Agent: Protamine sulfate
Clinical Considerations
1 mg of protamine neutralizes ~1 mg of low molecular weight heparin
Unlike unfractionated heparin, protamine does not fully reverse the effects of low molecular weight heparin. Protamine is expected to reverse about 60-75% of the anti-Xa activity of low molecular weight heparin.
Direct Oral Anticoagulants (DOACs)
Antidote/Reversal Agent(s): andexanet alfa or 3F-PCC
Clinical Considerations:
Andexanet alfa is very expensive and NOT readily available at a lot of facilities
3F-PCC can be dosed at 50 uunits/kg once for the reversal of DOAC-associated bleeds
Dabigatran
Antidote/Reversal Agent: Idarucizumab
Clinical Consideration: Idarucizumab is dosed at 5g (administered as 2 separate 2.5 g doses given no more than 15 minutes apart)
Stay tuned for part II of this severe bleeds series, in which we’ll tackle intracranial hemorrhages!