A Pharmacist’s Guide for Adult Gender-Affirming Care
Steph’s Note: This week, we’re tackling a topic that I’m betting most of you didn’t encounter in pharmacy school… and yet, these are medications that are frequently encountered on patients’ lists! While you may be decently familiar with the contraceptive utilities of hormone therapies (especially if you’ve perused this tl;dr post), it’s entirely possible you haven’t really studied too awfully much regarding therapies for transgender patients. Luckily, Dr. Megan Van Scoyoc is here to shed light on some lesser known - but increasing - uses for hormone therapies in order to help y’all be well-rounded practitioners.
Megan graduated from Texas A&M Irma Lerma Rangel School of Pharmacy in 2021 with her Doctor of Pharmacy. She is currently a Texas pharmacist assisting with genitourinary cancer clinical trials. Gender- affirming care is an avid interest of hers and she believes in the impact these practices make in patients’ lives.
The floor is all yours, Megan!
Congratulations! You have read two sentences. That is two sentences closer to educating yourself on impactful medications used by transgender people. I admire your dedication to learning about gender-affirming care. By educating ourselves on topics facing discrimination, we can become better health care professionals. Perhaps we can form a caring connection with others and pass on this information for their benefit.
Yes, I know those pharmacotherapy lectures were painfully long and chock full of info, but would a couple more slides for this topic really have made a huge difference for Hide the Pain Harold? (Image)
The text you read in this article takes shape in the lives around you. Did you learn about transgender health care while you were in school? Or perhaps it was a continuing education session?
I, for one, was not exposed to gender-affirming care in my formal education. Perhaps there should have been an extra slide in those long lecture notes?
Looking forward, let us expand our knowledge for the sake of others. This information is not intricate with mechanisms. Instead, it focuses on the principles for how we can attempt to assist transgender individuals.
Learn the Terminology Associated with Transgender Identities
Transgender or “trans” individuals are people who do not identify with the sex they were assigned at birth. To be clear, transgender women are people who were assigned male at birth but identify their gender as female, and transgender men were assigned female at birth but identify their gender as male.
The abbreviation for a transgender female is male-to-female (MTF), while transgender male translates to female-to-male (FTM).
Goals of Transgender Pharmacotherapy
In this article, I am solely focusing on medication therapy. However, this is just one piece of a large pie! Gender-affirming care incorporates many interdisciplinary aspects involving evaluation, diagnosis, mental health support, and surgical options. (I encourage you to read these 2017 Endocrine Society guidelines if you are interested in obtaining a broader view of gender-affirming care.)
Now, let’s get into the meat and potatoes of this article…medication therapy!
As you can imagine, medication therapy differs when someone is going from MTF versus FTM, but the major therapeutic themes are similar. Let’s think about what our goals are... First and foremost, we want our patients to feel aligned in their minds and bodies! So our priority is to induce physical changes that are congruent with gender identity.
Goals of care are individualized. For example, some individuals may aim to be nonbinary. But for simplicity’s sake in this post, I’m going to explain medication therapy as traditionally black and white (i.e., male and female) as possible.
Gender-Affirming Care for Adult Transgender Women
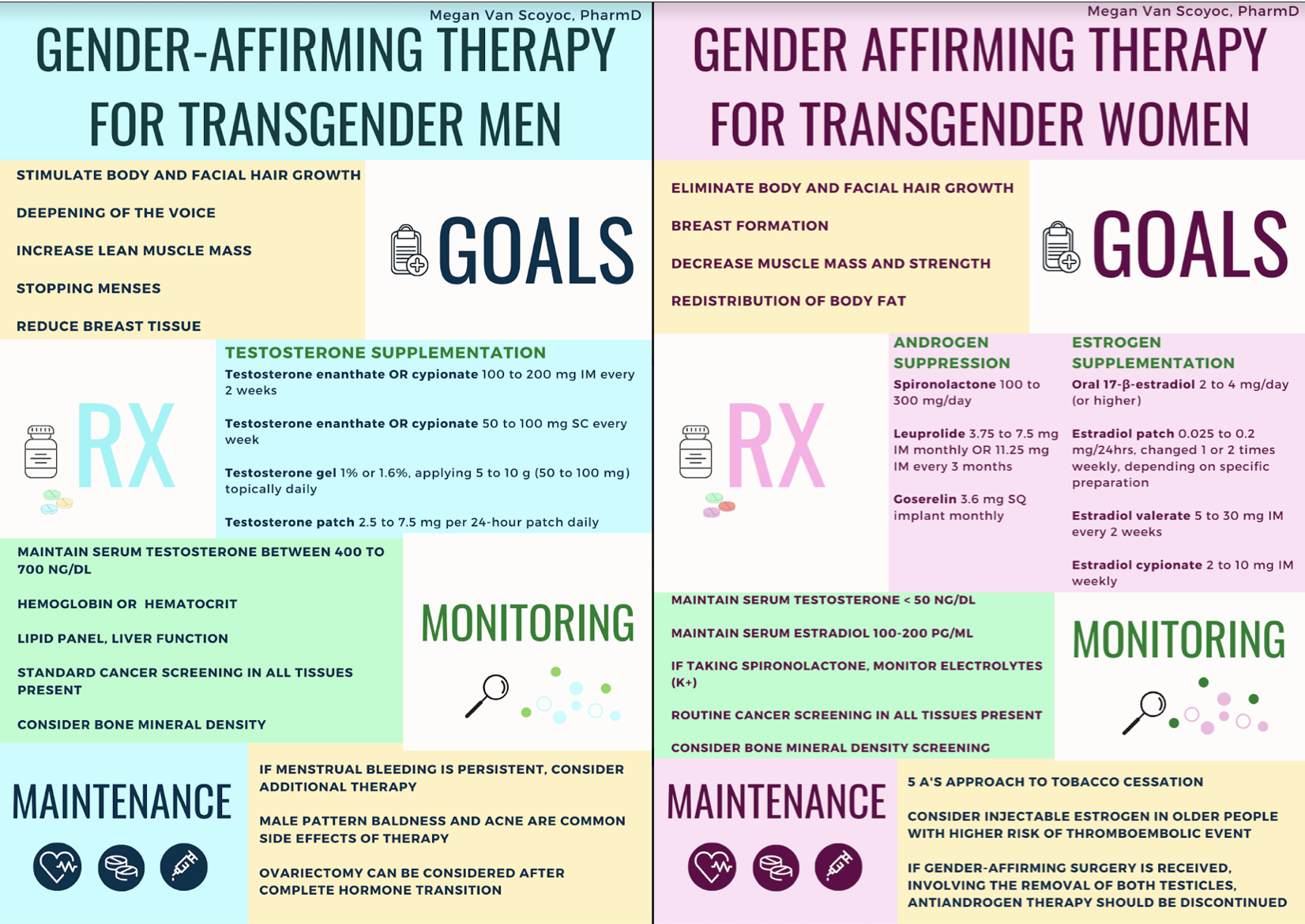
For transgender women (remember, this is MTF), goals of medication therapy include:
the elimination of facial hair growth,
the induction of breast formation,
a decrease of muscle mass, and
the redistribution of fatty tissue.
These changes commence in the first 3 to 6 months of therapy and reach their peak around 3 years, on average. To reach these goals, there are TWO parts of MTF medication therapy.
First, we want to suppress endogenous androgens.
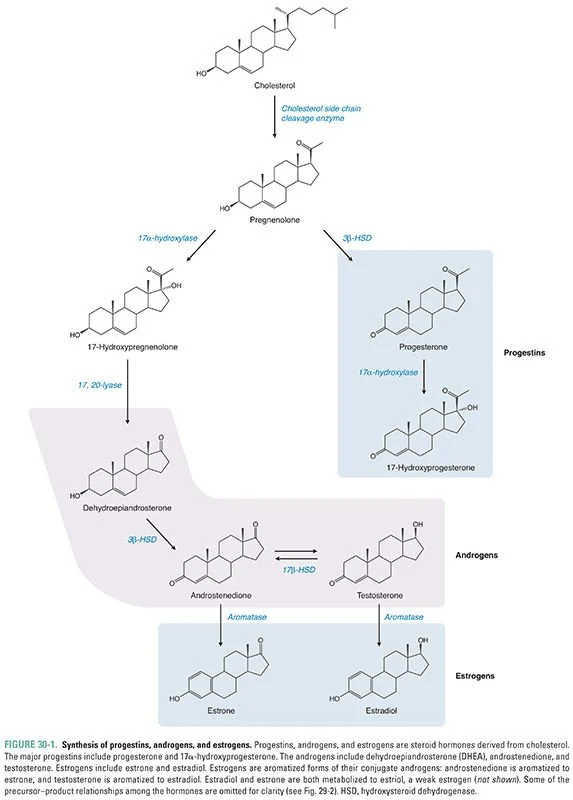
Yep, that’s right. Sex hormone production begins with cholesterol! (But no, this doesn’t mean go out and binge on Bojangles to up your testosterone.) Also note that the androgens include both testosterone AND estrogen precursors, so consider how antiandrogen therapy can impact hormone availability. (Image)
When you find out that spironolactone has yet ANOTHER therapeutic use. (Image)
Blocking androgen receptors or reducing androgen secretion is required so that we can meet our goals to decrease muscle mass and decrease hair growth. The primary medication used in the USA for blocking androgen receptors is spironolactone. (Indeed - the very same spironolactone that we use in congestive heart failure and cirrhosis! It’s a very multi-talented medication.) Cyproterone acetate (CPA) is another antiandrogen used, but it’s not available in the USA.
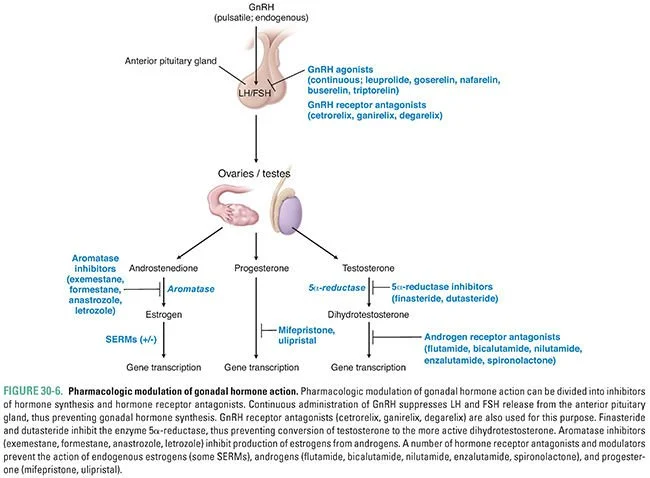
Both antiandrogen medications are effective and low cost, where available. Gonadotropin-releasing hormone (GnRH) agonists are equally safe and effective options, working by suppressing the secretion of androgens. Unlike the previous antiandrogens, however, these medications are expensive and require injections or implantation. Common GnRH agonists used include leuprolide and goserelin.
Let’s summarize some of these therapeutic options in context of the reproductive hormone pathway with the figure below:
In case you need a quick reminder of how GnRH, estrogen, and testosterone are inter-related - plus the medications that impact them. (Image)
Now, check out the chart below for a summary of the meds and doses used to suppress endogenous androgens:
Honorable mentions for medications used to suppress androgens go to 5-α-reductase inhibitors (finasteride and dutasteride) and medroxyprogesterone (MPA). Theories exist in favor of 5-α-reductase inhibitor efficacy in this patient population; nevertheless, there’s also data demonstrating no efficacy and increased adverse event risk. (Ouch, tough blow for this medication class. Might have to stick to benign prostatic hyperplasia (BPH)).
Meanwhile, MPA has proven efficacy as antiandrogen monotherapy, but cardiovascular and breast cancer risks limit its use. That being said, MPA is the recommended alternative when the first-line antiandrogens listed above (spironolactone, CPA, GnRH agonists) aren’t options.
The second part of MTF pharmacotherapy is supplementing estrogen.
Estrogen supports breast formation, and (just like breasts) estrogen formulations come in all shapes and sizes. Parenteral, oral, and transdermal, to be specific. The main concern with supplementing estrogen is considering individual thromboembolic risk. Patient-specific factors, such as smoking status, previous VTE, heart conditions, etc., are important when deciding on therapy. The risk of thrombosis according to estrogen formulation is as follows:
For safety, ethinyl estradiol is not recommended to be used in transgender women. The oral formulation of choice is 17-β-estradiol valerate. 17-β-estradiol valerate is a fancy way of specifying estradiol that is not synthetic or conjugated. Synthetic (ethinyl estradiol) and conjugated estrogens cannot have serum levels measured and, therefore, are not preferred in this setting. Regarding safety for injectable formulations, they have a prolonged onset and time to reach steady-state, leading to a risk of accumulation and overdose.
So what about progestins?
The use of progestins in therapy is controversial. Anecdotes report progestins supporting breast formation, but more studies are needed to confirm or disprove this theory.
Monitoring Adult Transgender Women
How do we monitor hormone therapy? Clinicians aim to establish and maintain a normal physiologic range of hormone levels aligned with the target gender. The occurrence of adverse events increases when hormone levels are elevated. For a transgender woman, monitoring of serum testosterone and serum estradiol is required. We use female premenopausal physiologic levels as references, resulting in a recommended serum testosterone less than 50 ng/dL and serum estradiol 100-200 pg/mL.
Consistent supplementation of estrogen helps to preserve bone density. Bone mineral density can be tested at baseline, conducted when 60 years old, or performed when non-adherence is an issue. If the patient is taking spironolactone, electrolytes should be monitored (especially potassium!).
Routine cancer screenings should be performed in all tissues present.
Special Considerations for Adult Transgender Women
Patients with intact testes will likely require higher doses of estrogen. If gender-affirming surgery is received, involving the removal of both testicles, antiandrogen therapy should be discontinued.
Vocal characteristics are also an important consideration. These feminizing medications (estrogen) cannot change voice pitch or resonance. Speech therapy or specialist assistance is recommended for individuals struggling with their vocal characteristics.
Gender-Affirming Care for Adult Transgender Men
For transgender men (FTM), goals of therapy include:
stopping menses,
stimulating the growth of body hair and facial hair,
deepening the voice,
increasing muscle mass, and
reducing breast tissue.
Now I’m not saying every patient can achieve the dulcet deep tones of Patrick Wharburton (Kronk!), but at least the medications can help some with vocal characteristics in the FTM case!
To achieve these goals, we use testosterone monotherapy. The onset of masculinization begins around 1 month and reaches maximum effect in 5 years. Deepening the voice is actually possible in this scenario because testosterone stimulates the Adam’s apple (laryngeal cartilage) to grow, whereas feminizing medications do not affect the voice.
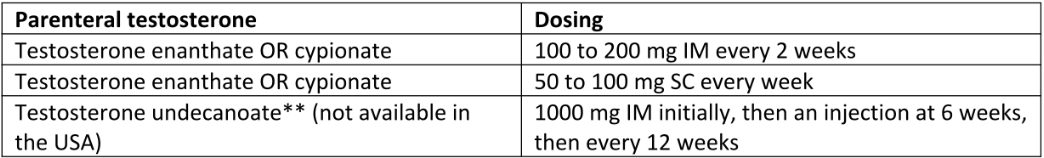
The recommended testosterone formulations are parenteral or transdermal preparations. Oral testosterone is not recommended due to the risk of liver toxicity. Injectable testosterone may be administered intramuscularly (IM) or subcutaneously (SC).
Btw, subcutaneous testosterone injection is not FDA approved, but data shows the administration is effective and well-tolerated. (And when I say well-tolerated, I mean the data also shows that, when presented with IM or SC options, 100% of individuals preferred SC testosterone. One hundred percent!! Don’t see that too often in studies.)
Some clinicians start at lower parenteral doses due to transgender men generally being smaller than cisgender men. (Cisgender refers to individuals assigned male at birth and who identify as male).
Dosing options for injectable testosterone are as follows:
Gel or patch formulations may also be used for testosterone monotherapy. Transdermal formulations will likely produce lower serum testosterone levels compared to injectables. Some clinicians may switch patients from injectable to a transdermal formulation after idealized physical changes are complete. Caution for patients using gel formulations is advised. Before the gel dries, inform patients that they must be careful to not have others touch the application area!
Dosing for transdermal formulations is as follows:
Monitoring Adult Transgender Men
Again, we monitor therapy by aligning serum hormone levels with the targeted gender’s normal physiologic profile. Monitoring of serum levels should be performed with consideration of testosterone formulation and administration timing. Check out this table for more details:
The most common adverse effects of testosterone therapy are an increase in red blood cells (erythrocytosis) and lipid profile changes (mostly decreasing HDL). Hematocrit and lipid levels should be monitored during physician follow-up, as well as weight and blood pressure. Routine cancer screenings should be performed in all tissues present.
Special Considerations for Adult Transgender Men
Some individuals may have persistent menstrual bleeding. To stop menses, there are both drug and surgical options that can be discussed. A modest increase in testosterone dosing, medroxyprogesterone (5 to 10 mg daily), or GnRH agonists may be considered, as well as endometrial ablation.
Even this Corgi knows… the hips don’t lie (Image)
Less desirable effects of testosterone supplementation include genetic expression of male-pattern baldness and the development of acne. Patients should be counseled on these potential effects. Similarly, patients should be aware that hormone therapy will not induce height changes nor will it change their broad hip configuration.
The tl;dr of Gender-Affirming Pharmacotherapy
As you can see, the medications used for gender-affirming therapy are common. Were you surprised?
In honor of pride month, perhaps you could send this article to your colleague to foster an inclusive environment. Perhaps, during the next coffee break, you could start chatting about how you just learned some unique uses for common drugs in the pharmacy, as well as aspects of being transgender that you never considered before. I dare you to go pass on your knowledge.
Thank you for stopping by to learn!