The Pharmacist’s Primer on Paralysis
Last Reviewed: August 25, 2025
Carley’s note: Hello again, my pharmacy phriends! I’m super excited today because we have Joe back covering another great critical care topic - paralysis. As a community pharmacist, I always envied my emergency and critical care counterparts for their ability to work in scary situations. Thankfully, Joe is great at making scary topics way less scary…take it away, Joe!
Let’s talk about the one topic that we all fear from both sides of the spectrum. Being paralyzed sounds frightening, but also administering paralytics sounds frightening. There’s really no winning here. It’s the topic we all would rather avoid. Until you’re called to the bedside to help with the preparation of a paralytic. All of a sudden, you start panicking and forget what a paralytic is, how they work, how to dose, contraindications, etc.
If I just described you, then please keep on reading :). We’re going to have an in-depth review of paralysis, paralytics, and reversal.
P.S. We previously had a small discussion on paralytics during our rapid sequence intubation post, which can be found here in case you need a refresher.
How Do Muscles Work? A Quick Anatomy Refresher
Close your eyes for a second. Think of the anatomy class you took in college. Personally, I am getting nightmares thinking about it as it was the hardest course I took in pharmacy school. Anyway, somewhere in your anatomy curriculum, you reviewed the different types of muscle tissue. Specifically, skeletal, smooth, and cardiac. Let’s review.
Skeletal Muscle
Location: attached to bones, enabling movement
Function: responsible for voluntary movements, posture, and generating heat
Control: voluntary
Smooth Muscle
Location: found in the walls of internal organs, blood vessels, and other internal structures
Function: controls involuntary movements like digestion, blood pressure regulation, and bladder control
Control: involuntary
Cardiac Muscle
Location: exclusively in the heart
Function: pumps blood throughout the body
Control: involuntary
You can’t tell your heart to beat, your blood vessels to constrict, or your GI tract to digest. That’s why smooth and cardiac muscles are involuntary. However, you can move your legs or your thumbs as you scroll through TikTok.
And that’s why our focus today is on skeletal muscle. We want to briefly inhibit your ability to voluntarily move to allow the medical professionals to do what they need to do (e.g., rapid sequence intubation).
The Nervous System’s Role in Muscle Movement
To better understand paralysis, we need to take a step back and review the basics of the human nervous system. The nervous system is composed of the central and peripheral nervous systems. The central nervous system is made up of your brain and spinal cord, while your peripheral nervous system is composed of the somatic (voluntary) and autonomic (involuntary) nervous systems. The autonomic nervous system is then further broken down into the sympathetic (“fight or flight”) and parasympathetic (“rest and digest”). The central and peripheral nervous systems are in constant communication with each other as they transmit messages from and to the brain.
I know. That was a lot of information, and you’re probably confused. Here’s a diagram to help visualize all of this.
(Image)
To put the pieces of the puzzle together, it’s important to recognize that skeletal muscles belong in the somatic nervous system, while the smooth and cardiac muscles belong in the autonomic nervous system.
Let’s start with a picture.
(Image)
Does that picture simplify it enough for you? In case your answer is no, let’s go over a simple real-life explanation to help make this even easier to understand.
Let’s say that I want to raise my arms. To do so, multiple steps need to happen
Step 1: My brain (aka me) creates the message that I want to raise my arms
Step 2: My brain sends that message through my spinal cord to reach the peripheral nervous system (central → peripheral nervous system communication)
Step 3: The message continues to transmit through the neurons in the peripheral nervous system
Step 4: Acetylcholine is released
Step 5: Acetylcholine binds to nicotinic receptors in the skeletal muscles of my arms
Step 6: I raise my arms
All of this happens within a fraction of a second. Now let’s play the other side. How do we inhibit my arms from moving? How do we paralyze a patient? You have two therapeutic options: non-depolarizing and depolarizing neuromuscular blockers.
Non-Depolarizing Neuromuscular Blockers
We’ll start with non-depolarizing neuromuscular blockers because they’re easier to understand. How this drug class works is actually fairly simple as long as you understand the somatic nervous system. Simply put, non-depolarizing neuromuscular blockers bind to the nicotinic receptors in the skeletal muscle and inhibit the binding of acetylcholine. This in turn prevents the body from moving voluntarily. For you visual learners, take a look below.
(Image)
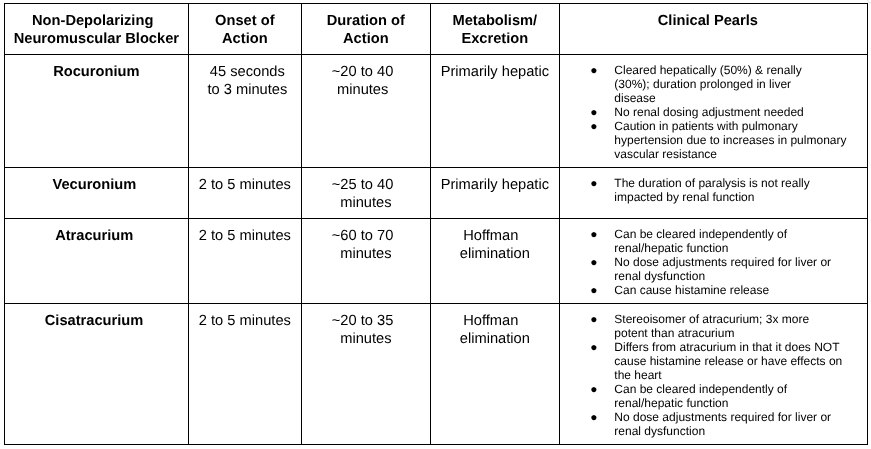
Now that we understand how this class works, let's talk about drugs. There are four non-depolarizing neuromuscular blockers available in the U.S..
There’s a lot of information in that table. So I wanted to discuss the really important parts that we should remember. But before we do that, I want to stress the importance of ensuring appropriate sedation BEFORE paralyzing a patient. The last thing you want to do is paralyze a patient who is fully awake and cognitive. I mean, imagine the nightmare that would be. Sitting there wide awake but unable to move. Sounds horrible. So yes, please don’t forget to always ensure the patient is appropriately sedated before administering paralytics.
Also, being sedated and paralyzed doesn’t necessarily mean that you can’t feel pain. Pain reception is a completely different pathway in the brain. Being sedated might make you feel better, but it’s not going to numb the pain completely. So in select patients, sedation and analgesia are generally recommended prior to paralysis. Long story short, we pretty much want to completely knock you out and help you not feel a thing because being paralyzed is the scariest thing in the world.
Oh, and one more thing. In patients with Class 1, 2, or 3 obesity (BMI ≥30 kg/m2), use the ideal body weight for weight-based dosing calculations.
Okay, now back to what we're talking about. Here are bullet points of all the important information that we should remember regarding non-depolarizing neuromuscular blockers.
Rocuronium:
Generally, the fastest on and the fastest off. This pharmacokinetic profile makes rocuronium a very attractive option for rapid sequence intubation
Primarily cleared by the liver. Older patients with hepatic dysfunction may experience prolonged effects of rocuronium
Vecuronium:
More potent than rocuronium
Duration of paralysis is not really impacted by renal function unless anephric (30% is eliminated in urine)
Younger children may require initial higher doses and more frequent supplementation
Atracurium:
Undergoes Hoffmann elimination, which occurs in the plasma and tissues of the body. This makes atracurium a very attractive option when prolonged/continuous paralytic use is needed, as it is cleared independently of renal and hepatic function
Given the Hofmann elimination, atracurium is generally used for the treatment of acute respiratory distress syndrome (ARDS) in mechanically ventilated patients in the ICU
No dosage adjustments required for altered kidney or liver function
Cisatracurium:
A stereoisomer of atracurium. In case you forgot what a stereoisomer is. Stereoisomers are molecules that have the same molecular formula and sequence of bonded atoms, but differ in the three-dimensional orientation of their atoms in space
Cisatracurium’s isomer is known for its higher potency and reduced propensity to release histamine compared to atracurium
Undergoes Hoffman elimination and therefore does not require dosage adjustments for altered kidney or liver function ○ Generally used for the treatment of acute respiratory distress syndrome (ARDS) in mechanically ventilated patients in the ICU
Depolarizing Neuromuscular Blockers
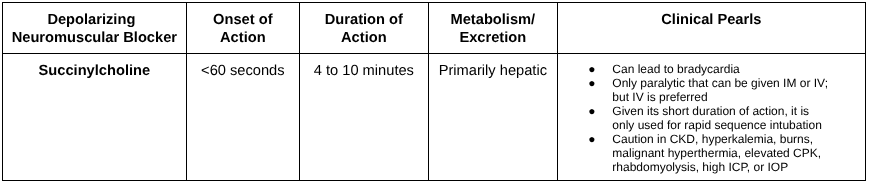
There’s really just one depolarizing neuromuscular blocker approved in the U.S. That drug is called succinylcholine. The mechanism of action for succinylcholine is slightly more complicated than the non-depolarizing agents that we discussed earlier. But bare with me, I am going to try and explain as simply as possible.
Succinylcholine is actually an analogue of acetylcholine. In fact, succinylcholine consists of two acetylcholine molecules linked together. So yes, it literally mimics acetylcholine at the neuromuscular junction. I bet you’re confused. Earlier, we said that acetylcholine binds to nicotinic receptors in the skeletal muscle, leading to voluntary muscle movement. So if succinylcholine mimics acetylcholine, won’t that just cause us to move even more?
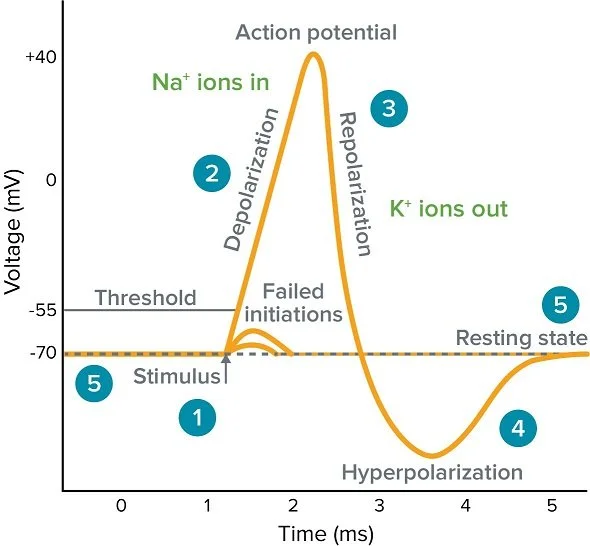
Yes and no lol. Remember action potentials? They looked like this:
(Image)
Each action potential is composed of 4 steps: depolarization, repolarization, hyperpolarization, and resting state. In skeletal muscle, an action potential triggers a series of events leading to muscle contraction. Specifically, muscle contraction occurs during the depolarization phase, and muscle relaxation occurs during the repolarization phase of an action potential. For us to move freely, all the steps of the action potential need to occur. Blocking one of these steps inhibits the action potential and prevents us from moving freely, leading to paralysis.
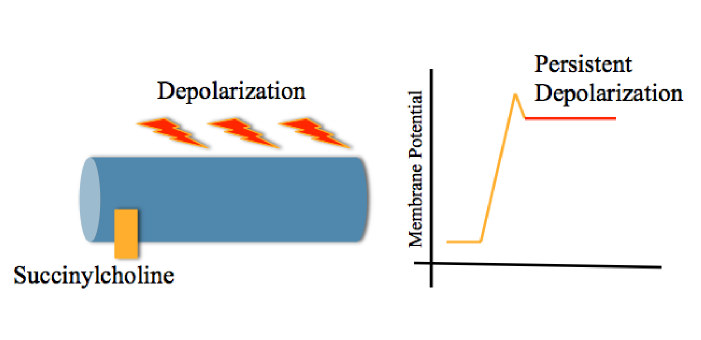
As the name clearly suggests, succinylcholine is a depolarizing neuromuscular blocker. Therefore, it works by producing depolarization of the motor endplate at the myoneural junction, which causes sustained flaccid skeletal muscle paralysis. Unlike the normal action potential, when succinylcholine is given, that same action potential looks a little something like this:
(Image)
As you can see, repolarization and hyperpolarization never occur, and the action potential never reaches that resting state as long as succinylcholine remains in the body. This prevents skeletal muscle relaxation and leads to paralysis.
Regarding the pharmacokinetic profile of succinylcholine, take a look below:
As you can see, succinylcholine is MUCH faster on and off than all of the non-depolarizing paralytics. This makes it a great option for rapid sequence intubation, as paralysis >10 minutes is rarely ever needed for RSI.
That being said, succinylcholine does have a big list of contraindications and adverse effects. One of the biggest downsides of succinylcholine is its notorious ability to cause hyperkalemia. In fact, a single dose of succinylcholine is estimated to increase serum potassium by up to 0.5 mEq/L. Additionally, succinylcholine has been shown to induce malignant hyperthermia in patients predisposed to this condition.
Given these risks, succinylcholine is generally contraindicated in patients with a history of:
Malignant hyperthermia (personal or family)
Neuromuscular disease involving denervation
Muscular dystrophy
Stroke over 72 hours old
Rhabdomyolysis
Burn over 72 hours
Significant hyperkalemia
Additionally, given it’s an analogue of acetylcholine, succinylcholine can lead to bradycardia, increased intraocular pressure, hyperkalemia, trismus, and fasciculations.
It sounds like succinylcholine is just filled with bad news. Does that mean we should never use it? Not at all. While it may carry more contraindications and side effects than non-depolarizing paralytics, its much shorter duration of action and quicker onset make it a more attractive option when patients don’t have any of the above contraindications.
Oh, and one last thing. Up in the non-depolarizing neuromuscular blocker section, we talked about using the ideal body weight for weight-based dosing in patients with a Class 1,2, or 3 obesity (BMI ≥30 kg/m2). Unlike the non-depolarizing neuromuscular blockers, succinylcholine should be dosed using the actual body weight. However, patients with extreme obesity (e.g., BMI >60 kg/m2), consider using adjusted body weight for weight-based dosing calculations.
How to Reverse Paralytics?
Let’s get straight to it. There is NO reversal agent for depolarizing neuromuscular blockers (succinylcholine). That is one of the negatives of this agent. However, given its short duration of action, paralysis generally lasts no more than 10 minutes.
Again, there is NO reversal agent for succinylcholine. So if you give the drug, you’re stuck with it until it wears off. There’s no emergent reversal.
However, there are a couple of reversal options for your non-depolarizing neuromuscular blockers. And truthfully, reversal of these agents is more important given their longer duration of action (~30-60 minutes). Anyway, you have two main options: an acetylcholinesterase inhibitor or sugammadex.
Let’s start with the acetylcholinesterase inhibitor. Most commonly, neostigmine. Neostigmine works by inhibiting the destruction of acetylcholine by acetylcholinesterase. The thought process here is that if we inhibit the breakdown of acetylcholine, we can lead to increased acetylcholine concentrations in the myoneural junction, leading to some binding to the nicotinic receptors and reversing paralysis. That being said, it’s not the most efficacious and generally is only effective in reversing light to minimal neuromuscular blockade.
On the other hand, we have a newer drug called sugammadex. Sugammadex is a selective relaxant binding agent that forms a complex with rocuronium or vecuronium in the plasma, reducing the amount of neuromuscular-blocking agent available to bind to nicotinic receptors in the neuromuscular junction. This results in the reversal of neuromuscular blockade induced by rocuronium or vecuronium. That being said, sugammadex has NO affinity for other non-depolarizing neuromuscular blockers and therefore cannot reverse atracurium or cisatracurium. In that case, neostigmine would need to be used.
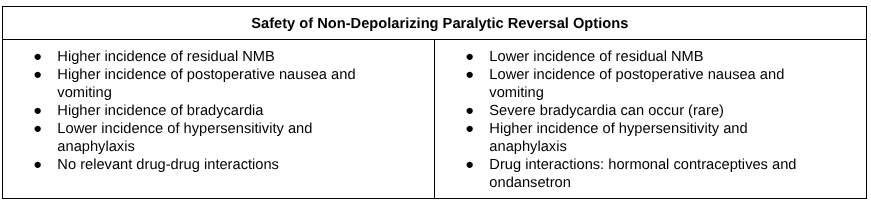
Here is a table that I made for you to help better summarize the efficacy and safety profiles of our non-depolarizing paralytic reversal options:
Well folks, that’s all she wrote. I know this was a complex topic, but I hope you are now an absolute paralysis guru.
The Tl;dr of Paralysis
Basics of Muscle & Nervous System:
Skeletal muscle = voluntary movement → target of neuromuscular blockers
Controlled via the somatic nervous system
Pathophysiology:
Brain sends signal → spinal cord → peripheral nerves
Acetylcholine release, which binds to nicotinic receptors on the skeletal muscle, leading to muscular contraction and movement
Neuromuscular Blocking Agents (NMBAs)
Non-depolarizing: antagonize acetylcholine receptors → prevents skeletal muscle contractions
Rocuronium:
Fastest onset of action with a short duration of action compared to other non-depolarizing NMBAs
Great for RSI
Hepatically cleared
Vecuronium
Longer onset of action than rocuronium with a similar duration of action
Hepatically cleared
Atracurium
Undergoes Hoffman elimination and is safe to use in patients with hepatic and/or renal dysfunction
Can cause histamine release
Ciastracurium
Undergoes Hoffman elimination and is safe to use in patients with hepatic and/or renal dysfunction
Is NOT known to cause histamine release
Generally, the ICU favorite for continuous paralysis
Depolarizing: mimics acetylcholine → overstimulation of nicotinic receptors → muscle stays depolarized → paralysis
Succinylcholine
Very quick onset of action (<60 seconds) and duration of action (4-10 minutes)
Pharmacokinetic profile makes it attractive for RSI
Use is contraindicated in patients with:
Hyperkalemia, burns >72 hours, rhabdomyolysis, malignant hyperthermia, muscular dystrophy, stroke >72 hours, and denervation injuries
Side Effect:
Increase in potassium (up to 0.5 mEq/L per dose)
Bradycardia
Fasciculation
Increase ICP & OP
Malignant hyperthermia
Always ensure appropriate sedation and analgesia BEFORE paralysis
Always ensure appropriate post-intubation sedation and analgesia
Paralytic Reversal Agents
No reversal agent for depolarizing NMBAs (succinylcholine)
Neostigmine
Can be used to reverse all non-depolarizing neuromuscular blockers
Less effective in deep blockade
Generally require an anticholinergic to reverse the side effects (e.g., bradycardia)
Sugammadex
Can ONLY be used to reverse rocuronium and vecuronium
Provides rapid reversal
Co-administration of anticholinergic agents is generally not necessary
May interact with hormonal contraceptives and Zofran