The Pharmacist's Guide to U-500 Insulin
Editor's Note: Laurie Elmes, PharmD, CDE, BC-ADM is a clinical pharmacist at Dell Seton Medical Center at the University of Texas. She has specialized in diabetes education and management for more than 25 years in both inpatient and outpatient settings. Her passion is patient education and insulin pump training/management.
Put another way, Laurie knows a lot about the pharmacist's role in diabetes care and education. And I'm super excited (and thankful) to have her share some of that with you. You're going to learn a lot from this post. Enjoy!
Would you like to print this article? Or save it for offline viewing? You can get it as an attractive and printer-friendly PDF right here.
PS. We've got a diabetes cheat sheet that will make NAPLEX questions a breeze and function as a handy addition to your peripheral brain on rounds. Check out the bottom of this post for more info!
Concentrated insulin? Chances are you may have never heard of or seen Humulin R U-500 insulin—or if you have, you didn’t quite know all the intricacies around it. Today I will dispel the mystery behind concentrated insulin and help you avoid errors when it comes across your computer screen (or on your NAPLEX).
What is U-500 Insulin?
Because of the propensity for error, Humulin R U-500 insulin is a frequent ‘star’ in ISMP’s publications (Institute for Safe Medication Practices).
Family photograph of U-500 insulin (yellow) and U-100 (green) (Image)
So….what is this dinosaur and why do we need it for managing diabetes??
Humulin R U-500 is a concentrated Regular insulin used as a basal insulin. So instead of the typical U-100 insulin (100 units/ml), U-500 insulin is 500 units/ml—5x as concentrated.
In contrast, Humulin R U-100 insulin is a short-acting, prandial insulin.
Can’t you already see the potential for mix-ups?!
They're both regular insulins, but U-500 is used for basal coverage while U-100 is used for prandial coverage.
Oh, and remember, it's 5x the concentration.
Our use of concentrated insulin has increased over the past 10 years due to the
increasing incidence of insulin resistance and obesity. The obesity rate in 2015 was 30%! On top of this, the diabetes rate in 2015 was 9.4% (30.3 million people) and another 84 million have pre-diabetes.
Insulin resistance is the hallmark characteristic for Type-2 Diabetes. As these patients get older, their insulin resistance worsens, resulting in ever-increasing insulin needs.
At a certain point, it’s just impractical to continue with U-100 insulin. The number of daily injections required can become too cumbersome (a compliance nightmare), and you start to see diminishing returns with U-100.
This begs the question...
When should you use U-500 insulin?
When a patient requires more than 200 units of insulin a day, changing to U-500 can improve blood glucose control and provide more comfort with fewer injections. I'll cover how to actually transition your patient to U-500 later in this post.
U-500 Insulin Dosing Considerations
Understanding how your pancreas works will help you understand how to use injectable insulin safely and effectively. So let’s review.
The pancreas has both exocrine and endocrine functions. The exocrine functions basically help you digest food. This is the amylase and lipase you've heard about. These enzymes get secreted whenever you eat, and they help us break down dietary proteins and fats into something usable for the body.
The endocrine functions include two main pancreatic hormones:
Insulin (lowers blood glucose)
Glucagon (raises blood glucose)
Two terms you will see regarding insulin management are basal and prandial. Basal refers to background insulin and prandial refers to mealtime insulin.
Basal - background insulin
Prandial - mealtime insulin
For people without diabetes, about 50% of total daily insulin is secreted during the basal periods (about 0.5-1 unit/hr). This manages blood sugar in between meals and overnight.
The remainder of insulin secretion is post-prandial. Post-prandial insulin controls blood sugar after meals. As an example, when you eat that donut you’ve been eyeing at the nurses station, your pancreas starts pumping out insulin within about 2 minutes (and continues for another 10 - 15 min). This is called prandial insulin secretion and it balances the rise in blood glucose from food.
As Type-2 Diabetes progresses, your patient’s pancreas gradually loses its ability to meet their insulin needs. Luckily, we can use the commercial insulins we have available on the market to mimic this basal/prandial pattern.
Humulin R U-100 is a prandial insulin
Humulin R U-500 is a basal insulin
Here’s example to illustrate why you might consider using U-500:
Your patient is currently using 400 units of basal insulin daily. Examples of basal insulin are insulin glargine [Lantus] and insulin detemir [Levemir]. Both Lantus and Levemir are U-100 (100 units/ml). U-100 Insulin syringes are available in a few different sizes:
30 units
50 units
100 units
In order for this patient to take 400 units of basal insulin, he will need to take 4 separate injections using the largest syringe (the 100 unit one). Not to mention that he is probably also using a rapid acting insulin analog at meal time, increasing the injection burden to 7 shots per day!
Ouch...
U-500 can really be a lifesaver for this patient.
U-500 Insulin Pharmacokinetics
Another consideration with large doses of insulin is absorption. Many factors influence insulin absorption after SQ injection:
Site of injection
Dose of insulin
Depth of injection
Thickness of the SQ fat layer
Exercise at the site
Temperature
Depth of injection
Volume is a key factor in absorption due to surface area and diffusion. Higher doses (and larger volumes) usually prolong insulin action because of residual levels at the site of injection. This makes intuitive sense if you think about it (a large ice cube takes much longer to melt than a small one). At the same time, it is also more painful to inject larger volumes. Remember that there is a limit to the volume you can inject subcutaneously (generally recognized as around 1.5 ml). The closer you are to that number, the more painful the injection.
And here’s the thing — as insulin injections become more painful and frequent, patient compliance tends to go down.
Our patient example above is a perfect patient to consider using concentrated Humulin R U-500 insulin. U-500 insulin is FIVE times as concentrated as U-100 insulin. A smaller volume injected under the skin means better absorption and potentially better blood glucose control. Since this patient is measuring 4 ml (400 units) of U-100 insulin per day he would need to measure only 0.8 ml (400 units) Humulin R U-500 insulin (because basic math tells us that 400 units divided by 500 units/ml = 0.8 ml). Big difference in volume of insulin while maintaining the same dose of insulin.
Does Humulin R U-500 have a different pharmacokinetic profile or does it work just like Humulin R (short acting) insulin?
Great question! As noted above, the high concentration of U-500 insulin makes the pharmacokinetic profile look very different from regular U-100 insulin. U-500 insulin has both prandial and basal characteristics. The onset of action is about the same for Humulin R U-100 and U-500 (about 15 - 30 minutes). The peak for regular U-100 insulin is 2.5 - 5 hrs compared to the peak for U-500 insulin at 4 - 8 hrs. The duration of action is also different, with regular U-100 insulin duration being 4 - 12 hrs compared to U-500 insulin duration 13 - 24 hrs. Let’s summarize with a handy table:
| U-100 vs. U-500 | |||
|---|---|---|---|
Insulin | Onset | Peak | Duration |
| U100 | 15 - 30 min | 2.5 - 5 hrs | 4 - 12 hrs |
| U-500 | 15 - 30 min | 4 - 8 hrs | 13 - 24 hrs |
So in effect, changing the concentration of this short acting insulin makes it more like an intermediate to long acting insulin. Thus, in practice, Humulin R U-500 insulin is used as a basal insulin instead of a mealtime insulin.
How to Convert from U-100 Insulin to U-500 Insulin
When patients are transitioning from U-100 basal insulin to Humulin R U-500, it’s usually best to initially decrease the dose 10-20%.
This is similar to when you convert opioids and you reduce the dose for cross-tolerance. It's easier to add some extra insulin to get blood sugar to goal than it is to deal with hypoglycemia. It's better to under dose than to overdose during the transition. You also need to change the frequency of injection.
U-100 basal insulin (e.g. Lantus and Levemir) is dosed once a day – sometimes twice a day
Humulin R U-500 is dosed BID to QID for basal coverage
Let’s go back to the example above in which the patient was using 400 units of U-100 basal insulin daily. When he converts to Humulin R U-500, he would measure 0.8 ml on a TB syringe (or measure to the 80 units mark on a U-100 syringe) (x 5 = 400 units) on a U-100 syringe.
Seems easy enough, right? Now that you have an idea about the differences between U-100 and U-500 and how you would convert doses, you might be thinking...
““Where are all these dosing errors coming from?””
The source of almost all U-500 Insulin dosing errors (Image)
What's the big deal, right? It's easy enough to convert the doses, it's just basic math.
It all boils down to insulin delivery devices. Namely, the SYRINGES!
Prior to 2017, U-100 insulin syringes were the only type of insulin syringes on the market (back in 1994, the specific U-500 insulin syringes were discontinued by the manufacturer). As I mentioned above, the only option for measuring the concentrated U-500 insulin was to use U-100 syringes (or in some cases, TB syringes...the same ones that are used when you get a PPD).
Because important points are worth re-emphasizing, let's cover our U-500 insulin conversion factor again.
Let’s say you need to measure 400 units of Humulin R U-500 insulin. The volume of this U-500 insulin dose would be 0.8 ml using a TB syringe or you could use a U-100 insulin syringe to measure to the “80 unit” marking.
What? I’m measuring 80 units? But the dose is 400 units? That’s right folks, there’s math involved. And that’s where the waters get muddy.
Patients and providers are required to divide the actual dose (units) by 5 in order to know how many units to measure (80 units) on the U-100 syringe. If the patient is using a TB syringe, you would divide the dose (in units) by 500 to calculate the volume that would be measured (0.8 ml) on the TB syringe.
You can probably see the dilemma...
Providers are telling patients that they are taking 80 units (because that’s what they're measuring) but the actual dose is 400 units. PLUS if the patient gets admitted to the hospital, the RN takes the admission history and documents that the patient told her she is taking 80 units of Humulin R U-500. This is where an astute hospital pharmacist would look at that dose and question why the patient is using concentrated insulin for an 80 unit dose. (Remember, Humulin R U-500 is only appropriate for patients who need more than 200 units of insulin/day).
This is actually a nice place to talk about practical ways to use Humulin R U-500 safely.
How to Use U-500 Insulin Safely
There are 2 main sources of U-500 errors in the hospital setting.
Documentation errors (i.e. recording the wrong dose/strength on the admit med reconciliation)
Dosing/Administration errors (i.e. administering the wrong dose of U-500 because of confusion with the using TB or U-100 syringes)
Both of these errors are multidisciplinary in nature.
Pharmacists have dispensed the wrong dose of U-500 because of syringe confusion and likewise nurses have used a U-500 vial to draw up the wrong dose. All health disciplines have recorded the wrong home dose while taking the patient's med reconciliation.
The key to hospital safety with using Humulin R U-500 centers around multiple things:
Correct admission medication reconciliation (check out this post for tips on how to do a thorough med rec)
Provider and nursing staff education
Verification of all orders and order changes by a pharmacist
Appropriate administration devices
Standardized orders (a custom set of U-500 orders with appropriate instructions)
Communication to the next level of care (i.e. clearly communicating U-500 use to the rehab center your patient is going to at discharge)
Appropriate administration devices? Isn't that part of the problem? We only have U-100 and TB syringes, right? Wrong. This brings us to the new kids on the block. Two new products became available recently to improve safety with Humulin R U-500 insulin.
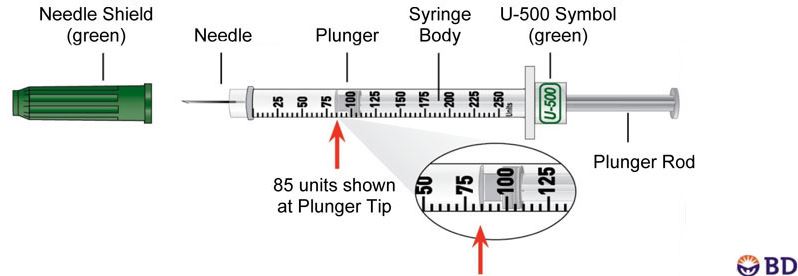
The first one is a U-500 syringe that is available by prescription only. It has a green cap (compared to the distinct orange cap with U-100 syringes) and can measure up to 250 units in 5 unit increments.
Look at this handsome little guy protecting the world from insulin dosing errors. Not all heroes wear capes. (Image)
The second product is a Humulin R U-500 Kwik pen. This insulin pen can measure up to 300 units per dose in 5 unit increments. Each pen holds 1500 units and has a distinct aqua color cap to distinguish it from other insulin.
Just like most other insulins, the U-500 Kwik pen is stable for 28 days unrefrigerated once opened (Image)
The Humulin R U-500 vial is also distinctly colored with brown/white stripes or aqua/white stripes. It’s a fatter 20 ml vial compared to U-100 insulin vials.
Yes, I just called the U-500 vial "fat." (Image)
One 20 ml vial of Humulin R U-500 is approximately $1500 (10,000 units/vial). One box of two 3 ml Kwik pens (3000units/box) is approximately $600.
This is what a safety needle looks like. See how it can re-cap itself without the user risking a needle stick? (Image)
Unfortunately, the U-500 insulin syringe is not available with a safety needle so some hospitals have chosen not to stock this product. Safety syringes protect the health care professional from potential needle sticks (and the associated blood-borne pathogens) because there is no re-capping involved.
If you're transitioning outpatients from U-100 syringes to U-500 syringes, it's critical to review the differences to avoid dose confusion. ISMP has reported errors with patients who had both U-100 and U-500 syringes in their home and confused the two.
Patients need education and practice to ensure that they understand accurate measuring, dosing, and administration with the new syringe markings. Also, if possible, efforts should be made to remove all U-100 syringes and supplies from the house if converting to U-500 syringes.
Additional U-500 Resources
Your local certified diabetes educator (CDE) is an excellent resource to recommend for your patients. CDE’s are healthcare professionals who have comprehensive knowledge and experience in diabetes prevention, pre-diabetes, and diabetes management.
CDE’s promote self-management to achieve individualized behavioral and treatment goals that reduce risks and optimize health outcomes.
You can find your local CDE’s at www.diabeteseducator.org.
Diabetes Cheat Sheet
Our Diabetes Cheat Sheet is 7 sweet pages of distilled diabetes information. It makes studying for the NAPLEX (or going on rounds) a breeze. It’s by far our most popular clinical cheat sheet. We've designed this thing so it's just as useful for a student as it is for a practitioner. Here's some of what's included:
A comprehensive chart of every available insulin - Including PK, dosing, how to store it, available dosage forms, and more
A chart of all oral combo drugs - So you can learn that brand/generic
Renal and hepatic dose adjustments for all drugs - Obviously
Clinical/monitoring pearls for all drugs - Also obviously
A quick algorithm for diagnosing diabetes
A1c goals (for both ADA and AACE) and basic treatment considerations
How to spot the difference between DKA and HHS - It could save a life (or a test grade)
How to treat hypoglycemia
Common drug interactions - You think we'd make a cheat sheet without including this?
A metric-crap-ton of other stuff - *Not an actual unit of measurement
Use this cheat sheet for an endocrine module, an ambulatory care rotation, or just to shake the cobwebs off the part of your brain where diabetes info lives. Have an exam coming up? Not sure if you need to renally adjust empagliflozin for the new admit on your floor? This cheat sheet is for you.