Pharmacology 101: An Overview of Thiazide Diuretics
Steph’s Note: Today we are pumped to introduce a new tl;dr author, Malashia Drummond. She’s a P4 at the University of South Carolina College of Pharmacy. She served as a Rho Chi tutor for pathophysiology during the 2019-2020 school year, so she definitely loves teaching and breaking things down for greater understanding. She’s not 100% certain of her future career field, but she knows she wants to provide care to underserved populations. In her free time, she loves eating sweet things and watching movies.
BTW - We compiled ALL of our Pharmacology 101 posts into one handy, downloadable (and printer-friendly) PDF. You can get your copy of it here.
Teach us, Malashia!
First things first…Corny joke time:
(Image)
Why did the doctor prescribe HCTZ to the bucket?
Because he was retaining water! (ba-dum tsss). Don’t worry folks, I’ll be here all night.
Okay back to business.
What are diuretics?
If you answered with “ a water pill,” you’d be correct. If you answered with “the workhorse behind flat tummy teas,” you’d also be correct. Diuretics are medications that promote urination through various mechanisms.
How Do Diuretics Work?
Let’s start with the kidney. In order to understand the mechanism of diuretics and their place in therapy, you must first understand the way of the kidney (+10 points if you get the Bruce Lee reference).
(Image)
If the kidneys are your least favorite organ, I recommend starting with tl;dr’s Kidney Bean series. It's a great review of all things pharmacy-related to the kidneys. But for now, I’ll give you an anatomy overview because I’m nice.
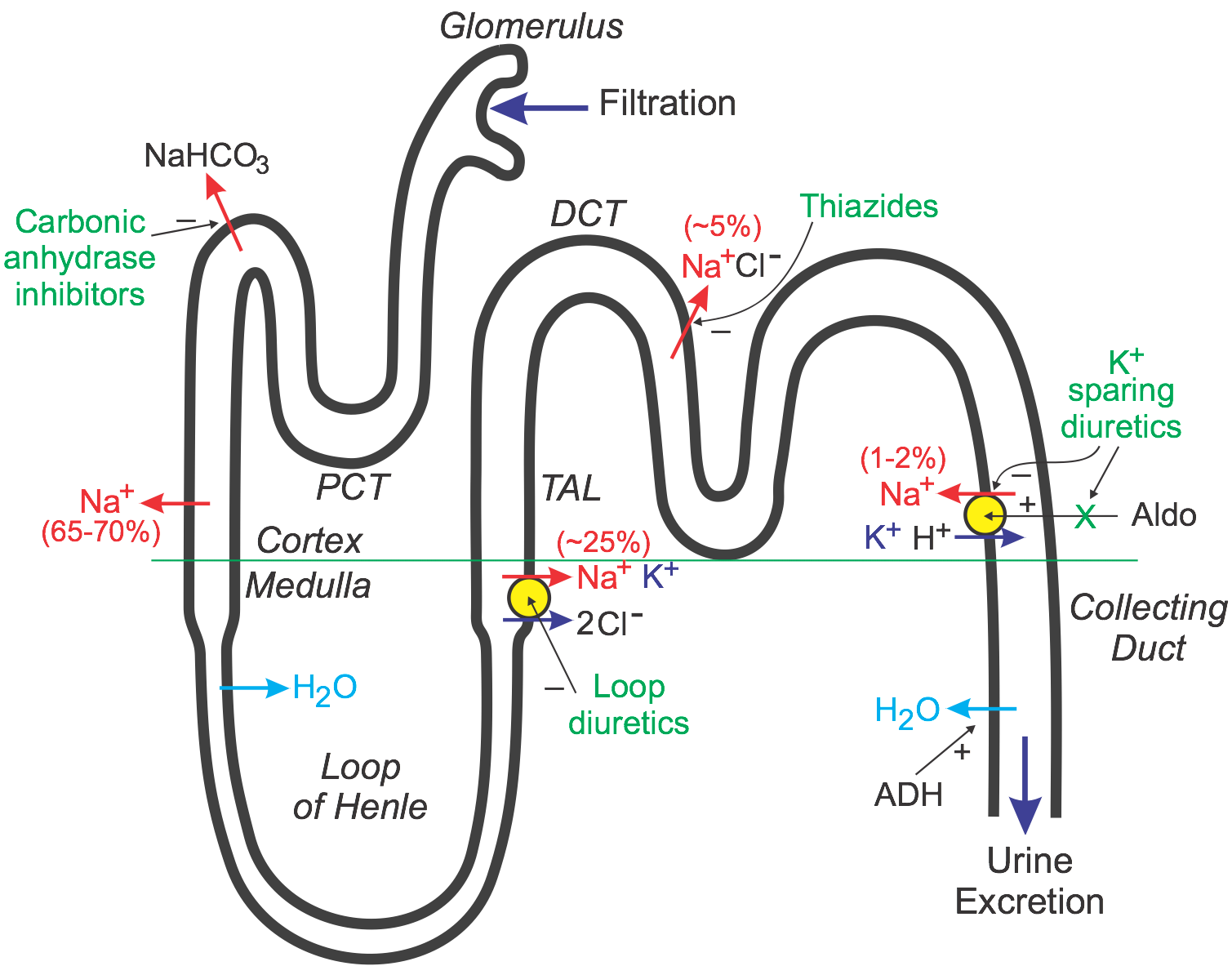
I envision the nephron as a neighborhood. First, we enter through the glomerulus. Think of this as the security gate. It determines what comes in and in what capacity. Next is the proximal convoluted tubule (PCT). The carbonic anhydrase medication family resides here, and it is a site of sodium reabsorption.
Driving a little further down the road, we arrive at the Loop of Henle where water is reabsorbed. After the Loop of Henle comes the thick ascending limb (TAL), which is the site of sodium, potassium, and chloride reabsorption. The Loop diuretic medication family lives at the intersection between the Loop of Henle and the TAL.
The TAL leads into the distal convoluted tubule (DCT). The DCT is home to our guests of honor, the thiazide family!
To exit kidneyville, you have to drive through the collecting duct, the final site of water reabsorption. The town’s misfit, antidiuretic hormone (ADH), lives here. We won’t discuss him very much in this post, but just know that he’s not entirely evil, just misunderstood. (Just like Shrek and onions, ADH has layers.)
The town of Kidneyville in all its glory, along with the diuretic families and where they live and work. (Image)
Now that we have the anatomy down... The next important concept to understand when thinking of diuretics is sodium/water balance. Diuresis occurs through the manipulation of sodium transportation. Remember the phrase “water follows salt”? Well, in order to release water, your body has to waste sodium.
The kidney contains 2 main types of membrane transport proteins: uniporters, which move ions down their concentration gradients; and cotransporters, which pair the transportation of one ion down its concentration gradient with the transportation of another ion against its concentration gradient. Cotransporters can be symporters (ions move in the same direction) or antiporters (ions move in opposite directions).
You may be saying, “Malashia, get to the point. How do the thiazides work?”
Let’s keep on digging into the why, y’all. (Image)
Hold your horses! I’m getting there, but I believe that diving into the details will help you to LEARN the clinical indications which is >>> than trying to memorize (no cramming and dumping, guys).
Anyhooo, before I was so rudely interrupted, we were discussing ion transport.
Important transporters to be aware of are the sodium-potassium and the sodium-chloride pumps. Thiazide diuretics inhibit the sodium-chloride symporter on the luminal surface (urine side) of the distal convoluted tubule, blocking sodium reabsorption and thereby promoting diuresis.
YAY you went to the potty!
So what happens with other ions in response to this blockage of the sodium-chloride cotransporter in the DCT?
Remember, the inside of our cells is naturally low in sodium, and blocking the influx with thiazides makes the nephron cells look for sodium to bring in at alternative places. Although not fully understood just yet, it’s possible the PCT compensates for loss of sodium in the DCT by ramping up sodium reabsorption at that site. And because sodium and calcium travel in tandem in the PCT, the end result is increased calcium reabsorption.
(Image)
It’s also possible that this compensatory mechanism is local to the DCT. In order to compensate for the blockage of sodium reabsorption by the sodium-chloride symporter in the DCT and because of the change in sodium gradient across the DCT cell, the flow of ions through the sodium-calcium antiporter on the basolateral surface (blood side) of the cell may increase. This attempt by the DCT cell to restore more intracellular sodium then would result in enhanced calcium reabsorption in the blood.
There is also a sodium-potassium antiporter that excretes potassium into the urine in favor of retaining sodium.
Basically, the DCT cell is a tenacious girl and will do whatever she can to bring in sodium.
Knowing these compensation mechanisms will help you remember the side effect profile of thiazides that we’ll discuss later. For now, know that thiazides primarily cause natriuresis, and as a result, some diuresis.
Meet the Thiazide Diuretic Family Members
The thiazide diuretics were introduced in 1958 by Merck Sharp & Dohme. For over 60 years, thiazides have been a mainstay in the management of various disease states requiring diuresis.
So who are they?
Chlorothiazide was the first thiazide diuretic to hit the market. It is available in both oral and IV formulations (but beware, IV is $$$). The plasma half-life is short at 45-120 minutes, and it’s usually dosed 500-2000mg in 1-2 divided doses.
No benefit and decreased safety? Nay nay. (Image)
Hydrochlorothiazide or HCTZ is the cheapest thiazide diuretic and is often seen in combination with other antihypertensive medications. The plasma half-life is 2.5 hours, and it is dosed 12.5-50mg PO daily. That being said, doses are usually capped at 25mg because there is an increased risk of adverse effects with no additional benefits when the dose is increased to 50mg.
Next are the thiazide-like diuretics. I think of these as the cousins - they are thiazide-like in action but not structure.
Metolazone has a half-life 8-14 hours. It’s most often used as an adjunctive agent in edema. It’s usually dosed at 2.5-20mg PO daily and can be used in patients with lower GFRs. Metolazone 5mg is roughly equivalent to HCTZ 50mg.
Indapamide has only mild diuretic activity but exerts antihypertensive activity through vasodilation. The plasma half-life is around 14 hours, and doses range from 1.25-5mg taken PO once daily.
Chlorthalidone has the longest half-life at around 40-60 hours (clingy much?). It’s dosed at 12.5 - 50mg PO daily. As with HCTZ, doses above 25mg have not been shown to increase antihypertensive benefits.
When are Thiazide Diuretics Used?
To remember the clinical indications of the thiazides, use the acronym CHIC:
C: congestive heart failure (CHF) + H: hypertension
Sodium wasting works to lower blood pressure, which is beneficial in both CHF and hypertension.
HCTZ and chlorthalidone are considered first-line therapies in the management of hypertension in patients without compelling indications for other medications.
I: diabetes insipidus (DI)
In DI, the kidneys are less responsive to antidiuretic hormone. This leads to the loss of greater volumes of water as compared to sodium. The body interprets this state as hypernatremic and increases the thirst mechanism. Thiazides release more sodium in the highly diluted urine, thereby breaking the polydipsia/polyuria cycle.
C: calcium calculi (aka calcium-containing stones)
The mechanism by which calcium is reabsorbed out of the urine is beneficial in reducing the formation of kidney stones.
Which Thiazide Diuretic is the Best?
There have been no trials directly comparing cardiovascular outcomes between the thiazide diuretics. Large trials support cardiovascular disease (CVD) benefits with chlorthalidone compared with HCTZ, although this is still somewhat controversial. It’s hypothesized that the longer half-life of chlorthalidone provides a benefit over HCTZ considering the latter’s short half-life and mismatched once-daily dosing.
So currently, chlorthalidone is the preferred starting thiazide in hypertension.
For Which Patients are Thiazide Diuretics Preferred?
Thiazide diuretics are preferred in African American patients without chronic kidney disease (CKD) (ALLHAT Trial) and in patients with history of stroke (PROGRESS Trial).
Patients with osteoporosis who require diuretic therapy may benefit from the enhanced calcium reabsorption effect. Use of thiazides in patients with gout should be done with caution due to its hyperuricemic effects. Patients with diabetes may experience slightly worsened glucose control when placed on a thiazide diuretic.
How Should We Monitor Thiazide Diuretics?
As exhibited by the mechanism of action, thiazides have a significant effect on ion balance, which can lead to:
Volume depletion
Hyponatremia
Hypokalemia
Hypercalcemia
Hyperuricemia
Hyperglycemia
Increased magnesium excretions
Decreased hydrogen reabsorption
Even if you’re 99% sure there’s not an interaction, just check it. Seriously. (Image)
Drug Interactions with Thiazide Diuretics*
Reduced efficacy with NSAIDs
Enhanced hypokalemia with corticosteroids
Increased risk of rhythm disturbances
Potentiated hyperglycemia with beta blockers
Reduced efficacy of uricosuric medications
Increased blood levels of lithium
* not all-inclusive, always run a Drug-Drug Interaction Check!
Clinical Pearls for Thiazide Diuretics
Thiazides are protein-bound, meaning they aren’t really filtered through the glomerulus. In order to reach their site of action in the DCT, they enter the tubular fluid by secretion through the PCT. This secretion is GFR-dependent. Lower GFRs result in less drug entering the tubular fluid. Therefore, patients with CrCl < 30ml/min are unlikely to benefit from thiazide therapy because the medication just plain can’t get to where it needs to go.
Thiazides are sulfonamide derivatives, so use is cautioned in patients with a true sulfa-allergy given there may be cross-reactivity. In patients with a severe sulfa-allergy, we may opt for a different class of diuretic (not necessarily the loop diuretics either).
Thiazides are on the Beers list for potentially inappropriate medications in the elderly. This doesn’t mean go pry Miss Smith’s HCTZ prescription from her hands! Just use it with caution and monitor her electrolytes closely.
Yay! You made it to the end! You go, Glenn CoCo!!
To wrap it all up, thiazides are diuretics with strong natriuresis. They are extremely cost-effective options for patients managing various disease states. Thiazides are great in that we may be able to use their side effects to our advantage, particularly in patients with osteoporosis and kidney stones.
BTW - We compiled ALL of our Pharmacology 101 posts into one handy, downloadable (and printer-friendly) PDF. You can get your copy of it here.