An Introduction to Pediatric Acute Lymphoblastic Leukemia (ALL)
Steph’s Note: This week, we’re going back to pediatrics and flavoring it with some oncology to boot. Here to team up with tl;dr and help us down this road is Heather Honor, a recent graduate from the University of Connecticut School of Pharmacy. She has now started her PGY1 residency at Dartmouth-Hitchcock Medical Center, and you may remember her from her previous pediatric post on common childhood infectious diseases. Take it away, Heather!
And BTW…we’ve got a super handy Pediatric Pharmacy Pocket Guide that gives you the ins and outs of all things peds. It’s an absolute life-saver…especially if you only occasionally come across pediatric patients in your practice. Check it out here!
Back to pediatrics, but this time, focusing on Acute Lymphoblastic Leukemia (ALL)! What is it? How can we treat it? Well, let’s get started.
The Basics of Pediatric ALL
ALL is estimated to account for a quarter of cancer cases in patients under the age of 15, and it’s the most common childhood cancer overall with ~41 new cases per 1 million children aged 0-14 years in the US. Incidence of ALL peaks around years 2-3 with rates 4 times higher in that age group than that in either infants or children at least 10 years old. Hispanic children appear to have the highest risk, followed by White children, who are in turn at ~3 fold higher risk than Black children. Although the incidence of pediatric ALL has been on the rise since 1975, the good news is that the 5-year survival rate has increased from ~60% to ~90% for children younger than 15 years within that same time frame.
(So the bad news is we’re diagnosing more ALL cases… But the good news is we’re learning how to better treat it. Enter pharmacy! But first, more background…)
Take a quick refresher with the blood cell development paths in the figure here, and note that the 2 main lineages are the myeloid and lymphoid paths. (Image)
The cause of acute lymphoblastic leukemia (ALL) is a variable slew of genetic mutations in blood progenitor cells, specifically those that are part of the immune system. In ALL, there is an issue in the lymphoid development path, leading to an increase in blasts of B or T cell subtypes. (“Blasts” or “lymphoblasts” is just another name for immature blood cells.) So ALL patients may be categorized according to predominance of B or T blast cells, as well as how mature those cells are, which altogether is called the immunophenotype of the malignancy.
The majority of pediatric ALL cases exhibit the B cell immunophenotype, as determined by finding high levels of CD10 and CD19 markers on the cells. A smaller portion of pediatric ALL patients have T cell surface markers, e.g., CD3, making them a T cell immunophenotype.
The reason for ALL development has not been fully elucidated, but there are a number of proposed and accepted risk factors for increased risk of leukemias, both environmental and genetic:
Environmental Risk Factors
Exposure to x-rays prior to birth
Exposure to radiation after birth (even therapeutic radiation)
Treatment with chemotherapy (e.g., cyclophosphamide and etoposide)
Intensive immunosuppression (e.g., after an organ transplant)
Having an identical twin with leukemia, especially during ages 0-1 year
Down syndrome (~2-3% of childhood ALL cases)
Neurofibromatosis (NF1)
Not gonna lie. I hadn’t heard of most of those either before researching this post. But many of them are related to genetic disorders of the immune system, so it’s not entirely out of left field that they could also be implicated in a lymphoproliferative disorder of the immune cells.
(Image)
Symptoms and Diagnosis of Pediatric ALL
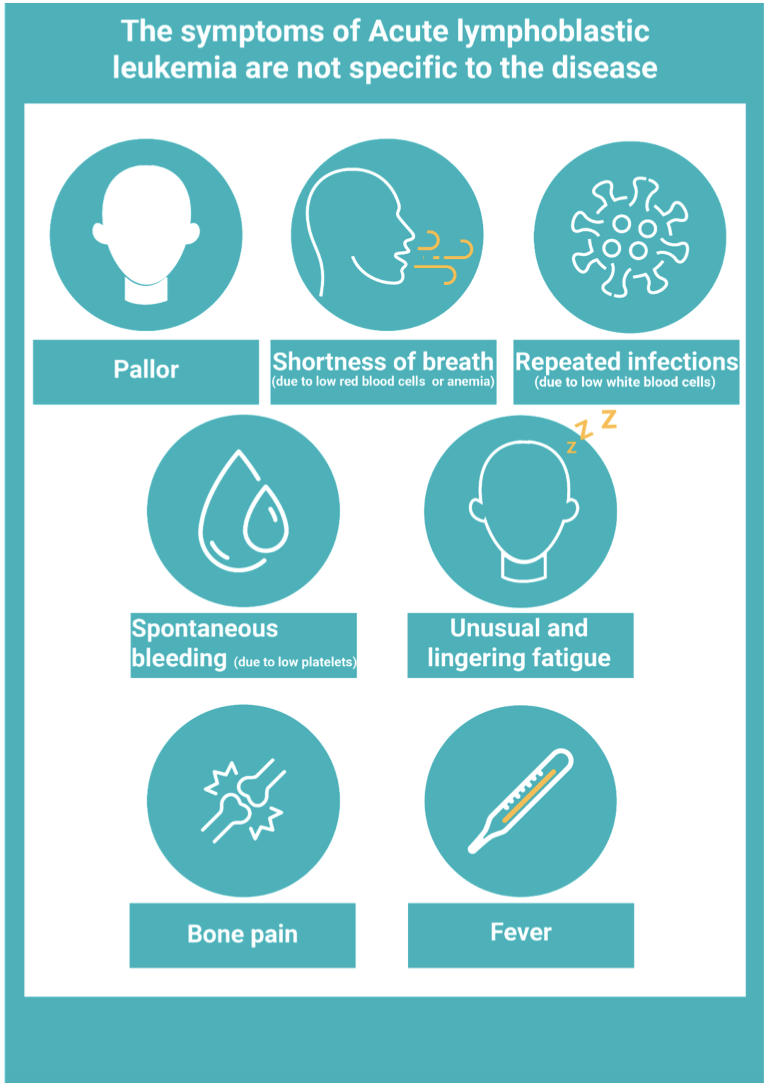
When a child presents with ALL, a lot of the symptoms can be non-specific. (This can make it really tricky without further evaluation to recognize that something more serious may be developing.) These symptoms are often directly related to the overgrowth of the lymphoblasts in the bone marrow.
For example, fatigue, bruising, chills, pale skin, and shortness of breath can all be related to anemia and/or thrombocytopenia, which arise when out-of-control lymphoblasts crowd out the bone marrow and don’t allow for normal numbers of red blood cells (RBC) or platelets.
Additionally, increased infections and fevers arise because of the lack of normal white blood cells (WBC). (This can be confusing because often the WBC count may actually be elevated on lab work. But just because the counts are high doesn’t mean the cell subsets or their functionality are normal for fighting infections!)
Other ALL symptoms can include the following:
bone or joint pain (related to the overcrowding of cells in the marrow),
abdominal pain (often secondary to an enlarged spleen and liver, which can often harbor these increased numbers of immune cells),
anorexia (loss of appetite caused by enlarged organs causing a feeling of fullness),
swollen lymph nodes (caused by increased numbers of WBC sequestering in these fortresses), and
extreme fatigue or weakness (caused by elevated WBC slowing circulation through the vasculature).
Not to turn everyone into a hypochondriac, but how many of you have experienced at least some these symptoms when you have a cold or flu?
Yeah. That’s part of what makes this so tricky, and it’s also why further objective evaluation is essential.
The bone marrow aspiration and biopsy procedure. Aspiration removes a sample of the liquid portion of the bone marrow, whereas a biopsy removes a solid core sample of the marrow. Patients usually receive local anesthetics and some mild sedation for this. (Image)
Diagnosing leukemia always involves obtaining a complete blood count (CBC) with differential to evaluate the subsets of WBC. Other pieces of diagnosis often include performing a bone marrow biopsy, obtaining imaging, such as x-rays, ultrasounds, and CT scans, and sometimes even conducting a spinal tap, aka lumbar puncture.
Each individual patient’s diagnostic course may vary slightly depending on the results of previous tests. For example, if a patient has an abnormal CBC and bone marrow biopsy, but they have imaging that doesn’t demonstrate spread of the disease, they might not undergo a lumbar puncture as that would only be useful for seeing if the leukemic cells had spread to the cerebrospinal fluid (CSF).
When evaluating the CBC, the RBC and platelet count are often low, indicating anemia and thrombocytopenia, respectively. As for the WBC, either leukocytosis or leukopenia may be present, with one 2019 study finding each o these scenarios present in ~36% of new ALL diagnoses. The CBC may also be evaluated by a pathologist, who performs a blood smear to look for blast cells. If there is a large number of blast cells, the lab may then perform a flow cytometry test to determine if the lymphoblasts are predominately B or T cells.
(Image)
In addition to the slew of diagnostic tests already mentions, patients often undergo further genetic tests to help narrow treatment options as many of these specific mutations are uniquely treatable. One of the most common mutations is a translocation, BCR-ABL, also known as the Philadelphia chromosome. (There are many more, including FLT3, PAX5, ETV6, E2A-PBX1, and HOX, but the cytogenetics of ALL is a topic for extra reading!)
(Image)
Because the BCR-ABL translocation has been a source of large amount of attention in the past decade for several types of leukemias (not just ALL), it’s something that pharmacists across lots of practice areas should be familiar with. So we’ll take just a moment to describe this mutation a little further.
The Philadelphia chromosome (or BCR-ABL fusion mutation) is found in ~3% of pediatric ALL patients with increasing incidence (up to 25%) in the older cohort of pediatric patients. Until recent years, presence of this mutation pretty much meant a patient was headed for a stem cell transplant. In the last decade or so, however, starting with the approval of Imatinib (Gleevec) in 2001, outlook for these patients has drastically improved with multiple drugs now approved in the tyrosine kinase inhibitor class.
One last part of diagnosis is risk stratification since this can impact treatment decisions. Is the patient at low, standard, or high risk?
Age and WBC are considerable factors in this. Patients aged 1-9 years have a better prognosis. If the patient is less than 1 year old or greater than 10 years old at the time of diagnosis, they are considered high-risk. As for WBC, if they have counts greater than 50,000 cells/m3, they are at higher risk and need more intensive treatment. One other factor to consider in risk assessment is B cell versus T cell subtype. In general, early B cell ALL subtypes tend to fair better than mature B cell or T cell disease.
Pharmacotherapy of Pediatric ALL
Finally… the PHARMACY!!! (But honestly, it’s so important to understand some background before we jump into the medications. Yes, we’re pharmacists but context matters! It’s not #allmedsallthetime.) Anyways…
ALL treatment regimens all follow a standard 3 or 4 step process (depending on your resource) with a different goal for each phase:
Induction therapy
This is the most intense phase, usually lasting about 4 weeks, and its goal is to kill the leukemic cells and allow for restoration of normal bone marrow function. Another goal of induction is to achieve minimal residual disease (MRD). MRD is the percentage of cancer cells that are left after induction. The lower the number (shooting for undetectable!), the better the outcome is for the patient.
Consolidation/intensification therapy
The goal of this second phase is to kill any and all of the lingering rogue leukemia cells throughout the body.
Maintenance therapy
The goal of maintenance is to prevent the leukemic cells from repopulating.
This phase alone can last years with the ultimate hope being to achieve remission or “cure.”
Luckily, pediatric ALL actually has one of the highest cure rates! If patients have a relapse in disease, treatment options are often dependent on when or where the disease returns.
A lot of these medications are combined into various, complex treatment protocols, which is very common when treating childhood cancers. The Children’s Oncology Group constantly has new protocols and studies for patients to enroll in. The patient can also follow a study protocol that has since become standard of care as well.
Some of the common medications that are used for treatment of pediatric ALL are vincristine, methotrexate, daunorubicin, asparaginase, and dexamethasone or prednisone. A few pearls on these…
Vinca alkaloids, including vincristine = DO NOT GIVE INTRATHECALLY!! Remember this for all tests and patient care. (Image)
Vincristine is a cornerstone medication used in treatment of ALL. One major side effect is neuropathy, which we try to mitigate by capping a single dose at 2mg. (Note, MILLIGRAMS, NOT GRAMS!) Also, vincristine has actually been fatal in patients when administered intrathecally. Therefore, institutions place auxiliary labels on it such as “IV Only” to make the staff aware, and it absolutely requires extra care when processing and checking orders!
Methotrexate is commonly used in this patient population to help treat or prevent disease within the CNS. One major concern in ALL is that the CNS can be a sanctuary site for leukemic cells. By targeting the CNS with intrathecal methotrexate, we hope to prevent this from happening. One thing to consider when using intrathecal methotrexate is the CNS fluid volume, which surprisingly reaches adult volume by the age of 5!
As for daunorubicin, it can help prevent further cell growth by stopping DNA synthesis. Daunorubicin is an anthracycline, which requires careful monitoring of total lifetime doses due to risk of cardiotoxicity. The maximum cumulative dose is not necessarily the same for everyone and often depends on age, comorbidities, and concomitant therapies, like radiation. Once ALL patients begin to get close to their determined lifetime dose or there are concerns for developing cardiotoxicity, dexrazoxane, which is a protectant against anthracyclines (i.e., doxorubicin, daunorubicin), can be administered off-label.
Here’s a drug chart with some more important information about these and the other medications:
As mentioned earlier, this slew of medications is administered in cycles, and the combinations vary based on what phase of treatment and study the patient is currently in. Some studies have added or removed medications depending on the focus of the trial. As just one example of what these regimens may look like, for the study AALL0631 and patients that are at least 6 months old at the time of diagnosis, the schedule looks like this:
So complicated!! This is where pharmacists can help to keep track of regimens and ensure medications are dosed and timed appropriately. (Image)
So is all the effort required by these complicated regimens worth it? How well do they work against ALL??
Definitely worth it!! With current regimens, the 5-year survival rate for patients with childhood ALL is above 85% in developed countries. However, although we have achieved this high rate of survival, there is still no consensus on what makes a regimen optimal. The development of more specific treatment options targeting mutations will likely further improve the survival rate overall, with a bigger effect on those with the more difficult to target or treat mutations.
As mentioned previously, BCR-ABL mutations used to be more difficult to treat, but with the development of medications such as imatinib (Gleevec), nilotinib (Tasigna), and more, those patients have seen significant improvements in outcomes. In addition to BCR-ABL, JAK1/2 mutations have targeted treatments available such as ruxolitinib (Jakafi). Over time, risk stratification strategies have also improved. This allows for more precise determinations of what treatments will be beneficial, especially for those who weren’t always considered high-risk.
Supportive Care for Patients with Pediatric ALL
In every oncology patient, supportive care is extremely important. Some oncologic medications require pre-medication before administration, and some require medications afterwards to help with blood marrow recovery, such as peg-filgrastim (Neulasta). Other important, yet simple medications that can be used to improve patients’ experiences throughout their treatment processes include acetaminophen, antiemetics, and antihistamines (e.g., diphenhydramine).
Bone marrow recovery is very important in cancer treatment because many chemotherapy protocols require patients’ blood counts to meet certain thresholds prior to initiating the next cycle of treatment. So it’s not uncommon for patients to have to delay the next cycle due to low blood counts (e.g., neutrophils).
With treatments such as filgrastim or peg-fligrastim, patients are able to achieve bone marrow recovery more quickly and therefore continue with chemotherapy on schedule. When treating patients with this medication, it’s important to remember that they are not achieving this recovery on their own, and sometimes, this quicker recovery comes at the price of some adverse effects (check out the table to the right for just a few examples).
Another important factor with regards to supportive care is consideration of the medications’ emetic risk. The National Comprehensive Cancer Network (NCCN) has some pretty awesome guidelines regarding oncology supportive care treatments, especially when it comes to emetic risk. The guidelines go into great detail about each medication and how likely it is for the patient to become nauseated or vomit during treatment.
Depending on the emetic risk of the medication, specific pre-medications can be administered to prevent those symptoms. For example, daunorubicin falls under moderate emetic risk, and according to the NCCN guidelines, patients should receive a 5-HT3 antagonist (e.g., ondansetron) + steroid +/- an NK-1 antagonist (e.g., aprepitant).
Emergencies in Pediatric ALL
Tumor Lysis Syndrome (TLS) is a medical emergency, should it occur during induction therapy (or any time, really!). For a full review, see this previous tl;dr post. But here’s the quick run down on TLS.
When chemotherapy is administered, tumor cells break down, or lyse. This lysis releases intracellular contents into the bloodstream, which include potassium, phosphate, purines, and pyrimidines. Once these materials are in the circulation, many complications can occur, such as hypocalcemia, hyperkalemia, hyperphosphatemia, and hyperuricemia.
You can likely imagine how the incidence of TLS is increased with lymphoproliferative disorders, where there are SO MANY extra cells floating around. One 2019 study found a TLS incidence of over 62% in 91 pediatric ALL patients - despite preventative measures. Eek!
We often try to prevent TLS from occurring by giving high risk patients allopurinol (yep, the gout medication). This is started ~12-24 hours prior to chemotherapy and is continued until uric acid levels normalize. The dose is 300-450 mg/m2/day given in three divided doses (up to 400 mg daily). Allopurinol competitively inhibits the production of uric acid by blocking the enzyme xanthine oxidase. Important note, allopurinol doesn’t do anything to uric acid already present; rather, it prevents the future development of uric acid. This is why it’s beneficial to start it prior to chemotherapy, especially in those patients at high risk for developing TLS. (Interesting fact, allopurinol is also available IV.)
Another medication that may be used for TLS is rasburicase, which converts uric acid to allantoin. Allantoin is more water-soluble and therefore easier for the kidneys to excrete. The downside? Rasburicase is rather expensive, so it’s really used as a second line agent. Dosing for this medication is 0.15-0.2 mg/kg/day, given once daily. What’s the pearl to log away here? Patients who have a G6PD deficiency cannot receive this medication, but it can beneficial in those that experience an allopurinol-induced rash.
Btw, there was going to be an extravasation sample pic inserted here, but honestly, not sure all of you want these images put in front of you. If you’re curious, there’s google. Just take this as fair warning… extravasation can be really painful and destructive to tissues! For you others who don’t want to google it, here’s a fluffy puppy. (Image)
Our next emergency is extravasation, which means that the drug didn’t go where it was supposed to! (Extra. Vasation. Literally outside the vasculature.)
That is, it was supposed to infuse through the IV line and stay in the blood vessels, but it ended up outside the IV line or blood vessels… going into tissue. Yikes.
Although risk of extravasation is thought to be related to multiple factors, including drug-specific issues (pH, osmolality, etc), patient-specific factors (e.g., infections, predisposition to leaky vessels, etc.), and mechanical problems (IV insertion technique), extravasation is often a topic with oncology medications because many of them are vesicants. Vesicants can result in the formation of blisters or even lead to tissue necrosis if they are infused into the area surrounding the vein. Double yikes!
One way to help prevent extravasation from occurring is to infuse these medications via central lines or ports. In a lot of pediatric patients, central lines are preferred for many reasons. The smaller the patient, the smaller the vein, which means increased difficulty in obtaining longer term access.
As for the extravasation, It’s good to know how to treat it, if it happens. When talking specifically about ALL chemotherapy, a warm compress should be applied at the extravasation site for vincristine. The warmth helps to increase blood flow through the area, which enhances drug circulation out of the damaged locale.
If the vincristine extravasation is severe enough, there is also an antidote, hyaluronidase. This medication is injected in multiple small increments at the site of the extravasation. It’s an enzyme that breaks down hyaluronic acid between cells, allowing for more rapid distribution of drug out of the local area (and for increased influx of surrounding fluid, which decreases the concentration of the extravasated drug even further).
On the other hand, for daunorubicin, a cold compress should be applied, which causes vasoconstriction and limits spread of the extravasated medication. (Remember, every medication has different properties… So for some, we may want that rogue medication to distribute ASAP out of the tissue area, whereas for others we want to keep it corralled). Other options for duanorubicin extravasation include dexrazoxane or dimethylsulfoxide.
For any horse crazy people out there, yes, we’re talking about THE dimethylsulfoxide, better known as DMSO. This (originally industrial-based) solvent is thought to increase distribution of the extravasated medication out of the local area by increasing tissue permeability and also may have free radical scavenging abilities. So it’s not just a topical anti-inflammatory for horses.
Also, don’t panic. Because it’s pretty impossible to keep straight warm versus cold compresses and exact antidotes for every administered medication, most institutions have easily-accessed extravasation protocols.
The image below is a good visual for steps a nurse might take if extravasation is suspected. Notice the difference between DNA-binding drugs and non-DNA binding drugs and how important it is for the medical team to know which agents fall under what path.
(Image)
The tl;dr of Pediatric ALL
As you now know, pediatric ALL is quite an interesting disease state, right? The genetic component alone is just a whole other level! From BCR-ABL to JAK1/2 mutations, it’s fascinating to watch the pipeline for new medications targeting those specifically or even the likely discovery of new mutations as well. Personally, the thing that excites me the most is the high cure rate!
Also, extravasation?! That was something I didn’t even know existed until I learned about it in class. Pharmacists can play such a huge role in knowing which medications are vesicants, irritants, and non-irritants, and then being able to recommend pharmacological and non-pharmacological treatment options.
As for us pharmacists, working in pediatrics is quite a specialty, and not everyone is comfortable in this realm. But if you are and would like to know how to become a pediatric hematology/oncology pharmacist there are many options for training. You could do a PGY1 into a PGY2 in pediatric hematology/oncology (think Memorial Sloan Kettering), a PGY1 at a children’s hospital and work your way up, or even doing a PGY1 then a PGY2 in general pediatrics and working your way into pediatric hematology/oncology pharmacy!