The Pharmacist's Rundown on Adult Vaccinations
Steph’s Note: Please welcome back one of our newest community pharmacy tl;dr voices, Carley Moses, PharmD. If you haven’t met her yet, you should definitely check out her debut post on chronic care management. As we’ve told her multiple times already, she really has a knack for being able to explain a whole lotta info in an easy-to-understand way. It’s like she’s on our tl;dr wavelength. Maybe we understand each other so well because of a deep seated, shared passion for tacos. Whatever it is, we love her, and we’re so glad she’s back this week to give us the rundown on adult vaccines every pharmacist should understand.
So, someone walked up to your pharmacy counter and asked for any and every vaccine they could possibly get, huh? Or maybe you work inpatient, and your colleagues are looking for vaccination recommendations before a patient discharges?
The HIMYM woo girls are hyped, so you should be too! (Of course, I’m betting they have a little more liquid assistance with their woos than you currently do…) (Image)
No problem!!
Let’s get down and dirty on vaccines, their side effects, and who should avoid them. (Spoiler alert: there are very few people who fall into the avoid category🙂).
But before we get into the specifics about vaccines, let’s do a quick vaccine and immunology refresher!! WOOOO!! I’m trying to hype you up here!!
Types of Vaccinations
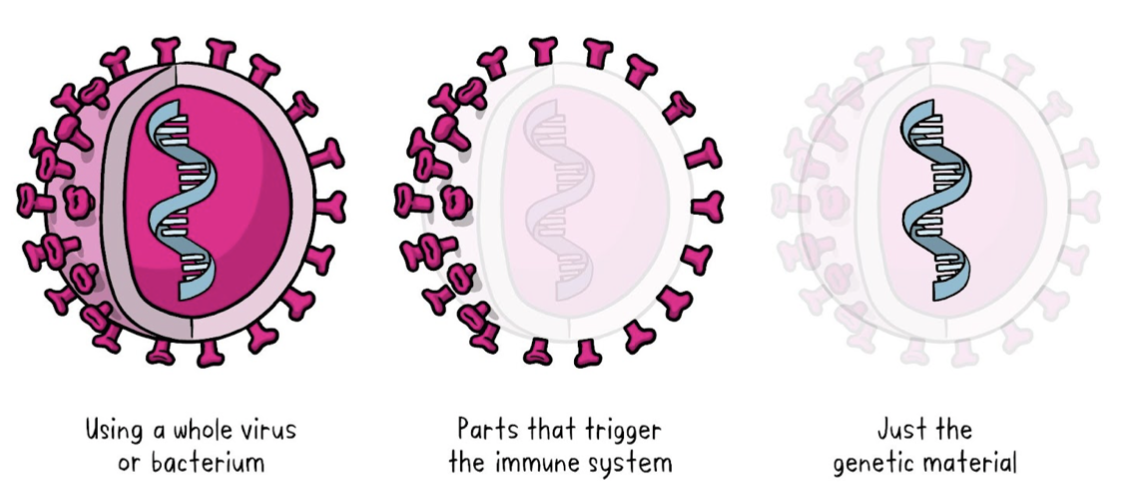
To get started, let’s cover the main formulations of vaccines that exist.
(Image)
Vaccine formulations can typically be broken down into three categories:
Vaccines containing the entire virus or bacteria that we are attempting to protect against,
Vaccines that contain specific antigens - or pieces of the virus or bacteria that our body thinks is foreign - that we are protecting against like a surface protein or toxin, and
Vaccines that contain only genetic material that typically accounts for the production of an antigen such as a surface protein.
Let’s start with our big boys that contain the ENTIRE virus or bacteria:
(Image)
Whole Virus or Bacteria Vaccines
Inactivated Vaccines
These vaccines contain killed or inactive forms of the virus or bacteria that you are protecting against. These vaccines are more common than live attenuated vaccines as they do not pose the same side effect risks (since the virus or bacteria are not active). We’re going to talk about a couple different inactivated vaccines including a different influenza vaccine, and the hepatitis A vaccine.
Live Attenuated Vaccines
These vaccines contain a super weak form of the virus or bacteria that you are protecting against. One example of a live vaccine that we will discuss is one formulation of the influenza vaccine, which contains weakened influenza strains for our bodies to mount a response to. Since these vaccines do contain live bugs, we need to take special care with our immunocompromised and pregnant patients as they can cause more severe side effects in these populations.
Next, we’ll dive into our subunit vaccines.
Subunit Vaccines
(Image)
Remember, rather than presenting the entire virus or bacteria, now we’re only presenting pieces of them for our body to recognize and mount a response to.
Recombinant Vaccines
Contrary to the above vaccines, the recombinant vaccines work using recombinant DNA technology to produce an antigen for presentation using a separate host. These vaccines use a specific gene from the pathogen you’re trying to protect against, usually a surface protein, and they insert that gene into a separate host like yeast or bacteria for antigen production.
Essentially, we insert this foreign gene into our host, and it goes CRAZY making those surface proteins, AKA our antigens. Once those antigens are floating all around our body, our immune system recognizes the specific antigen and forms an immune response. We see this type of response with our shingles and hepatitis B vaccines we’ll discuss.
Conjugate Vaccines
Similar to our recombinant vaccines, the conjugate vaccines only contain small portions of the virus or bacteria rather than the whole thing. But in the case of conjugate vaccines, whatever antigen we are looking to mount a response to is attached to a carrier protein, kind of like a backpack. This carrier protein helps to carry all those tiny bug pieces around for our immune system to find and mount a response to. We’ll discuss these when we talk about pneumococcal vaccines.
Toxoid Vaccines
These vaccines are different from any of the vaccines above. They contain the specific toxins related to the virus or bacteria that we want to protect against. Our body recognizes these toxins as antigens and mounts an immune response directly to the toxin rather than to a part of the virus or bacteria. Our example of these vaccines include the tetanus, diphtheria, and pertussis vaccine, which we will discuss in a bit.
And finally, we have our genetic vaccines.
Genetic Vaccines
These bad boys use a part of the virus or bacteria’s genetic code to provide instructions to create specific proteins for our immune system to recognize rather than presenting the whole virus or bacteria, or even pieces of it.
Almost like downloading a software code to produce surface proteins…kinda cool right??
mRNA Vaccines
Ahhhh, our newest vaccine technology. This technology debuted with the COVID-19 vaccines and involves injecting genetic material from the virus or bacteria we are protecting against. Once injected, the mRNA stimulates the production of proteins specific to the virus or bacteria we are protecting against. Our body finds these proteins floating around, says, “THAT’S NOT OUR PROTEIN,” and mounts an immune response to protect us against that disease.
Now all of that sounds great - but I know what you’re thinking. What does “mount an immune response” even mean?? What happens once these things are in our bodies?? How do I even know it worked?? Let me introduce you to my friend…immunology.
How Do Vaccines Work with the Immune System?
Let’s start with antigens since we’ve dropped that buzzword a few times. An antigen is simply something floating around our bodies that our immune system knows isn’t ours.
Random virus? Antigen.
Random bacteria? Antigen.
Surface protein? Antigen.
Heck, dust in the air? You got it, that’s not supposed to be there. Antigen.
So when we inject a vaccine, whether the whole virus or bacteria or just a subunit as we discussed, our body seeks out those foreign antigens and goes to work.
(Image)
How exactly does it go to work?
Well, you see, we have specific cells for anything that presents an antigen in our body…and they are appropriately named antigen-presenting cells or APCs. They recognize these foreign antigens in our blood, break them all down into tiny pieces, and display them like trophies on the surface of their cells. The white blood cells in our immune system, specifically our T cells and B cells, get a little jealous of these trophies, so they come to check our APCs out.
Now our T cells typically provide two role. The cytotoxic T cells (TC) attack infected cells, and the helper T cells (TH) recruit other homies to help with infected cells. Our helper T cells are the ones who find our APCs, and they also release cytokines that call in the other big boys (like our B cells) to come help. Unlike the helper T cells which require assistance to carry out their assassinations, the cytotoxic T cells can recognize the little antigen fragments on infected cells and attack and kill those cells directly. They take care o’ business.
Once the B cells arrive, the real fun begins. Our B cells begin to divide and produce large amounts of antibodies against all those antigen fragments. Once those antibodies are formed, they circulate through our blood looking for anything that resembles those trophy fragments. They ring the alarm anytime they find one to either kill the trophy antigen or get it ready for killing by other immune cells.
Now, wanna hear something REALLY cool??
Once our B cells make those antibodies one time, some of our B cells develop into memory B cells. Essentially, these B cells remember all of the trauma they’ve been put through and can make those SAME antibodies again in the distant future if they run into that antigen again.
We maximize how well vaccines work by using this information to our advantage and providing booster doses. Essentially, when we provide a booster dose of a vaccine, we wake up those memory B cells and yell, “WE NEED MORE OF THESE ANTIBODIES! DON’T STOP NOW!” This further reinforces the formation of more memory B cells to protect us even longer into the future.
(For a full immune system refresher, also check out out this previous tl;dr post.)
But how do we know if a vaccine did as intended?? Now’s the time to introduce you to my other friend named titer.
Vaccines and Titers
We can use a vaccine titer to measure how many antibodies are present in your blood to a specific antigen or disease. It’s important to note that titers detect antibodies formed both from vaccination, as well as natural exposure to the bacteria or virus itself.
We use titers to determine just how protected we are against a disease. For example, before you start working in healthcare, you may have to have a hepatitis B titer performed. This titer checks to see if you still have sufficient antibodies from a previous hepatitis B vaccination to protect you against hepatitis B infection.
We can use this information to make clinical decisions to protect our patients further. If someone’s hepatitis B titer comes back negative, we can give them a booster dose of the hepatitis B vaccine to try and wake up those memory B cells we talked about to make more antibodies before they are exposed to potential dangers (e.g., needle sticks). On the other hand, if that person’s hepatitis B titer is positive, we can conclude that their B cells have still been hard at work making antibodies; therefore, they likely have adequate protection against hepatitis B.
Now that all of the nitty-gritty is out of the way, let’s talk about specific vaccines.
Adult Vaccinations All Pharmacists Need to Understand
COVID-19 Vaccines
Currently, there are three COVID-19 vaccines that we use in the United States: the Pfizer-BioNTech vaccine, the Moderna vaccine, and the Johnson & Johnson (Janssen) vaccine. The Pfizer-BioNTech and Moderna vaccines use messenger RNA (mRNA) to teach our own cells to produce a piece of the spike protein found on the surface of COVID-19, while the Johnson & Johnson vaccine uses a modified adenovirus to carry genetic material from COVID-19 into cells. By recognizing the spike protein or the genetic material, our immune systems can produce antibodies and activate immune cells to fight off the virus for us (pretty cool, right?).
(Image)
The COVID-19 vaccine is recommended for nearly all adults. The vaccine is especially important for people at higher risk for severe illness from COVID-19, including older adults, people with certain underlying medical conditions, and healthcare workers (hey, that’s us!!). The vaccine is also important for those who have previously had COVID-19 because we still don’t quite know how long immunity from natural infection lasts.
There are very few absolute contraindications to the COVID-19 vaccines; however, people who have had severe allergic reactions to any of the vaccine components such as polysorbate (which is found in ice cream), or polyethylene glycol (AKA colonoscopy prep solution), or to a previous dose of the vaccine should not receive the vaccine. People who are currently positive for COVID-19 should wait until they have recovered before receiving the vaccine. For a full reference of clinical considerations regarding use of the COVID-19 vaccines, check this CDC site out.
Influenza Vaccines
The most common types of flu vaccines are the inactivated influenza vaccine (IIV), which contains inactivated flu viruses, the recombinant influenza vaccine (RIV), which contains genetic material from flu viruses, and the live attenuated influenza vaccine (LAIV), which contains a tiny baby dose of the live viruses. The inactivated influenza vaccine is the most commonly recommended.
In addition to the various vaccine types, each flu vaccine covers a different numbers and strains of flu bugs. The most common flu vaccines are the trivalent and quadrivalent vaccines. The trivalent vaccine protects against three strains of the flu virus: two influenza A strains and one influenza B strain. The quadrivalent vaccine protects against four strains of the flu virus: two influenza A strains and two influenza B strains.
(Image)
We also have flu vaccines that are only for our loved ones 65 years and older, such as the high-dose vaccine (which contains FOUR TIMES the antigen of the regular dose vaccine) and the adjuvanted flu vaccine (which contains an adjuvant that helps to “beef up” your immune response to the vaccine).
The flu vaccine is recommended for all adults, particularly those who are at a higher risk of developing complications from the flu, such as older adults, people with certain chronic medical conditions, and our pregnant friends (flu vaccines for everyone!!). In rare cases, people may experience an allergic reaction. This is most common in those with egg allergies when receiving certain flu vaccines that contain preservatives.
Pneumococcal Vaccines
All of the pneumococcal vaccines protect against different kinds of pneumococcal bacteria, which can cause pneumonia, meningitis, and other serious infections. There are two main types of pneumococcal vaccines: pneumococcal conjugate vaccines (PCV13, PCV20, and PCV15) and pneumococcal polysaccharide vaccines (PPSV23).
The main difference between the pneumococcal conjugate vaccine (PCV) and the pneumococcal polysaccharide vaccine (PPSV) is how they induce an immune response in our bodies. PCV vaccines are designed to protect against pneumococcal bacteria by inducing an immune response to the bacterial polysaccharide antigen PLUS a protein carrier (remember our backpack analogy?). On the other hand, PPSV vaccines work by exposing the immune system to the bacterial polysaccharide antigens themselves (no shuttle or backpack needed 😎). The currently available pneumococcal vaccines include Prevnar 13™ (PCV13), Prevnar 20™ (PCV20), Vaxneuvance™ (PCV15), and Pneumovax™23 (PPSV23).
When you just need to find a quick answer for which pneumococcal vaccine a patient needs. (Image)
If you haven’t run into these recommendations before, the pneumococcal vaccine guidelines can be a little tricky. For the majority of our patients older than 65, as well as our patients aged 19-64 with high-risk factors, giving one dose of PCV20 is typically enough to complete their pneumococcal vaccines, regardless of what prior pneumococcal vaccines were given.
But what about the people who already got PCV13 or PPSV23??? OR BOTH??? WHAT IF I DON’T HAVE THE NEW VACCINES IN STOCK?? NOW WHAT???
Luckily for you, the CDC has not only guidelines, but 2 options for pneumococcal vaccine completion that are considered equally effective. Insert informative table!!
Note that option A typically involves completing the pneumococcal series with PCV20, whereas option B utilizes PCV15 in combination with the already common PPSV23 to complete the series.
Some colleagues may prefer a different combination of vaccines, depending on the patient’s risk factors. In this scenario, the CDC offers additional guidelines for different options for vaccine completion, based on what previous vaccines the patient has already received. An excellent resource for working through these options using patient-specific factors is the CDC’s PneumoRecs VaxAdvisor. This tool is available for both desktop and mobile application to help you pick the best pneumococcal vaccine combination for each of your patients.
Shingles Vaccine
The shingles vaccine works to prevent the painful rash that can last for several weeks (or even months!) caused by the varicella-zoster virus. Remember all the talk about the infamous chickenpox parties? Well, chickenpox is caused by the same virus. After you recover from chickenpox, the virus just kind of hangs out and sleeps in your body for a while. Then as we get older, our immune systems aren’t quite as strong, and guess who wakes back up?
You guessed it - the varicella-zoster virus.
Once this big guy wakes back up, BAM! Shingles time. The shingles vaccine, Shingrix™, is a recombinant vaccine that codes for a protein found on the surface of the varicella-zoster virus. Your body recognizes this protein as foreign and produces antibodies to that protein, which helps to protect us from reactivation of or exposure to the varicella-zoster virus in the future.
^^Steph, when she found out Shingrix had finally been approved in 2021 for immunocompromised patients under age 50 (after spending countless hours on prior authorizations!!) (Image)
Shingrix™ is recommended for all adults over the age of 50, as well as our immunocompromised homies aged 19-49. It’s given in two doses separated by 2 to 6 months. If your patient is immunocompromised and could benefit from a shorter vaccination period, the second dose can be moved up to 1 to 2 months after the first dose.
Of note, some patients may have received a prior formulation of the shingles vaccine, Zostavax™. This vaccine was live and is no longer indicated for use (or available in the US). Even if your patient was vaccinated with Zostavax™ previously, it is recommended that they be vaccinated again with Shingrix™ for full protection.
But what if your patient never had chickenpox? What if they were vaccinated against chickenpox as a kid rather than having a natural infection? How can that impact risk of shingles and/or need for the shingles vaccine?
Immunization against the varicella-zoster virus as a child is highly effective at preventing chickenpox; however, it can’t completely eliminate the chance of the virus entering our bodies. The chickenpox vaccine (Varivax®) is also a live vaccine, so we are technically actually introducing patients to the virus when we vaccinate them. For these reasons, those who received the chickenpox vaccine as a kid still have a risk of developing shingles and should consider the shingles vaccine.
Now don’t go hating on the chickenpox vaccine just because it’s not 100% perfect! Prior vaccination against chickenpox has been shown to lower the risk of getting shingles, as well as lowering the risk of having a severe case with complications. So it’s still a good thing to do!
Tetanus, Diphtheria, and Pertussis (Tdap/Td) Vaccines
The Tdap vaccine is a combination vaccine that protects against three different diseases (wow, fancy): tetanus, diphtheria, and pertussis (whooping cough).
Tetanus is caused by the bacteria Clostridium tetani. This scary bug produces a toxin that can cause muscle stiffness and spasms. Diphtheria is caused by the bacteria Corynebacterium diphtheriae, which also produces a toxin, but this time it damages the heart, kidneys, and nerves. Finally, pertussis, or whooping cough, is caused by the bacteria Bordetella pertussis, which, you guessed it, produces a toxin that causes severe coughing.
In the case of the Tdap and Td vaccines, they contain small amounts of the toxoids produced by both tetanus and diphtheria, as well as small pieces (or antigens) of the pertussis bacteria. Our bodies recognize these toxoids and bacteria pieces as foreign and form antibodies to prevent future illness by any of the 3 bacteria (or 2 bacteria in the case of Td).
There are currently two Tdap vaccines given in the United States: Boostrix™ and Adacel™. Both Boostrix™ and Adacel™ are approved for anyone over the age of 10; however, Adacel™ is only approved for use up to the age of 64. Anyone 65 years or older should always receive Boostrix™.
The Tdap vaccine is recommended for all adults, particularly those who are in close contact with babies. Specifically, pregnant ladies should receive a Tdap vaccine during each pregnancy, regardless of when their last vaccination was. This is typically given during weeks 27-36 of pregnancy, and it aids in protecting both mom and baby from whooping cough!
For all other adults, it’s recommended to receive at least one Tdap booster either at 11-12 years old or during adulthood, followed by a Tdap OR Td booster every ten years. The exception to the 10 years rule is if a patient has a special circumstance that puts them at higher risk of tetanus, diphtheria, or pertussis infection (we’re looking at you rusty nails and snotty kid noses).
The Td booster is similar to the Tdap booster but only contains tetanus toxoid and diphtheria toxoid, with no pertussis or whooping cough protection. Patients may opt to receive EITHER the Td or Tdap vaccine for their 10-year boosters following their initial Tdap booster, taking into consideration if they require pertussis protection.
Hepatitis A and B Vaccines
Finally, we have our hepatitis vaccines. Currently, we have vaccination options to protect against both the hepatitis A virus (HAV) as well as the hepatitis B virus (HBV), both of which infect the liver.
I mean, really, hepatitis A from restaurants shouldn’t even be a thing. Eww. C’mon, people. (Image)
HBV is spread through contact with infected blood or other bodily fluids with the most common modes of transmission being unprotected sex, contaminated needles or injection equipment, and from mother to child during childbirth. HAV on the other hand is typically spread through fecal matter contact being passed through food, water, or close personal contact.
The hepatitis vaccines are similar to the influenza vaccines in that the hepatitis A vaccines (Havrix™ and Vaqta™) contain inactivated HAV. The hepatitis B vaccines (Engerix-B™, Recombivax HB™, and Heplisav-B™) are recombinant vaccines containing genetic material from the HBV. For both HAV and HBV vaccines, our bodies use them to recognize and form antibodies against the viruses to prevent future illness.
In addition to the individual vaccines, there is also a combination hepatitis A/B vaccine called Twinrix™ to simplify vaccination. This vaccine contains a combination of the inactivated HAV as well as recombinant genetic material from the HBV.
The hepatitis A and B vaccines are recommended for adults who are at risk of infection, such as healthcare workers (what can we say, we handle all of the injection devices and bodily fluids), people who inject medications or illicit drugs, and those living or traveling to regions with a high rate of transmission of HAV or HBV. As much as we all love a good food-truck when we travel, we can never be too protected from contamination! (PSA, let’s all just thoroughly wash our hands. Please. Everyone.)
Vaccine Adverse Effects
The most common side effects seen with any of the vaccines above typically include injection site soreness or redness, mild fever, or headache. It’s important to counsel our patients that these side effects do NOT mean that the vaccine caused them to fall sick! Instead, I like to remind my patients that building protection takes ENERGY. Fatigue, soreness, and mild fever are all typically related to the immense amount of energy your body is spending building antibodies to protect you from illness!
To help with these side effects, patients can take over-the-counter pain relievers such as acetaminophen or ibuprofen. These symptoms typically only last 24-72 hours. If they are still experiencing side effects after that time, advise them to contact their practitioner for further guidance.
Should a patient report a vaccine side effect to you, the CDC and FDA operate the Vaccine Adverse Event Reporting System, or VAERS, which is an application to track reports of side effects after vaccination to monitor and identify any possible concerns for the public. Both you and your patient can report these side effects to VAERS to help us better understand and ensure the ongoing safety of our vaccines.
Vaccine Contraindications
Aside from the scenarios mentioned above, the main contraindication to receiving any of the above vaccines is an allergic reaction to either the vaccine itself or one of the vaccine components. It’s also best to advise any patients with a fever or current illness to wait until those symptoms subside to receive any vaccinations as their immune system may not be able to mount a sufficient response to the vaccine for protection.
Special populations, such as immunocompromised or pregnant patients, may also have specific vaccines to avoid, such as live vaccines. Refer to the vaccine-specific monograph and guidelines for contraindications related to these patients.
The tl;dr of Adult Vaccinations
In a world full of scary, evolving bugs and bacteria, you must ready your arsenal with any tools possible for your patients. By knowing your main adult immunizations, how they work, and who should get them, you can help to reduce the burden on the healthcare system while increasing your patients’ health and long-term quality of life. Because let’s be honest…what’s a worse quality of life than to be in bed with the flu, pneumonia, AND a shingles rash??
Thankfully, as of January 1st, 2023, all Advisory Committee on Immunization Practices (ACIP)-recommended immunizations are COMPLETELY covered by Medicare for our disabled or older patients. Most other insurance companies have followed suit covering most immunizations for adults entirely.
Be sure to follow your state’s immunization reporting requirements to ensure your patient’s health record stays updated for other practitioners, and also be sure to provide each patient with a Vaccine Information Statement (VIS) after administration to help address any questions. Should you ever get lost or scared (viruses and bacteria scare me, no judgment) double check the current CDC guidelines for which vaccine is in question.
Now, go forth and help fight the good infectious disease fight!